Abstract
Aims: Despite the results of recent randomised studies, the systematic use of aspiration techniques in ST-elevation myocardial infarction has not been included in the new guidelines. To date, there have been very few bench tests of the different systems and the aim of our study was to test two catheters on different models of arteries with thrombi at six and 12 hours.
Methods and results: The test apparatus consisted of 3 mm diameter glass tubes of 150 mm in length. The thrombi were left for either six or 12 hours and ten models of tubes were used: straight, with a single bend and with two bends. Two types of catheters were tested: the Export® aspiration catheter (EAC) and the Proxis® embolic protection system (PES). The main assessment criterion was total thrombectomy. Total thrombectomy was achieved in only 55.3% of the tests and no difference appeared between the two systems. Total thrombectomy was achieved more frequently with 6-hour thrombi than with 12-hour thrombi for the two techniques, 62.5% vs. 42.5% (p=0.018) and 67.5% vs. 48.7% (p=0.025) for EAC and PES catheter, respectively. In contrast, total thrombectomy was more frequent in straight tubes and in tubes with a single bend than in tubes with double bends, respectively for EAC (64% vs. 44.8%, p=0.028) and for PES (85.9% vs. 35.4%, p<0.001).
Conclusions: The use of thrombectomy in the invasive management of acute coronary syndromes is growing. Our work on a “laboratory bench” reveals important technical differences. In consequence, in clinical practice, we speculate that the catheter system must be chosen according to both the artery anatomy and the delay between chest pain and PCI.
Introduction
Primary angioplasty is the established treatment for recanalisation of coronary arteries during acute ST-segment elevation myocardial infarction (STEMI). Rapid restoration of Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow is closely associated with improved survival1,2. Despite the use of increasingly powerful anti-thrombotic and antiplatelet therapy, distal embolisation in patients treated with primary percutaneous coronary intervention (PCI) occurs in about 10% of patients and remains a serious problem3,4. Dislodgement of the thrombus leads to distal thromboembolisation which frequently results in diminished microcirculatory perfusion or microvascular obstruction, increased infarct size and reduced survival1-10. In addition to the pharmacological approaches, several thrombectomy devices have been investigated to reduce the risk of embolisation. In a recent study, Vlaar et al randomly assigned 1,071 patients to initial thromboaspiration (Export Medtronic (EM), Medtronic Inc., Minneapolis, MN, USA) with stenting or conventional primary PCI with the use of a balloon and stent. Cardiac death at one year was significantly lower in the thrombus aspiration group when compared with the conventional PCI group (respectively 3.6% vs. 6.7%; p=0.020)11. These data were further confirmed by three meta-analysis12-14. There are many thromboaspiration (TA) devices, with very different technical characteristics, and the interventional cardiologist has to make choices. Based on the clinical observation that efficacy of thrombectomy devices can be greatly modified by the anatomy of the artery and the age of the thrombus, we specifically designed a study to answer the interaction between these phenomena. Among these many devices, we compared the efficacy of the Export® catheter (Medtronic Inc., Minneapolis, MN, USA) (used in many clinical trials) and the Proxis® catheter (St. Jude Medical, Maple Grove, MN, USA) which is a novel system of combined proximal embolic protection and thrombus aspiration. This new device extracted debris before dilation in 75% of STEMI patients treated by primary PCI15,16. To date, there have been very few bench tests of the different systems and the aim of our study was to test these two catheters on different models of arteries and with thrombi of six and 12 hour duration.
Materials and methods
Samples of blood (10 cc) were taken from fasting healthy subjects who were not taking any medication and had specifically not taken aspirin or non-steroid anti-inflammatory drugs during the previous month. The untreated blood samples were put into 3 mm diameter glass tubes to create 30 mm long thrombi. The glass tubes used had different angulations in order to represent a wide sampling of the possible coronary anatomy encountered by the interventional cardiologists. Ten models of tubes were used and each tube was made in duplicate: a) straight tubes; b) tubes with a single bend at 30°, 60° and 90°, and c) tubes with two bends at 30°/30°, 60°/60°, 90°/90°,30°/60°, 30°/90°, 60°/90° (Figure 1).
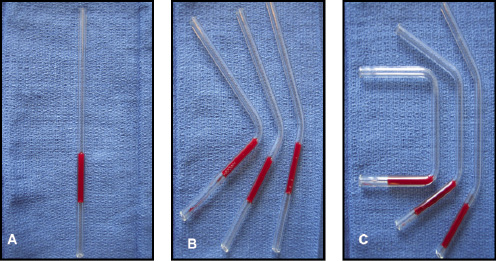
Figure 1. Photographs of tubes: (A) straight; (B) tubes with a single bend of 30°, 60° or 90°; (C) tubes with two bends 30°/30°, 60°/60° and 90°/90°.
Recent data coming from the pooled-analysis of Burzotta et al suggested that pharmacological and mechanical thrombus remodelling is important14. For this reason, our bench test used two different age thrombi (6-hour and 12-hour thrombi) that had formed at room temperature. Two types of catheters were tested: the Export® aspiration catheter (EAC) with a bevelled tip (Figure 2A), and the Proxis® embolic protection system (PES) (Figure 2B).
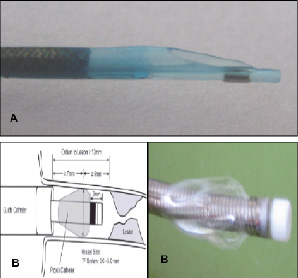
Figure 2. Photograph of the distal end of the Export® aspiration catheter (A) and Proxis® embolic protection system (B).
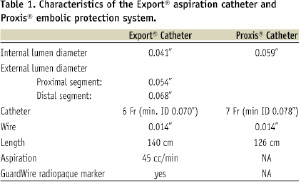
The characteristics of both systems are detailed in Table 1.
The aspiration system was controlled by a manual manometer (0-500 mbar) linked to an air-tight flask into which the thrombus was aspirated. The vacuum was constant and set at 200 mbar17. The catheter was connected to the aspiration system and the tip placed in direct contact with the thrombus by visual assessment. The catheters were tested in random order, and eight series of tests per device were performed for each model (6-hour or 12-hour thrombus). Finally, 160 tests per device were analysed. The device was inserted into each tube to allow aspiration of the thrombus (which was either complete or incomplete). Failure to remove the thrombus was defined if it took more than four attempts to remove it. The influence of the different combinations of bend and age of the thrombus were also tested, according to total thrombectomy and number of sequences of thromboaspiration needed to remove the whole thrombus.
The primary endpoint was the performance of each study device assessed by the complete aspiration of the thrombus into the flask. The number of sequences of thromboaspiration needed to assess a complete aspiration of the thrombus was the secondary endpoint, and this data was dichotomised in two groups according the number of sequence of thromboaspiration (1 or 2 sequences vs. ≥ 3).
The data were analysed using Sigma Stats software (Jandel Inc., Ashburn, VA, USA). The results are presented in the form of percentages for qualitative values. All the comparisons were performed by χ2 test. The threshold of significance was set at 5%, a p-value < 0.05 was considered significant. Since the variables for evaluating the number of sequence were not continuous, we dichotomised them into two categories: number of sequences of thromboaspiration < 3 and ≥ 3.
Results
Performance of the devices
The complete aspiration of the thrombus was achieved in only 55.3% of the tests. No difference was observed between the two devices when we compared the overall results (52.5% vs. 58.1%, p=0.368).
Impact of the age of the thrombus
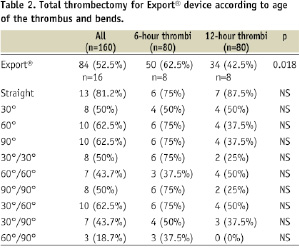
Total thrombectomy was achieved more frequently with 6-hour thrombus than with 12- hour thrombus (65% vs. 45.6%, p=0.012). For the Export® system, total thrombectomy was achieved in 52.5% of cases, and a significant difference was observed between 6-hour thrombus and 12-hour thrombus (62.5% vs. 42.5%, p=0.018) (Table 2).
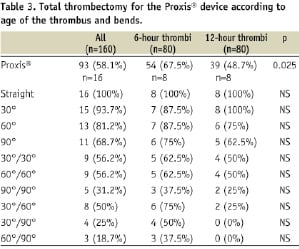
For the Proxis®, total thrombectomy was achieved in 58.1% of cases, and we found a significant difference between 6-hour thrombus and 12-hour thrombus (67.5% vs. 48.7%, p=0.025) (Table 3).
Impact of the bends and angles
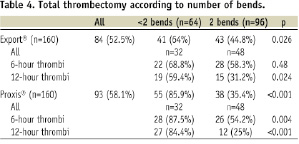
The rate of total thrombectomy decreased according to bends and angles, but no significant difference was observed for both devices (Tables 2 and 3). However, if we dichotomised our population according to the number of bends in the glass (0-1 bend vs. 2 bends) a significant difference was observed between the two groups, whatever the age of the thrombus (75% vs. 40.1%, p=0.004), (Figure 3).
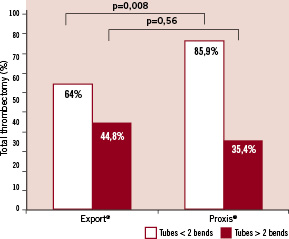
Figure 3. Total thrombectomy according to number of bends.
The Proxis® catheter is much more efficient in the model with 0-1 bend than the Export® device and that, for a 6-hour or 12-hour thrombus. This superiority disappears in the two bends models where the Proxis® catheter seems to be less efficient than the Export®, especially in old thrombus (Table 4).
Number of sequences of thromboaspiration
No significant difference was observed in the frequency of ≥ 3 attempts between the two devices, whatever the age of thrombus or angulations (75.6% vs. 70.6%, p=0.45). For the EAC, a number of attempts ≥ 3 was significantly more frequent for tubes with two bends than for straight or 1-bend tubes (88.5% vs. 56.2%, p<0.001) (Table 5).
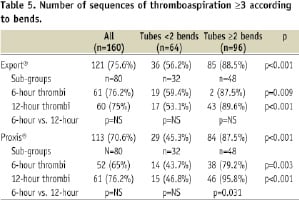
This difference remained significant, whatever the age of the thrombus (87.5% vs. 59.4%, p=0.009 for 6-hour thrombus and 89.6% vs. 53.1%, p <0.001 for 12-hour thrombus respectively) (Table 5). For the PES, a number of attempts ≥ 3 was significantly more frequent for tubes with two bends than for straight or 1-bend tubes, and this difference also remained significant, whatever the age of the thrombus (Table 5).
Discussion
Our work is the first to test the impact of various bend angles and age of the thrombus and the efficacy on two thrombectomy devices. Global results do not show a difference between the devices with an average rate of total aspiration of the thrombus of 55%. But we show a different efficacy of each device according to the coronary model in the test. The Proxis® catheter is more efficient than the Export® catheter in the model with 0-1 bend and with a 6-hour or 12-hour thrombus. But this advantage is less clear in the two bends models, and especially in old thrombus.
Impact of coronary anatomy and age of the thrombus
To the best of our knowledge, these two parameters have never been tested in the setting of the thrombectomy device on a bench test. However, interventional cardiologists are aware of the great differences raised by the previous parameters on the efficacy of their aspiration procedure. First, the different angulations had a significant impact on the efficacy of thrombus aspiration devices. We did not test the flexibility and the difficulty of crossing in the present work, but these data are very relevant in clinical practice for the interventionist who must choose a device according to the anatomy of the coronary tree. Our data first addressed this issue and by showing a different pattern according to the vessel tortuosity, it can give some clue to the best choice in the context of a clinical application. Furthermore, the impact of the age of the thrombus on the efficacy of the two thromboaspiration devices studied is clearly in relation to the histopathological characteristics and size18. The initial thrombus is predominantly composed of platelets, but changes very rapidly and erythrocytes are deposited over the platelet thrombus in the stagnant blood. It then becomes organised with time, more compact and adherent to the walls, and therefore more difficult to aspirate. In our study, we found a significant difference between the two devices to reach the main assessment criterion (total thrombectomy) regarding the time delay of clotting (p=0.018 for Export® and p=0.025 for Proxis®). However, we did not find any difference on the secondary criterion. This last information was not found with Rioufol’s study and seems to be related to the use of angled glass tubes17. Finally, few clinical studies have assessed the performance of the TA devices on totally removing the thrombus. Data on collected aspirated thrombi are not widely reported. Thus, in the TAPAS study, the aspirated thrombi were collected in 73% of cases, with large differences depending on the artery (68.7% for the LAD, 65.3% for the LCX and 81.9% for the RCA)19.
From the bench test to the patient
In a recent meta-analysis, Bavry and colleagues12 reported that the impact on mortality of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction varied widely according to the type of device. However, no data are available to explain such differences. The concept of the bench test gives the opportunity to address specific issues. Sakurada et al compared the aspiration, the easy of positioning, and lateral-branch accessibility of a new design of thrombus vacuum catheter with those of two branded systems (Percusurge and Rescue). They used a 1.4 mm diameter gelatine cylinder to mimic the behaviour of thrombi20. However, the chosen diameter was smaller than that of epicardic arteries, which are generally treated by PCI (even more so for TA)21,22. Moreover, the biochemical properties of gelatine do not correspond to those of thrombi, which are the result of a dynamic process23 and probably do not offer the same mechanical resistance. These choices are thus limited to the clinical relevance of the results. By using 3 mm diameter thrombi created in vitro we created conditions that are closer to those found in clinical practice23. The methodology used for the present study was previously described by Rioufol and colleagues17, and in agreement with their results we used a constant aspiration pressure with the two devices although we had important technical differences. Furthermore, in our model, we conducted our tests using tubes occluded by the thrombus; this point is crucial because in the majority of clinical trials treating this topic, patients included have a baseline TIMI flow 0 or 1 or a visible thrombus. Of the two devices used in this study, the Export® Catheter, produced since 2001, has been used to remove embolic debris in more than 250,000 patients worldwide; recent evolution and upgrades have led to improved deliverability, reduced vessel trauma and improved debris capture, plus a hydrophilic coating for greater lubricity. The Proxis® catheter has the ability to aspirate during the PCI procedure and also provides protection of the side branches. This is the first and only system to provide both, embolic protection before wire crossing of the thrombotic coronary occlusion and thromboaspiration. More recently effectiveness and safety has been assessed in patients24, and the device was tested in STEMI patients in the PREPARE trial15,16. Despite an aspiration rate of 75%, the study failed to show a difference in the ST-segment resolution, as well as on infarct size or left ventricular ejection fraction as measured by CMR. The aspiration rate could be improved by technical progress and by better analysis of the initial angiographic data, which should also identify patients likely to respond well to the technique. The number and quality of aspiration procedures could thus be optimised especially regarding basic information such as coronary anatomy.
Conclusion
Thromboaspiration is a promising technique in the treatment of atherothrombosis25-29. Various devices are available but selection must be based on efficacy. Our study is the first to highlight the interaction between age of the thrombus, the anatomy of the coronary tree and the quality of the thrombectomy, and thus contributes towards a better understanding of the complexities of performing total thrombectomy. This work will help clinicians in their choice of catheter especially when the thrombus is located in a tortuous coronary artery. Finally, the study emphasises the need to rationalise the thromboaspiration procedure and to identify the population that would most benefit from this therapy.
Acknowledgements
This work was supported by the Association de Cardiologie de Bourgogne, The University Hospital, Dijon, France and by grants from Union Régionale des Caisses d’Assurance Maladie de Bourgogne (URCAM), and Agence Régionale de l’Hospitalisation (ARH) de Bourgogne. We wish to thank Anne Cécile Lagrost and Juliane Berchoud for research assistance and Philip Bastable for assistance with translation. (English assistance).

