Abstract
Aims: To establish success and complication rates of excimer laser coronary atherectomy (ELCA) in a contemporary series of patients with balloon failure during percutaneous coronary intervention (PCI) of both chronic total occlusions (CTO) and lesions with distal TIMI 3 flow.
Methods and results: We identified 58 cases of balloon failure treated with ELCA±rotational atherectomy (RA) over four years, representing 0.84% of all PCI performed in our centre during this period. Balloon failures were classified according to: (i) mechanism of balloon failure; and (ii) whether this occurred in the context of treating a CTO. ELCA was performed following balloon failure using the CVX-300 Excimer Laser System and a 0.9 mm catheter with saline flush. For the entire cohort, procedure success was achieved in 91% (with ELCA successful: alone in 76.1%, after RA failure in 6.8% and in combination with RA for 8.6%). Only in one case did RA succeed where ELCA had failed. There were four procedure-related complications, including transient no-reflow, side branch occlusion and two coronary perforations, of which one was directly attributable to ELCA and led to subsequent mortality.
Conclusions: ELCA provides safe and effective adjunctive therapy in contemporary PCI to treat lesions associated with balloon failure due to an inability either to cross the lesion or to expand a balloon sufficiently to permit stenting. ELCA was successful in the majority of these selected cases when used independently with further effectiveness achieved when combined with RA or after RA failure.
Abbreviations
ELCA: excimer laser coronary atherectomy
RA: rotational atherectomy
PCI: percutaneous coronary intervention
CTO: chronic total occlusion
Introduction
Failure to cross or expand a coronary stenosis with an angioplasty balloon (balloon failure) is often associated with technical failure, incomplete revascularisation and complications. With the increasing age of the PCI population and the increasing complexity of cases being undertaken in many centres, balloon failure is now encountered more frequently, particularly in high-volume units dealing with elderly patients.
Typical lesions encountered in balloon failure are significantly calcified stenoses, chronic total occlusions (CTO) and non-compliant plaques, which often require utilisation of techniques other than balloon angioplasty in order to prepare the vessel for stenting. Adequate lesion debulking is considered mandatory in the drug-eluting stent (DES) era to permit better procedural success and target lesion revascularisation (TVR), and to facilitate stent expansion with sufficient wall apposition to reduce the incidence of late stent thrombosis (LST)1.
The most commonly used device for heavily calcified coronary lesions and identified or perceived balloon failures is certainly rotational atherectomy (RA) and perhaps it is not surprising that this device has seen a surge in uptake over the last few years2. There is good evidence that, when dealing with heavily calcified lesions, the combined approach of RA-DES has a favourable effect on both angiographic and clinical outcomes3,4. However, RA is a demanding technique that requires advanced PCI training and in most centres only the minority of operators are proficient in these skills. Additionally, even in experienced hands there are occasions when the dedicated RotaWireTM (Boston Scientific, Natick, MA, USA) cannot be delivered beyond the lesion, either independently or using a microcatheter exchange system, which is usually the case when treating CTOs, thus rendering RA impossible.
Alternative techniques, such as upsizing the guide catheter, the use of the GuideLinerTM catheter (Vascular Solutions Inc., Minneapolis, MN, USA), the parallel wire technique or the anchor technique, may assist passage of balloon or microcatheter across the lesion, but success is variable and often dependent on operator experience. The Tornus® penetration catheter (Asahi Intecc Co., Ltd, Aichi, Japan) and Corsair microcatheter (Asahi Intecc Co., Ltd, Aichi, Japan) are alternative devices that have demonstrated success in CTO. These devices can be used to create a channel through the lesion to permit subsequent balloon or microcatheter passage and can therefore be used alone or in combination with RA. The Tornus® device is 0.014” compatible with either a 300 cm exchange length guidewire or a standard length (180-190 cm) guidewire using a balloon trapping technique and a suitably sized guide catheter. It has been compared with RA in a retrospective study of CTO cases but there are no direct prospective comparative trials of these devices against each other5.
Excimer laser coronary atherectomy (ELCA) has an established role in the treatment of balloon failure occurring due to mild-moderate calcification6-10. A major advantage of ELCA is that the catheter is deliverable using the standard 0.014” guidewire and therefore, unlike RA, it can be utilised more readily when a CTO has been crossed. Furthermore, the technique itself is relatively simple to master and more easily adoptable by most PCI operators when compared to RA11.
Briefly, the rapid-exchange ELCA catheter is advanced to the lesion and, during continuous saline flush, lasing commences with gentle, slow, forward traction of the catheter. The pulsed ultraviolet emitted (wavelength 308 nm) has a shallow penetration depth reducing the risk of dissection and vessel perforation. For non-crossable and non-expansile lesions the highly deliverable 0.9 mm X-80 catheter is favoured with maximum fluence (energy) 80 mJ/mm2 and repetition rate 80 Hz attainable. Activation of 10 seconds is followed by a mandatory rest of five seconds between each lasing period, which is continued until either the catheter has traversed the lesion, or sufficient lesion modification has occurred to permit balloon crossing or expansion.
In the last four years there has been an increase in the number of European PCI centres which have the ability to offer ELCA on site. However, there is a paucity of data on the overall success rates of ELCA for balloon failure in patients undergoing contemporary PCI6-10 and, in addition, there is little guidance on the safety aspects. The latter is important given that previous studies using earlier generation ELCA equipment and techniques reported specific risks, including major coronary dissection (in up to 5% of cases) and coronary perforation (0.6% of cases)12,13.
ELCA is usually successful without the need for additional RA, but the combination may be useful for selected lesions with more resistant calcification14,15. Lesions that cannot be treated with RA initially, due to an inability to advance a RotaWireTM, can first be treated with ELCA with the understanding that the device will not fully debulk the lesion to permit stenting. However, the “pilot hole” created by ELCA can then be used to pass a RotaWireTM, either independently or via a microcatheter exchange technique, to permit subsequent RA and achieve procedural success. We have previously reported this combination of ELCA and RA and termed it the “Raser” technique14,15.
The objective of this retrospective study was to analyse balloon failure cases treated with ELCA±RA in our centre over a four-year period.
Methods
We performed a retrospective analysis, identifying all patients who had ELCA for balloon failure during a four-year period at our centre. This was defined as: failure of the balloon to cross (using the lowest-profile balloon available at the point where predilatation was required, despite good guide catheter and wire support); and failure of adequate balloon expansion (<50% expansion achieved or repeated balloon rupture). These were subclassified according to whether the treated coronary artery was a CTO (defined as complete obstruction of a coronary artery with TIMI 0 or 1 flow for >3 months) or where there was TIMI 3 flow in the distal vessel beyond the lesion.
In all cases we utilised the CVX-300 Excimer Laser System (wavelength 308 nm, pulse duration 135 ns, output of 165 mJ/pulse; Spectranetics Inc., Colorado Springs, CO, USA) in conjunction with a Vitesse CTM laser atherectomy 0.9 mm catheter (Spectranetics Inc.). The “saline flush” technique16,17 was used whereby all contrast in the coronary artery, guide catheter and manifold was flushed out with 0.9% normal saline prior to lasing with 5 to 10 mls of saline injected as a bolus prior to each train of laser pulses through the guide catheter and continued at a rate of 1 ml/sec during lasing. The laser catheter was advanced at a rate of 0.5-1 mm/sec for a maximum of 10 seconds per train with at least five seconds allowed between trains of laser energy.
We recorded patient demographics, lesion characteristics, procedure details, laser and procedural success and complications. Lesion characteristics recorded were: CTO, ACC lesion classification, calcification (graded angiographically as none, mild, moderate or severe), angulation (with moderate angulation defined as ≥45 degrees), and lesion length in mm. Procedure details included number of ELCA trains, fluence, total pulses delivered in addition to case fluoroscopy dose and contrast volume.
Procedural success was defined as successful stent deployment and residual stenosis <20% without major complications of flow-limiting dissection or vessel perforation with extravasation (Type II or Type III). ELCA success alone was defined as successful case completion where the ELCA catheter had either fully crossed the lesion or sufficiently modified the plaque to permit subsequent balloon crossing and expansion. Complications of no-reflow, flow-limiting dissection, vessel perforation, Q-wave myocardial infarction and death were recorded. Data are reported as mean±standard deviation.
Results
We identified 58 cases of balloon failure treated with ELCA from 6,882 consecutive patients undergoing PCI in our centre over a four-year period from January 2007 to January 2011 (0.84%). To put ELCA use for this indication into greater perspective, 58 cases represented 35% of all ELCA cases performed compared with 187 RA cases (2.7% of all PCI) during this period. RA is the first choice device used in our centre for lesions with angiographic severe calcification.
Of the aforementioned 58 cases, 36 cases (62%) were due to failure of the balloon to cross the lesion, of which 16 cases were in the context of CTO. In the remaining 22 cases (38%), ELCA was used after failure of balloon expansion, of which only two cases were for CTO. Eighty-four per cent of patients were male and the average age was 72±8.5 years with 50% of patients >75 years old (Table 1).
Overall procedural success was obtained in 53 cases (91%). In 76% of cases ELCA was the only atherectomy device required to achieve a successful outcome. In the majority of these cases the ELCA catheter traversed the lesion completely, but in some the catheter could not be advanced beyond the distal lesion. These cases were still considered ELCA success, so long as the original balloon that would not initially advance could now cross and expand the lesion permitting a successful outcome.
In five cases (8.6%) where there was angiographic severe calcification, ELCA was necessary to provide a pilot hole to permit passage of a RotaWireTM with subsequent RA – the “Raser” technique. In four cases (6.8%) ELCA was used after RA had been unsuccessful owing to severe vessel tortuosity and/or inability to advance a RotaWireTM. In one case of angiographic moderate calcification (1.7%) ELCA was unsuccessful and RA was required to complete the case.
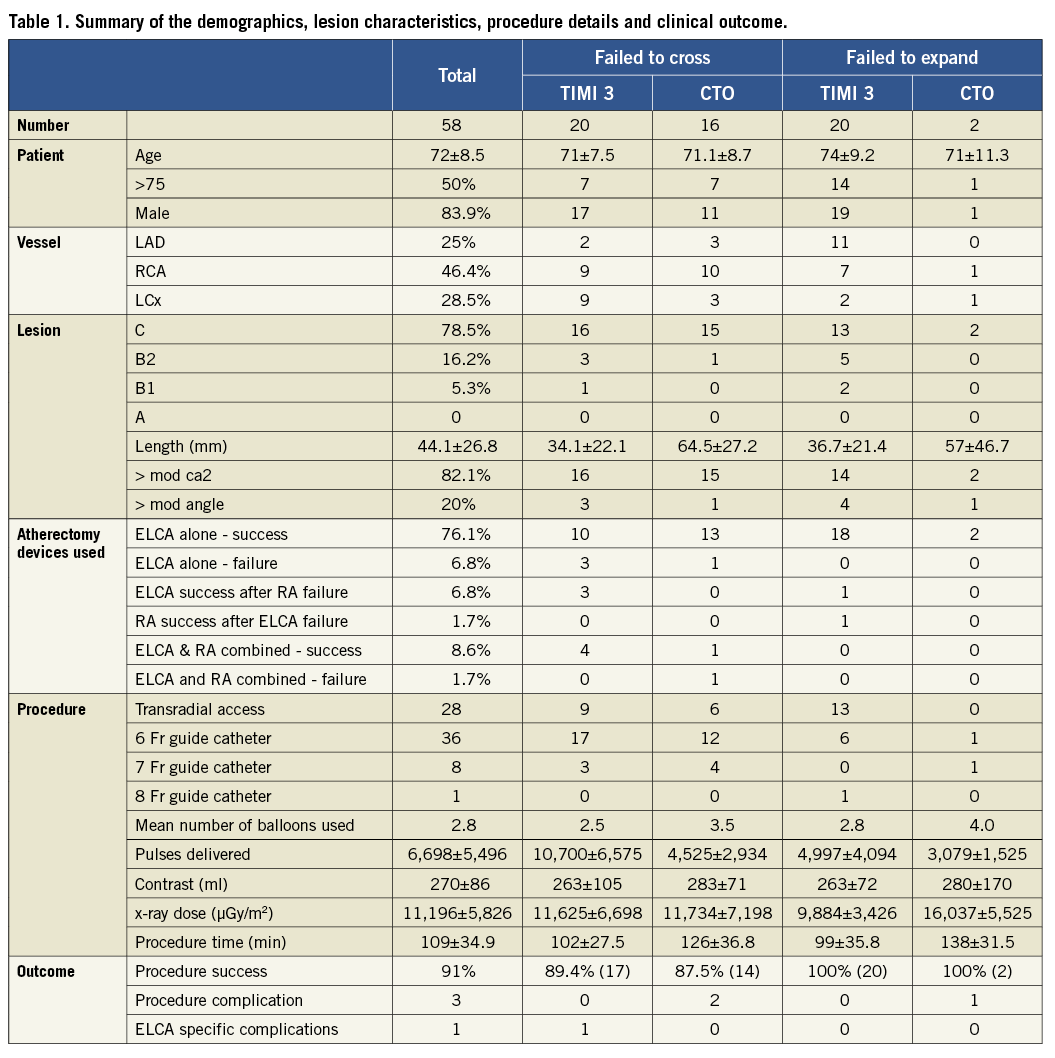
FAILURE OF BALLOON TO CROSS (Figure 1 and Figure 2)
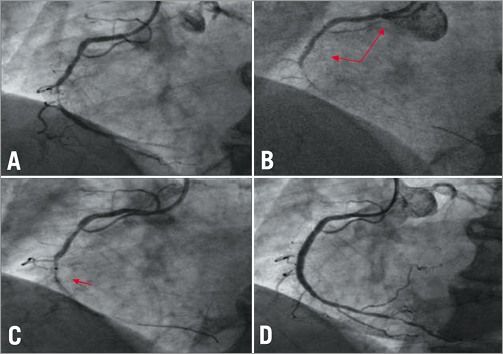
Figure 1. All left anterior oblique (LAO) projections of the RCA. A) Severe mid calcific stenosis with TIMI 3 flow. B) 1.5 mm balloon would not traverse the target stenosis backing out the guide catheter (arrows). C) 0.9 mm ELCA catheter (arrow). D) Final angiographic result.
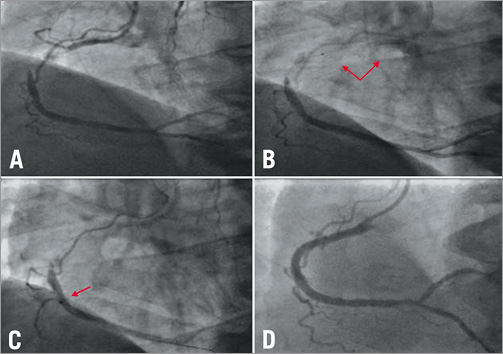
Figure 2. All LAO projections of the RCA. A) Large dominant vessel with a proximal chronic total occlusion (CTO) lesion. B) FineCross MG catheter would not traverse the CTO backing out the guide catheter (arrows). C) 0.9 mm ELCA catheter (arrow). D) Final angiographic result.
Thirty-six cases of failure to cross were identified. Sixteen cases (44%) were in the context of CTO. The mean minimum balloon diameter utilised was 1.18±0.15 mm.
For the CTO cases laser energy was delivered with 7.6±5.1 trains, maximum fluence of 72.8±11.5 mJ/mm2 and frequency of 66.6±20.9 hertz, delivering a total of 4,525±2,934 pulses.
ELCA used alone led to procedural success in 13 cases (81%). One case required combined ELCA and RA with initial laser to permit passage of the RotaWireTM in order to attain procedural success. Two cases were abandoned after successful wiring of the CTO, with ELCA used alone failing in one case and in combination with RA in the other. One patient developed transient no-reflow remote from ELCA use without subsequent rise in cardiac enzymes. There were no flow-limiting coronary dissections or perforations.
For the 20 cases where a balloon failed to cross lesions with TIMI 3 flow, laser energy was delivered with 15.8±7.3 trains, maximum fluence of 76.8±7.5 mJ/mm2 and frequency of 73.7±15.0 hertz, delivering a total of 10,700±6,575 pulses.
ELCA used alone led to procedural success in 10 cases (50%). Four cases required the “Raser” technique with combined ELCA and RA to achieve procedural success. In three cases where RA was not successful (severe tortuosity and inability to pass a RotaWireTM), ELCA use led to successful outcome of the procedure. Three cases were abandoned after successful wiring of the vessel with ELCA being the only atherectomy device utilised. Complications included one case of a patient where procedural success was associated with occlusion of a side branch without significant rise in cardiac enzymes. There were no flow-limiting coronary dissections, but the ELCA catheter was associated with a Type III coronary perforation in one case14,15. This patient was initially stabilised by treating with bare metal stents, as a covered stent could not cross the lesion. However, further persistent haemorrhage led to cardiogenic shock and subsequent mortality.
FAILURE OF BALLOON EXPANSION (Figure 3 and Figure 4)
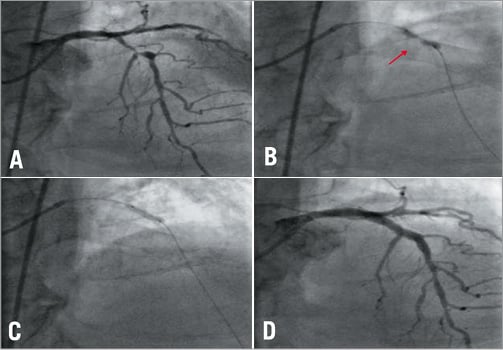
Figure 3. All posteroanterior (PA) cranial projections of the LAD. A) Severe and calcific proximal stenosis in the LAD. B) Failure to expand with a residual waist despite high pressure inflation (arrow). C) Full balloon expansion achieved post ELCA. D) Final angiographic result.
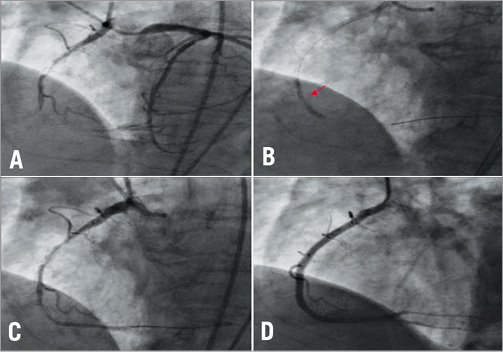
Figure 4. All LAO projections of the RCA. A) Large dominant right coronary artery with a severely calcified proximal CTO. Contralateral injection technique to visualise the distal vessel. B) Failure to expand with a residual waist despite high pressure inflation (arrow). C) Post 0.9 mm ELCA. D) Final angiographic result.
Twenty-two cases of balloon expansion failure were identified of which two cases (9%) were in the context of CTO. In each case the failed balloon expansion was from a non-compliant balloon at high pressure and in some cases a double-coated balloon at >30 atm. In the two CTO cases, laser energy was delivered with 6.0±1.4 trains, maximum fluence of 70.0±14.1 mJ/mm2 and frequency of 60.0±28.3 hertz, delivering a total of 3,079±1,525 pulses. Both cases were successfully treated with ELCA used alone. In one case there was a Type I (contained) perforation without extravasation, related to subsequent balloon dilatation remote from ELCA use, which was successfully treated with drug-eluting stents. There were no flow-limiting coronary dissections.
In the 20 cases where a balloon had failed to expand the lesion in the presence of TIMI 3 flow, laser energy was delivered with 9.5±7.8 trains, maximum fluence of 75.0±8.9 mJ/mm2 and frequency of 70.0±17.8 hertz, delivering a total of 4,997±4,094 pulses. ELCA used alone led to procedural success in 18 cases. In one case ELCA was successful after RA had failed (unable to deliver RotaWireTM or use a microcatheter exchange system). In the remaining case, ELCA was unsuccessful at debulking the moderate angiographic calcification and RA was required to achieve procedural success. In this group of patients there were no procedure-related complications and, in particular, no flow-limiting coronary dissections or perforations.
Discussion
Adequate preparation of significant coronary artery lesions for stenting can usually be achieved with balloon angioplasty18. However, failure of a balloon to cross or adequately expand the coronary lesion is a well-recognised problem6-10. Indeed, with an ageing population requiring PCI with increasingly complex calcified disease, it will continue to be a taxing clinical problem despite improvements in guidewire and balloon technology and the increasing use of rotational atherectomy to debulk calcified lesions.
Without doubt, RA remains the adjunctive therapy of choice for balloon failure cases, particularly for those where severe calcification is present2,3. However, this study demonstrates that ELCA can be considered an alternative to RA for a range of balloon failure cases and an additional adjunctive therapy to RA when dealing with severe calcification and an initial inability to pass a RotaWireTM.
There are of course a variety of other ways to deal with an inability to cross the lesion with a balloon, including techniques such as upsizing the guide catheter, use of the GuideLinerTM catheter25 (Vascular Solutions, Minneapolis, MN, USA), the parallel wire or the anchor balloon method. These may permit passage of a balloon or microcatheter across the lesion, but further problems with balloon expansion may then limit success and necessitate RA. Devices such as the Tornus® penetration catheter (Asahi Intecc, Aichi, Japan) are a further development with demonstrable success in the treatment of CTO. However, a small study compared the historical use of RA in 41 patients with a CTO, where the smallest balloon would not cross, with 36 more contemporary CTO cases where Tornus® was used as the first device. The Tornus® group had longer procedure times and less success compared to the RA group with RA required in three of the eight Tornus failure cases5.
Cutting balloons19 and double-coated balloons (Schwager Medica AG, Winterthur, Switzerland) are other devices which can successfully dilate lesions where conventional semi- and non-compliant balloons have failed, but delivery to the lesion can often be challenging. In one notable case from our series, a double-coated balloon failed to expand at 40 atm despite the lesion having been treated using RA with a 2.0 mm burr20.
In this study ELCA was used in 0.84% of balloon failure PCI cases over a four-year period with nearly one third of these cases for CTO. During the same period RA was used in 2.7% of cases reflecting the fact that this technique remains our first choice atherectomy device for treating significantly calcified lesions. However, the use of RA in CTO is usually limited by an inability to traverse the lesion with a RotaWireTM and therefore the successful utilisation of an alternative atherectomy device, such as ELCA which can be delivered over a standard 0.014” guidewire, offers a real advantage. In our study the use of ELCA alone in treating CTO with balloon failure was associated with a high success rate and a low complication rate.
Severe coronary lesions where the distal vessel is well visualised and can be crossed with a standard 0.014” guidewire but not with a low-profile balloon can be treated with ELCA. It is evident from our study that although the success rate remains high (65% with ELCA alone or after failed RA), additional RA is still required in some cases after ELCA (although RA could not be performed without initial ELCA in some cases). RA would perhaps have been an alternative in the three cases where ELCA failed.
It is well recognised that ELCA is not usually sufficient for adequate debulking of severe calcification independently and we would not recommend its use as an alternative to RA in these circumstances. However, when dealing with mild-moderate calcification ELCA will usually suffice to enable balloon passage and dilatation leading to procedural success. It is notable from Table 1 that this particular cohort of patients required relatively more use of the ELCA catheter with more pulses delivered but similar procedure times and contrast dose compared to the other patient groups.
Similarly, for lesions crossed with a standard “workhorse” guidewire and balloon, but where the balloon fails to expand, ELCA provides a highly successful and safe alternative to RA as long as there is no evidence of severe calcification. The potential mechanism for underexpansion of the balloon in these lesions is a short focal area of fibro-calcific disease, which is usually amenable to absorption of laser energy and subsequent ablation. Severely calcified lesions will be more resistant to laser energy making RA the therapy of choice in these situations. However, it should be noted that, even after apparent RA success with the largest burr available, balloon and stent expansion can still remain inadequate. We have successfully used ELCA to permit full stent expansion in exactly this situation20.
ELCA was first approved for use in cases of balloon failure during PCI in the USA in 1992 by the U.S. Food and Drug Administration. There is, however, little data on its use, particularly in contemporary practice. There are several case reports of its use for balloon failure in the balloon angioplasty era1,7-9. In addition, the percutaneous ELCA (PELCA) multicentre registry enrolled 37 patients with balloon failure (24 with failure of balloon to dilate and 14 with failure to cross) from 1989 to 19937. The technology available at that time was limited to 1.4, 1.7 and 2.0 mm laser catheters and the laser energy delivered was much lower than current practice with a maximum of 60 fluence and 25 hertz. It was also prior to the introduction of continuous saline flushing during lasing, which has been shown to decrease complications16,17. Complication rates in these patients were high (8% significant dissection, 3% perforation, 3% acute stent thrombosis and 3% emergency bypass surgery) and laser success rates were only 37%, although clinical success was obtained in 89%.
Advances in PCI (with improved wire and balloon technology, the near universal use of coronary stents and the introduction of various drug-eluting stents) have increased the range of indications for PCI and improved outcomes since the 1990s. There has been a resulting increase in case complexity. At the same time there have also been significant advances in ELCA technology, particularly with the introduction of a 0.9 mm laser catheter, an increase in the laser energies delivered and the use of a continuous saline flush system6,16,17.
Bilodeau et al studied the novel 0.9 mm catheter and saline flush technique in 100 calcified and complex lesions (including 35 in which there was primary “balloon failure” although this was not defined or analysed independently)8. They also utilised higher laser energies and demonstrated that increased laser energies increased laser success rates without an obvious increase in complications. In this study, overall laser and procedural success rates were over 90%. Complications included in-hospital death (2%), myocardial infarction (4%) and coronary dissection (5%).
Shen et al have more recently reported a series of 33 cases in which they utilised ELCA, although without the saline flush technique (including 21 patients with failure of balloon to cross, 15 in the context of CTOs)9. They reported a success rate of 90% and no complications directly related to laser catheter treatment.
Our observational study comprises the largest series of ELCA for balloon failure lesions reported to date and includes a high proportion of CTO cases. We have shown that ELCA now enables successful completion of the majority of PCI cases (over 90% of cases in our series, which is in keeping with other smaller recent studies)7-9 where there is balloon failure, with acceptable complication rates. We believe that ELCA is a useful adjunctive therapy for the treatment of non-crossable and non-expansible lesions. PCI centres undertaking high-volume PCI, particularly in elderly populations, should expect to encounter such challenging lesions and, whilst ELCA is not the only solution, it offers an effective alternative to devices such as the Tornus or Corsair.
In times of austerity and budgeting constraints, the financial implication of using ELCA in PCI has to be assessed. In the UK at least, the consumable cost of the catheter is comparable with that of RA (RotaWireTM, advancer and burr) whilst it is about twice the cost of a Tornus or Corsair catheter. However, the purchase and maintenance of the CVX-300 excimer laser console is considerable, but can be somewhat offset by the multiple uses of the system. Within the PCI setting, ELCA is also indicated for treating saphenous venous grafts21, dealing with thrombus in acute myocardial infarction22-24 and treating significant in-stent restenosis26. Excimer laser sheaths for pacing and defibrillator lead removal have an expanding role and there is widespread use of catheters in treating peripheral vascular disease including limb salvage due to critical ischaemia.
Conclusion
Balloon failure is not uncommon in high-volume PCI centres with elderly populations. Rotational atherectomy remains the adjunctive treatment of choice in heavily calcified lesions but the use of this technique is dependent on delivery of a dedicated RotaWireTM and requires advanced PCI operator training which may not always be available. This study demonstrates that ELCA, a device delivered on the standard 0.014” guidewire, provides a useful adjunct to contemporary PCI practice in such cases. ELCA, either utilised independently or in combination with rotational atherectomy, enabled successful and safe completion of the procedure in 91% of cases in our study where there was either failure to cross the lesion with the balloon or where the balloon could not be expanded. In one third of these balloon failure cases the lesion was a chronic total occlusion and it is in these circumstances that ELCA could subsequently prove to be the device of choice.
Conflict of interest statement
P. O’Kane and S. Talwar are European proctors for Spectranetics. The other authors have no conflicts of interest to declare.

