Abstract
Aims: Percutaneous treatment of coronary chronic total occlusion (CTO) is associated with important arterial remodelling after successful recanalisation. Bioresorbable vascular scaffold (BVS) implantation in CTO has been shown to be feasible and can be of interest when the scaffold achieves complete bioresorption. We sought to evaluate the three-year results in terms of clinical events, serial imaging outcomes and vasomotion response in CTO lesions successfully treated with BVS.
Methods and results: A total of 33 patients (35 CTO lesions) successfully treated with BVS were included in the ABSORB-CTO study. Clinical outcomes, quantitative coronary angiography (QCA) and optical coherence tomography (OCT) assessment were analysed at one- and three-year follow-up. Vasomotion examination was also performed at three years. At three years, cumulative target vessel reocclusion was observed in four lesions (11.4%). By QCA, the in-scaffold segment presented a lumen loss of 0.23±0.46 mm compared with the baseline procedure (p=0.001) and a lumen gain of 0.05±0.29 mm between one and three years (p=0.220). By OCT, the mean neointimal area stenosis progressed from 11.45% at 12 months to 17.10% at 36 months (p<0.001) and mean scaffold area increased continuously at 12 (+12%; p<0.001) and at 36 months (+14.85%; p=0.001). Late acquired incomplete scaffold apposition (LAISA) observed at 12 months in three patients was completely undetectable at three years. Most cases responded to endothelium-dependent vasomotor stimuli (69%). Vasoconstriction to acetylcholine was the predominant response (45%).
Conclusions: Successful recanalisation of coronary CTO with BVS implantation is associated with favourable clinical and imaging outcomes. Despite vessel motility restoration, successfully treated CTOs remain with signs of endothelial dysfunction.
Abbreviations
| ACh | acetylcholine |
| ADR | anterograde dissection and re-entry |
| AWE | anterograde wire escalation |
| BVS | bioresorbable vascular scaffold |
| CTO | chronic total occlusion |
| DES | drug-eluting stent |
| DS | diameter stenosis |
| ISA | incomplete scaffold apposition |
| IVUS | intravascular ultrasound |
| LAISA | late acquired incomplete scaffold apposition |
| LLL | late lumen loss |
| LVEF | left ventricular ejection fraction |
| MaxLA | maximal lumen area |
| MaxLD | maximal lumen diameter |
| MaxSA | maximal scaffold area |
| MeanLA | mean lumen area |
| MeanLD | mean lumen diameter |
| MSCT | multislice computed tomography |
| TLF | target lesion failure |
Introduction
Implantation of bioresorbable vascular scaffolds (BVS) has proven to be an appropriate treatment option in several types of non-complex coronary lesion1,2. In the setting of chronic total occlusion (CTO), a few studies have shown encouraging results at one-year follow-up, with a low rate of target lesion failure (TLF) (5%)3,4 and scaffold reocclusion5,6. However, there is a lack of information regarding the long-term follow-up outcomes in patients with CTO treated with BVS. Moreover, several questions regarding the potential advantages of BVS over traditional metallic stents remain unsolved, such as the late lumen gain, long-term vessel remodelling, the fate of malapposed struts and the restoration of vasomotion in the scaffolded and distal coronary segments.
The present study evaluated the three-year follow-up results in terms of clinical events, serial imaging outcomes in-scaffold and in the distal vessel using optical coherence tomography (OCT), and the vasomotor response when BVS resorption is almost complete.
Methods
POPULATION AND STUDY DESIGN
The design, post-procedural and one-year follow-up results of the ABSORB-CTO study have been published previously5,7. Briefly, between February 2013 and March 2014, 33 patients with 35 CTO coronary lesions (EuroCTO definition)8 with reference vessel diameters between 2.5 and 3.5 mm were included in the study. The Research Ethics Board approved the study and written informed consent was obtained from all patients.
PROCEDURAL PROTOCOL DURING PERCUTANEOUS CORONARY INTERVENTION
Percutaneous coronary intervention (PCI) was performed following a strict protocol7. After CTO recanalisation with the guidewire, dilatations with undersized balloons (1.5 to 2.0 mm) were performed in order to restore coronary flow. Intravascular ultrasound (IVUS) was performed to evaluate the lesion length and reference vessel diameters, and to characterise the plaque morphology in order to guide PCI. Accordingly, non-compliant balloons, cutting balloons or rotational atherectomy were used to achieve optimal lesion preparation under IVUS guidance. BVS implantation was performed following the manufacturer’s instructions for use. After BVS implantation (Absorb™; Abbott Vascular, Santa Clara, CA, USA), expansion and apposition were analysed by OCT. Post-dilatation with non-compliant balloons 0.5 mm larger than the BVS was performed, when needed, to obtain an optimal result that was again verified by OCT.
Patients were discharged on dual antiplatelet therapy for a minimum of 12 months.
CLINICAL OUTCOMES AND FOLLOW-UP PROCEDURES
Clinical follow-up was scheduled at 6, 12, 24 and 36 months. Moreover, as per protocol, multislice computed tomography (MSCT) was performed at six-month follow-up5. Angiographic follow-up with OCT analysis was performed at one and three years post procedure. Vasomotor examination in relation to endothelium-dependent and independent drugs was carried out at three years.
QUANTITATIVE CORONARY ANGIOGRAPHY
In each patient, the treated segment, the 5 mm peri-scaffold segments, and the >5 mm distal segment were analysed by quantitative coronary angiography (QCA) in matched angiographic views after the procedure and at one- and three-year follow-up (Figure 1). QCA analysis was performed by an independent core laboratory (Barcelona Cardiac Imaging Core-Lab [BARCICORE-Lab]). Late lumen loss (LLL) or gain was defined as the difference between minimal lumen diameter values in the follow-up and post procedure, after nitrate administration2. More detailed information on the QCA methodology has been described previously5.
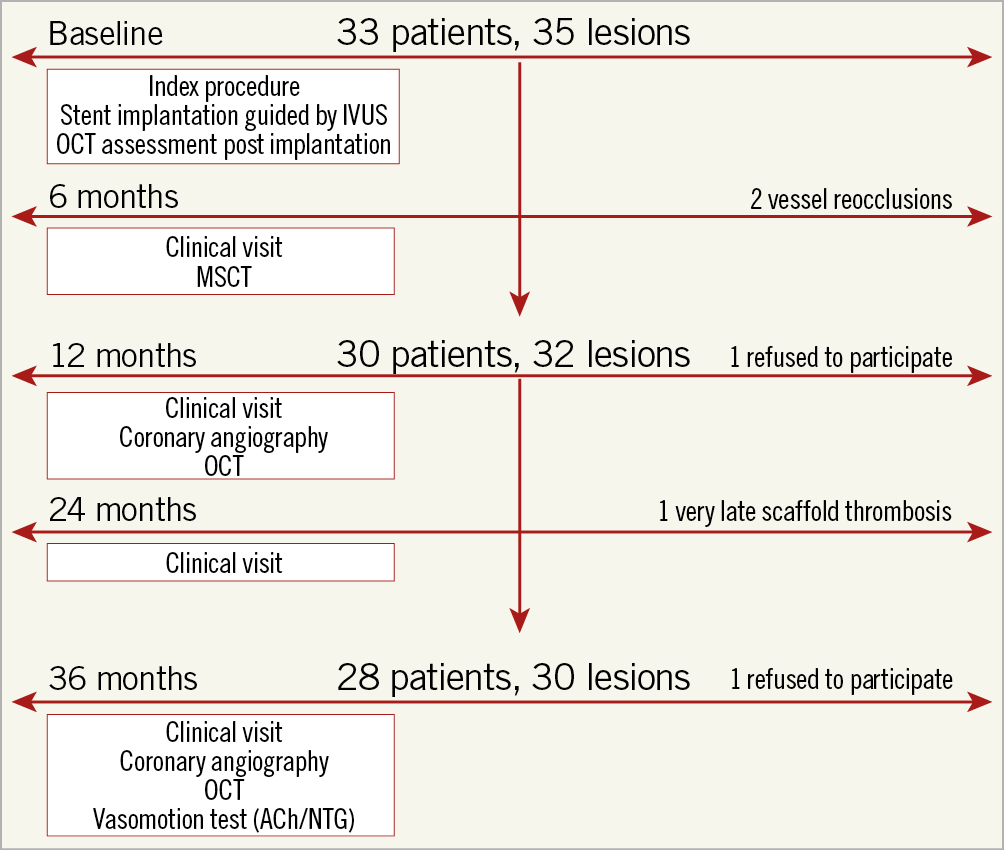
Figure 1. Study flow chart. ACh: acetylcholine; IVUS: intravascular ultrasound; MSCT: multislice computed tomography; NTG: nitroglycerine; OCT: optical coherence tomography
OCT ANALYSIS
OCT analysis was performed using dedicated software (C7XR™ System; St. Jude Medical, St. Paul, MN, USA) by an independent core laboratory (BARCICORE-Lab). More detailed information and definitions have been described previously5,9.
VASOMOTOR TONE ANALYSIS
A vasomotor test was performed after control angiography followed by OCT imaging. The protocol is extensively described in Supplementary Appendix 1.
Vasoconstriction or vasodilation was defined as at least a 3% change in the mean lumen diameter after infusion of the maximal dose of ACh or nitrates1,2,9,10.
STUDY DEFINITIONS
The primary endpoint was target lesion failure, defined as a composite of cardiac death, target vessel myocardial infarction and clinically driven target lesion revascularisation. Secondary endpoints included each individual endpoint of the primary endpoint as well as all-cause mortality and in-scaffold reocclusion. All endpoints were defined according to the Academic Research Consortium (ARC) definitions on stent trials11.
STATISTICAL ANALYSIS
Continuous variables are described as mean±standard deviation (SD) or as median and interquartile range, as appropriate. The Student’s t-test for paired data was used to compare means at different time periods for each patient. Categorical variables are expressed as counts (percentage) and were compared with the use of Pearson’s chi-square test or Fisher’s exact test, as appropriate. P-values of less than 0.05 were considered to indicate statistical significance. All statistical analyses were performed using SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
STUDY FLOW CHART
Thirty-three patients (35 CTO lesions) were prospectively included in the ABSORB-CTO study, with a procedural success rate of 100% (final in-scaffold residual stenosis <30% and TIMI flow 3 in the target vessel). The MSCT imaging control at six months showed lesion reocclusion in two patients. Moreover, two patients refused catheterisation at 12 and 36 months, respectively; one patient presented scaffold thrombosis at 24 months and did not undergo the 36-month coronary angiography. Therefore, 28 patients (30 lesions) underwent coronary angiography at three years. One patient with a patent artery at 12 months presented with asymptomatic vessel reocclusion at three years. This patient did not undergo intravascular imaging or a vasomotion test. In one patient, OCT could not be performed due to technical issues. Figure 1 shows the study flow chart.
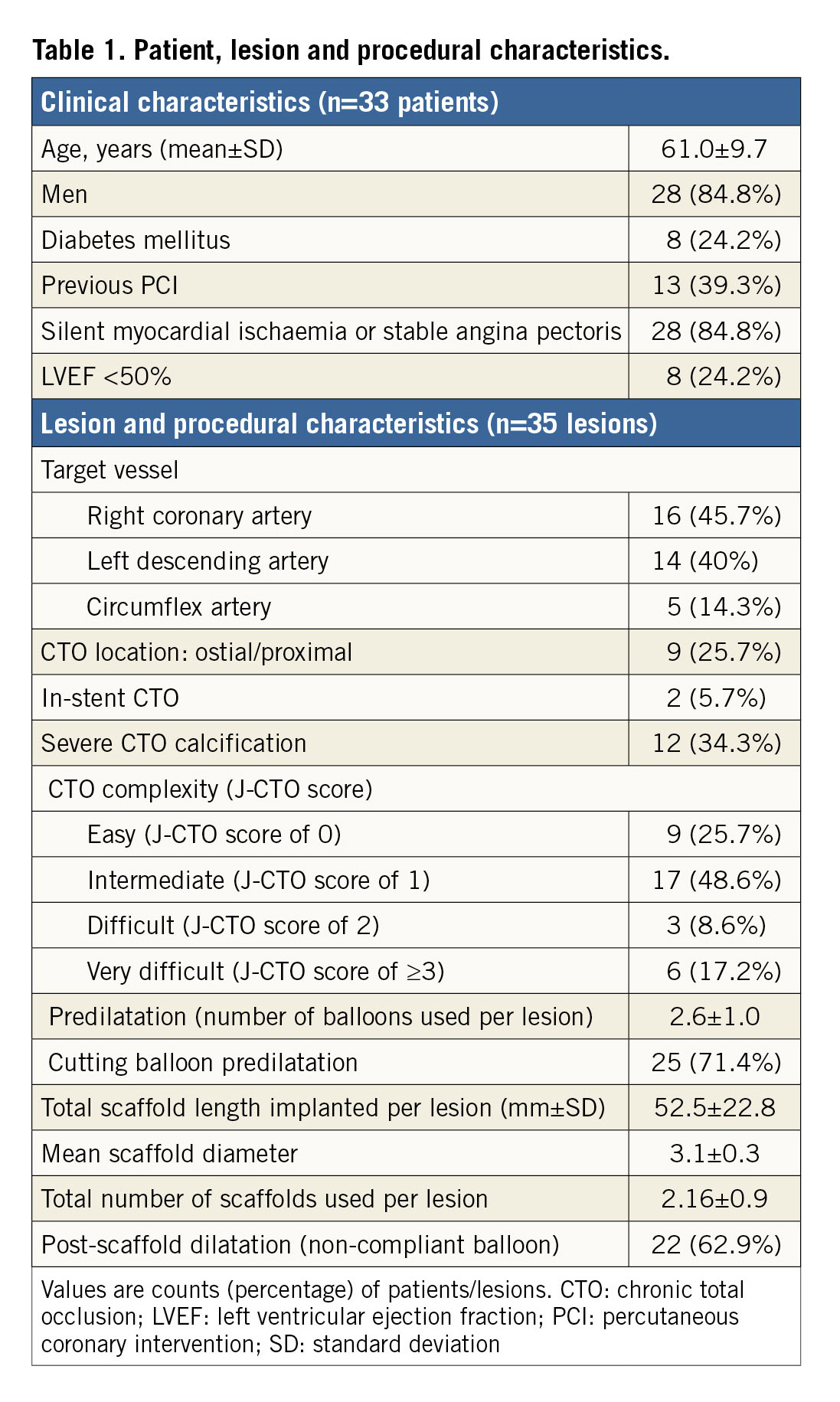
PATIENT AND PROCEDURAL CHARACTERISTICS
Patient data, lesion and procedural characteristics are summarised in Table 1. Mean age was 61.0±9.7 years and the clinical presentation was stable angina in 84.8% (n=28) of patients. Lesion complexity was graded as difficult or very difficult in 25.8% (n=9) of cases according to J-CTO score. IVUS-guided plaque preparation was performed in all cases, using a cutting balloon in most cases. Mean implanted scaffold length was 52.5±22.8 mm per lesion. After OCT analysis, post-dilatation with a non-compliant balloon was required in 62.9% (n=22) of lesions.
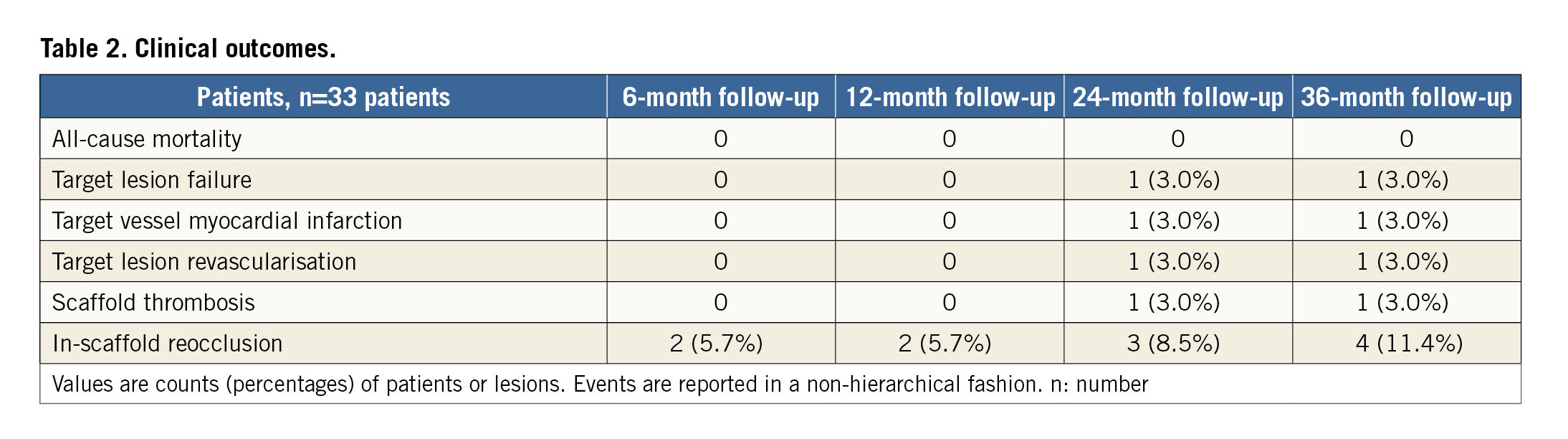
CLINICAL OUTCOMES
Three-year follow-up was completed in all patients and is shown in Table 2. No clinical events were observed during the first 12 months. At 24 months, one patient presented a non-Q-wave myocardial infarction. Coronary angiography revealed very late scaffold thrombosis that was subsequently treated with thrombectomy and DES implantation. No other clinical events were observed during the course of the study.
ANGIOGRAPHIC RESULTS
Complete angiographic follow-up was performed in 81.8% (n=27) of patients, with 29 lesions analysed at different time points. Table 3 summarises the results of QCA data.
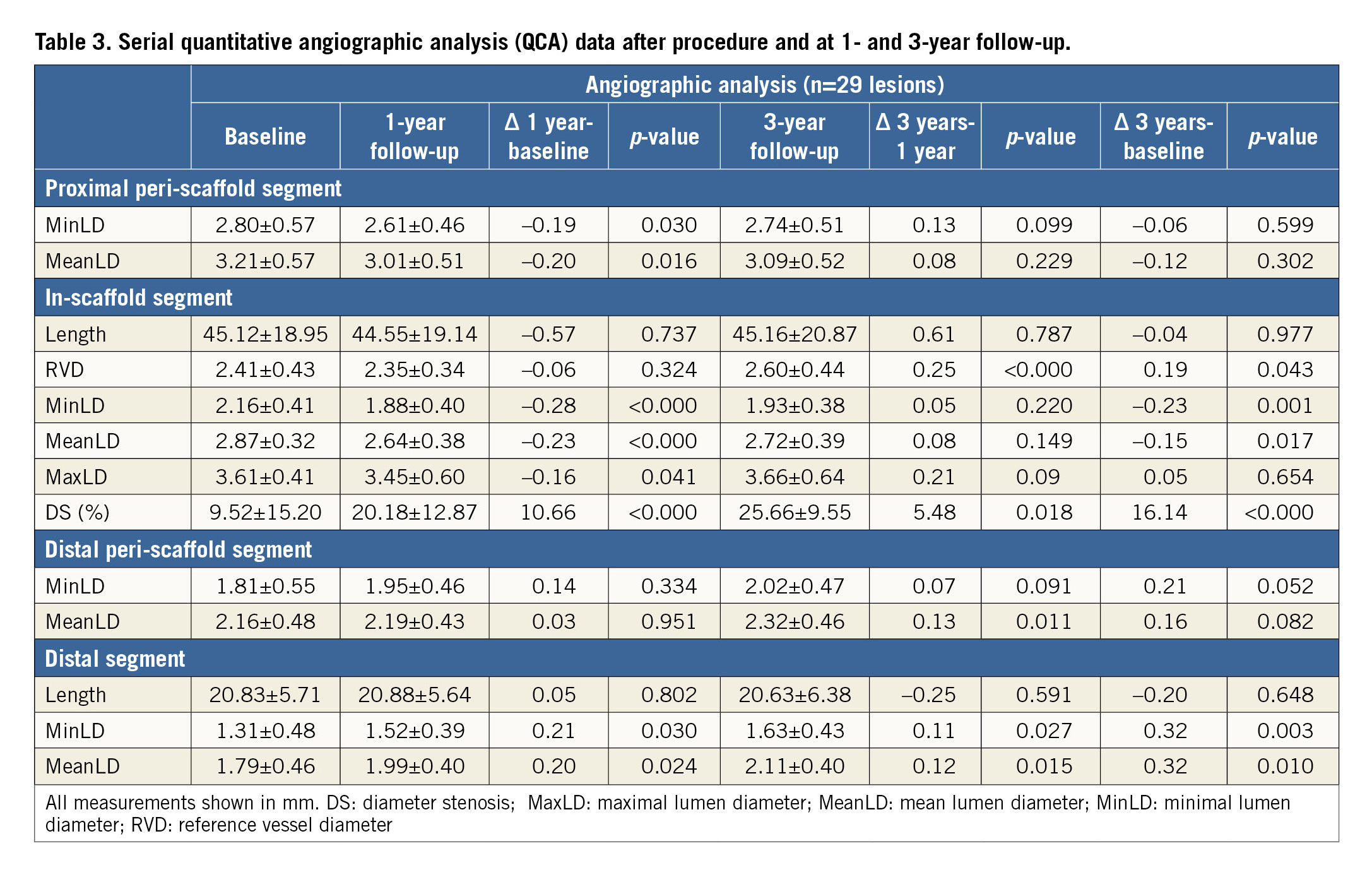
At 12 months, all lumen diameters were significantly smaller than the corresponding dimensions obtained immediately post implantation. The one-year in-scaffold lumen loss was 0.28±0.33 mm. However, all lumen diameters presented a trend towards an increase from 12-month to 36-month follow-up. At 36 months, the in-scaffold lumen loss was 0.23±0.46 mm. Diameter stenosis increased progressively both at 12 months (20.18±12.87%; p<0.001) and at 36 months (25.66±9.55%; p<0.001).
Distal segments >5 mm presented a continuous lumen enlargement with minimal and mean lumen diameter increases of 25% (1.31 vs. 1.63 mm, p=0.003) and 18% (1.79 vs. 2.11 mm, p=0.01) at 36 months, respectively, as compared to baseline.
OCT ANALYSIS
Complete serial OCT analysis was obtained in 78.8% (n=26) of patients, with 28 matched segments explored at baseline, 12 and 36 months. Quantitative OCT data are shown in Supplementary Table 1. Mean neointimal area stenosis progressed from 11.45% at 12 months to 17.10% at 36 months (p<0.001), but mean scaffold area increased by 12% at 12 months (Δ=0.79 mm2; p<0.001) and 15% at 36 months (Δ=0.98 mm2; p=0.001). The mean and minimal lumen areas decreased at 12 months (Δ=-0.88 mm2, 11%, p=0.001, and Δ=-1.33 mm2, 25%, p<0.001, respectively), but were maintained at 36 months (Figure 2). Finally, mean incomplete scaffold apposition (ISA) increased from 0.80 mm2 immediately post procedure to 1.31 mm2 at 12 months.
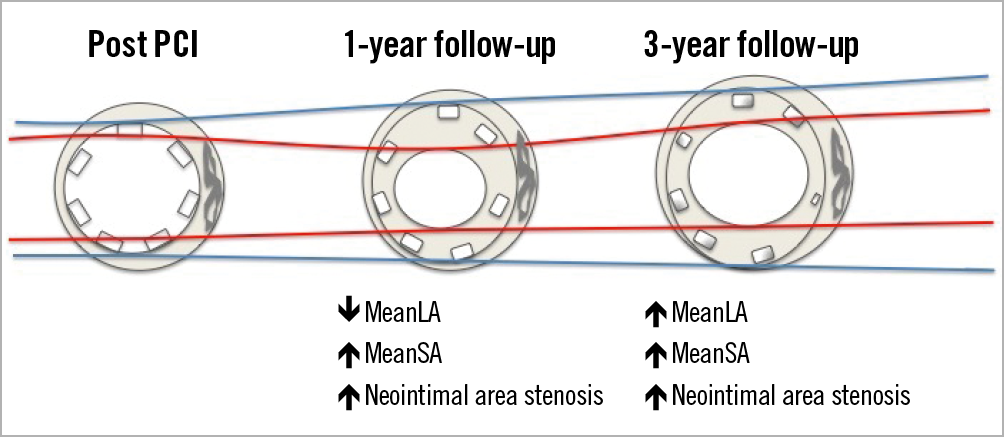
Figure 2. Evolution of the mean stent area and mean lumen area during follow-up. Red lines delimit mean lumen area. Blue lines delimit mean scaffold area. PCI: percutaneous coronary intervention
All qualitative OCT data are detailed in Supplementary Table 2. Three patients presented late acquired incomplete scaffold apposition (LAISA) at 12-month follow-up. The malapposition length occupied 18.6% of the BVS total length (31/166 mm) with a mean incomplete scaffold apposition area of 4.8 mm2. All three patients had no signs of malapposition at three years due to the complete disappearance of malapposed struts (Figure 3).
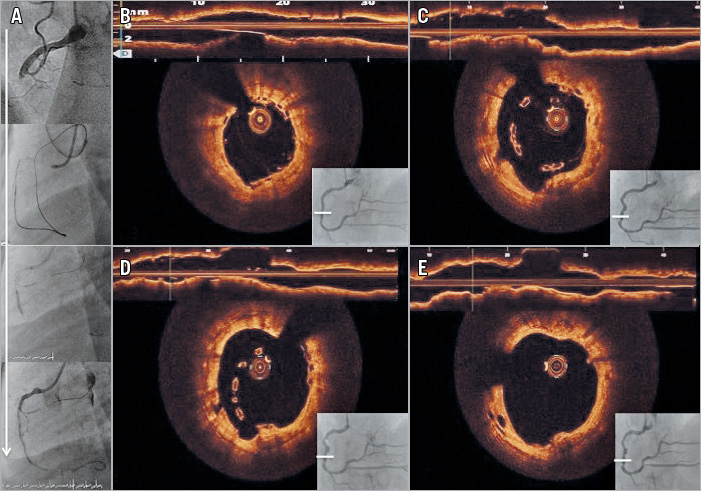
Figure 3. Representative case of LAISA after a CTO intervention. A) Mid right coronary artery CTO with successful retrograde dissection re-entry technique, with implantation of 3 BVS. B) Final result of both angiographic and OCT assessment. C) 12-month follow-up, positive vessel remodelling with severe LAISA. D) 24-month follow-up, persistent LAISA. E) 36-month follow-up, LAISA resolution after BVS resorption. White lines correspond to malapposed segment. BVS: bioresorbable vascular scaffold; CTO: chronic total occlusion; LAISA: late acquired incomplete scaffold apposition; OCT: optical coherence tomography
VASOMOTOR TONE ANALYSIS
A vasomotion test was performed in 27 patients (29 lesions). Both stented segments and distal non-treated segments responded to vasomotor stimuli (69.0%). Paradoxical vasoconstriction to ACh was the predominant response (45%). Vasodilatation to ACh occurred in 24% of cases. When nitroglycerine (NTG) was administered, vasodilatation occurred in almost half of the cases (Figure 4).
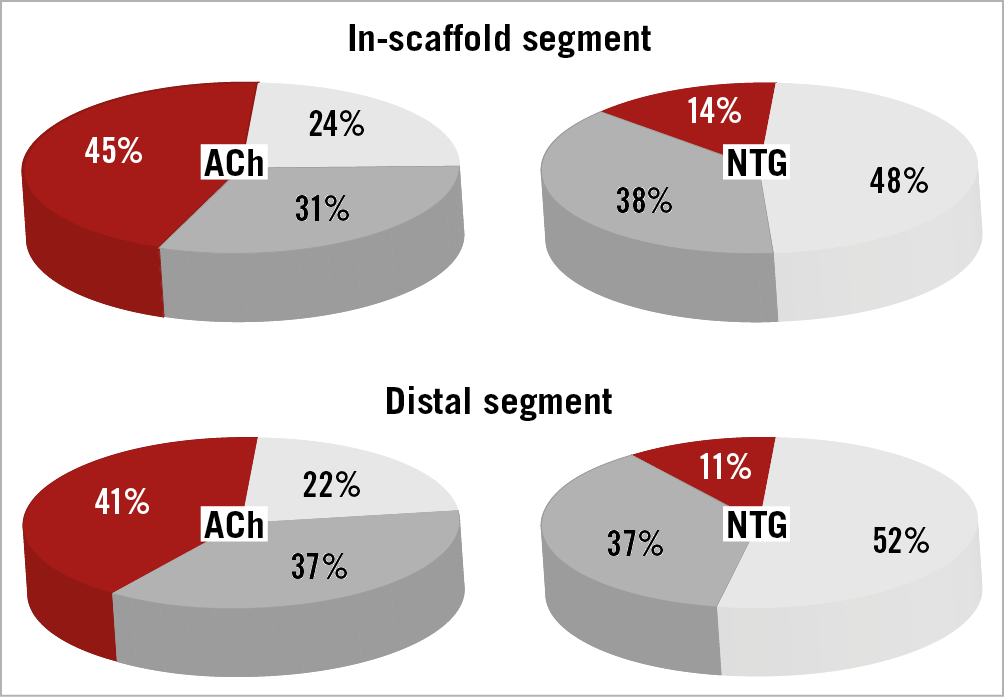
Figure 4. Vasomotion responses to acetylcholine and nitroglycerine in-scaffold and in distal segments. The percentage of the segments that responded to maximal doses of ACh or NTG with vasodilation (light grey), with vasoconstriction (red) or without significant change (grey) in the lumen diameter. ACh: acetylcholine; NTG: nitroglycerine
Mean lumen diameters in-scaffold and in distal segments decreased slightly after maximal doses of ACh; however, after NTG administration, they increased significantly (p<0.05) (Supplementary Figure 1).
Discussion
To the best of our knowledge, the ABSORB-CTO study is the first reporting clinical outcomes, serial multimodality imaging (angiography, OCT) and coronary vasomotor assessment of patients with CTO lesions treated with BVS at three-year follow-up. The main findings of the present study are: (1) patients with CTO treated with BVS presented favourable outcomes with target lesion failure of 3% and an asymptomatic reocclusion rate of 8.5% at three-year follow-up; (2) lumen dimensions of the in-scaffold segment showed a significant reduction by QCA and OCT analysis from baseline to 12 months, but were maintained from 12 months to 36 months; (3) there was a significant increase of the scaffold diameters from 12 to 36 months, indicating a possible positive vessel remodelling; (4) LAISA, detected by OCT in 9% of the cases, resolved during long-term follow-up due to resorption of malapposed struts; and (5) although OCT imaging showed BVS remnant material at three years, 70% of the lesions responded to vasomotor stimuli.
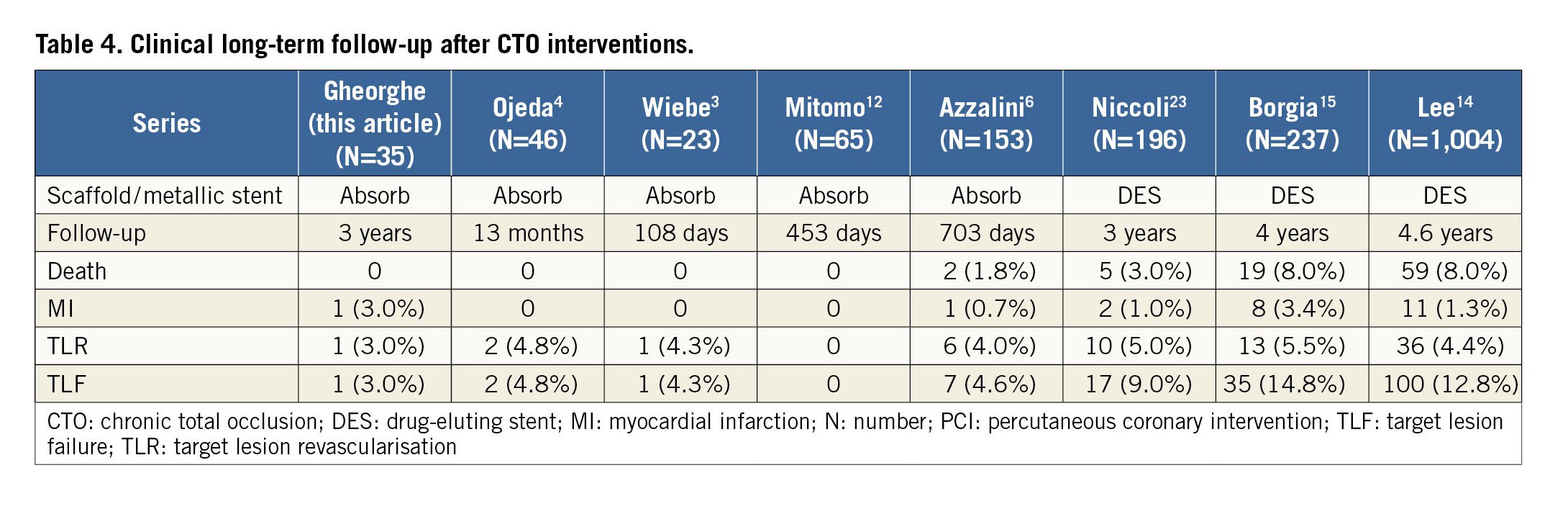
Clinical outcomes of patients with CTO treated with BVS have been reported previously in a few studies3,4,5,6,12,13. Unfortunately, long-term follow-up data (3 years) are only available with non-bioresorbable stents14,15 (Table 4). The three-year cumulative reocclusion rate of the present study is 11.4% (including one symptomatic very late scaffold thrombosis and three asymptomatic reocclusions).
Although interest in CTO revascularisation has increased exponentially, the “real” incidence of asymptomatic restenosis and reocclusion is still unknown at long-term follow-up in the absence of systematic angiographic or MSCT imaging follow-up.
Despite the limited data, it is difficult to conclude that the Absorb BVS is prone to asymptomatic reocclusion. Ojeda et al reported a reocclusion rate of 6.5% after CTO treated with BVS at six-month follow-up as defined by MSCT4. On the other hand, the reocclusion rate in a large CTO series (n=172 patients) treated with sirolimus-eluting stents was 16.8% at 12-month follow-up16, and another study including 117 CTO lesions treated with DES using only the anterograde approach showed a 9.9% reocclusion rate at 12- to 18-month follow-up17. Therefore, it seems that the reocclusion rate in CTO lesions treated with metallic stents is similar to that observed in the present study.
The mechanism of in-stent reocclusion/thrombosis is unclear, but fragmented internal elastic lamina and disruption of the media seen at the proximal fibrous cap at the entrance of the CTO, as well as prominent macrophage infiltration, can promote this phenomenon15. The angiographic and intravascular imaging of the patient presenting with very late scaffold thrombosis at 24 months is shown in Supplementary Figure 2. The intravascular imaging performed during the baseline procedure showed subintimal dissection in the proximal cap of the CTO, attributed to the subintimal position of the retrograde wire. At one-year follow-up, full strut coverage with macrophage-rich neointimal tissue and residual malapposition were detected by OCT. Inflammatory tissue and malapposition were probably associated with scaffold thrombosis, although the patient continued on dual antiplatelet therapy.
Although post-dilatation was performed in only 63% of the cases (only when needed), all the cases with reocclusion had benefited from post-dilatation with NC balloons. Two of these patients were treated with a 2.5 mm diameter scaffold (circumflex artery, without acute malapposition) and presented with asymptomatic reocclusions at six months, as assessed by CT scan. The patient with asymptomatic late reocclusion seen at 36 months had a right coronary artery CTO, treated with four BVS (from ostium to distal segment). Traumatic engagement of the guiding catheter with several strut fractures in the proximal segment during 12-month angiographic control could have played a role in this event.
The ABSORB II study2 reported the angiographic results at three-year follow-up in non-CTO lesions treated with BVS, showing an LLL of 0.37 mm. Our study presented an LLL of 0.28 mm at one year but, due to the positive remodelling, LLL was 0.23 mm at three-year follow-up. Similar findings were observed in initial studies with BVS, but had not been previously reported in the setting of complex lesions such as CTOs18. Positive remodelling of coronary CTO arteries has been observed after successful recanalisation in distal coronary segments17. The present study also noticed a positive lumen remodelling of the distal segments at three years (mean lumen diameter enlargement >18%).
There are no previous data regarding OCT control during long-term follow-up in CTOs treated with BVS. The changes of mean lumen area (MeanLA) and mean scaffold area (MeanSA) in our study followed the same pattern as those described in the ABSORB cohort A: a reduction of MeanLA was observed at one year, with later enlargement at three years and progressive MeanSA increase both at one-year and at three-year follow-up.
LAISA is a frequent phenomenon after CTO treatment with metallic stents. It may be caused by an excessive vessel enlargement due to mechanical injury during aggressive plaque modification or subintimal wire tracking and it is associated with stent thrombosis. In our study, LAISA was observed in three cases at one-year follow-up. Dual antiplatelet therapy was continued in all patients and this issue was resolved once the scaffold resorption occurred, highlighting the potential advantage of BVS over metallic or non-resorbable stents (Figure 3).
Endothelial dysfunction has been associated with atherosclerotic disease progression and cardiovascular events both in patients without angiographic coronary stenosis and in patients treated with stent implantation19,20.
CTO lesions are the worst scenarios of coronary atherosclerotic disease and endothelial dysfunction is present not only in the CTO segment, but also in the distal segment. Galassi et al21 showed that the distal vessel continues to have a certain degree of endothelial dysfunction after CTO revascularisation.
The hypothesis of vasomotility restoration after BVS implantation has been tested with several drug stimuli and in different clinical settings or stages of BVS resorption. For example, in “non-complex lesions”, the ABSORB II study showed no significant diameter increase of BVS after NTG administration at 36 months compared with everolimus-eluting metallic stents2. However, several studies have shown certain vasomotion response to ACh in different clinical settings22. In accordance with these studies, and by the time of almost complete BVS resorption, our study showed that endothelium-dependent vasomotility recovered in almost 70% of cases, although with vasoconstriction as the predominant response.
These findings suggest that, despite motility restoration, endothelial dysfunction usually remains both in the in-scaffold segment and in the distal vessel. A representative case is presented in Supplementary Figure 3.
Due to the small sample size, our study could not establish a relationship between subintimal dissection, vessel calcification and endothelial dysfunction. Nevertheless, anterograde wire escalation (AWE) was performed in 85% of the cases, where subintimal stenting was unusual.
Although the radial strength of the device is no longer present at three years, it is plausible that a certain degree of inflammation to remnant material may be prone to a larger degree of endothelial dysfunction than in later bioresoprtion phases with no visible struts, as assessed by OCT.
Limitations
The present study has several limitations. First, the device used in the study (Absorb; Abbott Vascular) is no longer available for commercial use and the number of patients included is small. Therefore, all results presented in this study should be considered as exploratory and hypothesis-generating. Second, there were several cases with a large number of indiscernible struts due to their advanced bioresorption state as assessed by OCT. This makes it difficult to assess the scaffold area in those cross-sections. Finally, vasomotion assessment can be altered by the presence of struts, as assessed by OCT, at three years.
Conclusions
Our study suggests that BVS implantation in CTO lesions may have favourable clinical outcomes at long-term follow-up. The LAISA frequently observed in CTO lesions can be resolved with this novel technology when the scaffold disappears completely. Moreover, despite restoration of vessel motility in successfully treated CTO at three years, endothelial dysfunction persists in the context of remnant intravascular material. Larger studies with longer follow-up are needed to confirm the potential advantages of BVS over DES, such as malapposition resolution or endothelial function restoration in these complex lesions.
|
Impact on daily practice The present study showed favourable clinical and imaging outcomes at long-term follow-up after CTO interventions treated with BVS. In addition, this study suggests potential advantages of using bioresorbable stents, such as LAISA resolution or vasomotion restoration. The safety and efficacy of BVS implantation in CTO lesions at long-term follow-up should be confirmed in further investigations. |
Funding
L. Gheorghe has received a grant from the Catalan Society of Cardiology.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix 1. Vasomotion tone analysis.
Supplementary Figure 1. Changes in mean lumen diameter in-scaffold and in distal segment after acetylcholine and nitroglycerine administration.
Supplementary Figure 2. Very late scaffold thrombosis.
Supplementary Figure 3. Representative case of vasomotion response to acetylcholine and nitroglycerine.
Supplementary Table 1. Serial quantitative optical coherence tomography (OCT) data after the procedure and at 1- and 3-year follow-up.
Supplementary Table 2. Serial qualitative optical coherence tomography data.