Abstract
Aims: Our aim was to report on a survey initiated by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) collecting the opinion of the cardiology community on the invasive management of acute coronary syndrome (ACS), before and after the MATRIX trial presentation at the American College of Cardiology (ACC) 2015 Scientific Sessions.
Methods and results: A web-based survey was distributed to all individuals registered on the EuroIntervention mailing list (n=15,200). A total of 572 and 763 physicians responded to the pre- and post-ACC survey, respectively. The radial approach emerged as the preferable access site for ACS patients undergoing invasive management with roughly every other responder interpreting the evidence for mortality benefit as definitive and calling for a guidelines upgrade to class I. The most frequently preferred anticoagulant in ACS patients remains unfractionated heparin (UFH), due to higher costs and greater perceived thrombotic risks associated with bivalirudin. However, more than a quarter of participants declared the use of bivalirudin would increase after MATRIX.
Conclusions: The MATRIX trial reinforced the evidence for a causal association between bleeding and mortality and triggered consensus on the superiority of the radial versus femoral approach. The belief that bivalirudin mitigates bleeding risk is common, but UFH still remains the preferred anticoagulant based on lower costs and thrombotic risks.
Introduction
Multiple studies have investigated the transradial as compared to the transfemoral approach and bivalirudin versus unfractionated heparin (UFH) treatment in patients with acute coronary syndrome (ACS) undergoing invasive management1-8. However, it remained unclear whether avoiding access-site bleeding and vascular complications through routine transradial interventions improved outcomes (i.e., mortality)1-4. Moreover, the evidence regarding bivalirudin as compared to UFH with or without glycoprotein IIb/IIIa inhibitors (GPI) was conflicting5-8, and the debate on the most effective antithrombotic regimen for preventing ischaemic complications, while limiting bleeding risk, remained unresolved.
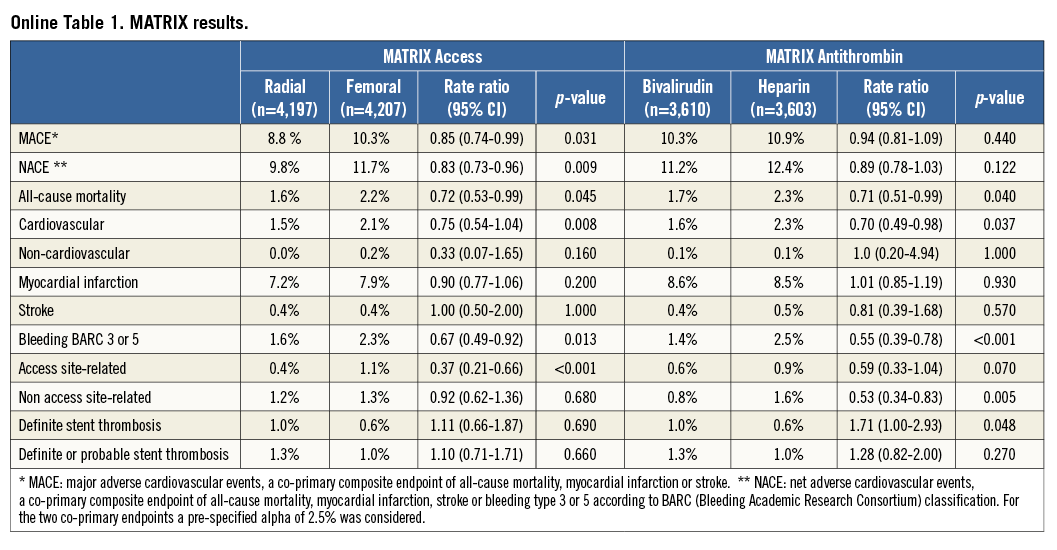
During the American College of Cardiology (ACC) 2015 Scientific Sessions, the results from the MATRIX trial9-12 – a multinational randomised study involving more than 8,000 unselected ACS patients and comparing both radial with femoral access (MATRIX-Access) and bivalirudin with UFH±GPI (MATRIX-Antithrombin) – were reported (Online Table 1). This trial demonstrated the superiority of the radial as compared to the femoral approach with respect to the composite co-primary endpoint of net cardiovascular adverse events (NACE) owing to a significant reduction of mortality and access-site bleeding. Although the two co-primary endpoints of major cardiovascular events (MACE) and NACE were not met for the antithrombotic treatment, a lower mortality and bleeding rate in patients treated with bivalirudin, as compared to those receiving UFH±GPI, was observed.
The aim of this manuscript is to summarise the results of a voluntary web-based survey undertaken by the European Association of Percutaneous Coronary Interventions (EAPCI) in order to collect the opinions of the scientific community regarding the invasive management of ACS patients (i.e., arterial access site and antithrombotic therapy) before and after ACC 2015.
Methods
This survey consisted of two sets of questions, dispensed before and after the ACC 2015 congress. Both the pre- and post-ACC survey investigated the clinical practice and interpretation of evidence on the radial as compared to the femoral approach and on bivalirudin as compared to UFH. The questionnaires were drafted by the EAPCI Scientific Documents Committee and subsequently approved by the EAPCI board. The survey was undertaken using a free web-based survey tool (Survey Monkey, Palo Alto, CA, USA) and comprised multiple-choice questions, including the possibility to add comments if required. It was not mandatory to reply to the entire survey. The sample population comprised the mailing list of EuroIntervention – the official journal of the EAPCI. Overall a total of 15,200 individuals were invited to participate. The first part of the survey was performed between 25 February 2015 and 5 March 2015. The second part of the survey was carried out from 8 to 15 April 2015.
The data are reported as percentages and compared using the chi-square test. A two-sided p-value <0.05 was considered significant. The results were stratified by age (i.e., <40 vs. between 40 and 50 vs. >50 years), country (i.e., European vs. non-European and European vs. North American), PCI volume centre (i.e., <600 vs. between 600 and 1,000 vs. >1,000 in year 2014), radial PCI volume centre (i.e., <60% vs. between 60 and 80% vs. >80% in year 2014); professional figure (i.e., interventional cardiologists with more than 10 vs. between 5 and 10 vs. <5 years of experience vs. non-interventional cardiologists) and bivalirudin use (none vs. in less than 30% vs. in at least 50% of patients). All analyses were performed with SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
RESPONDENT CHARACTERISTICS
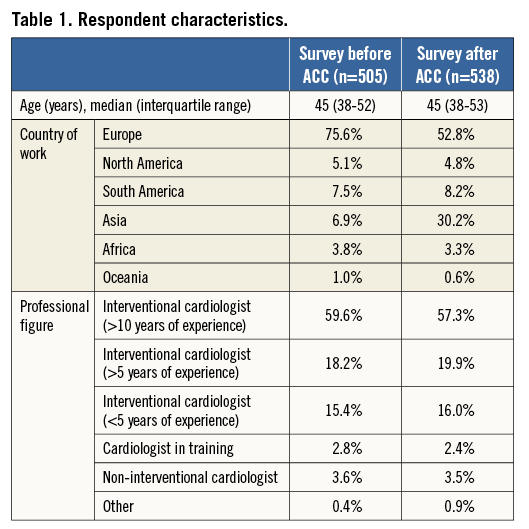
Of the 15,200 invitations sent, a total of 572 (3.8%) and 763 (5.0%) physicians responded to the first and the second part of the survey, respectively. Among these, 505 (88.3%) for the first and 538 (70.5%) for the second survey provided personal and professional information with respect to age, geographic region of practice and medical qualifications (Online Appendix). The participants’ characteristics are detailed in Table 1. The median age of respondents was 45 years in both the pre- and the post-ACC survey. A significantly higher rate of non-European respondents was observed in the post- compared with the pre-ACC survey (47.2% vs. 24.4%; p<0.001). The majority of participants were interventional cardiologists with more than 10 years of experience in both surveys (59.6% and 57.3%; p=0.44).
Only 59 physicians responded to both surveys with results consistent with the overall population.
ACCESS-SITE COMPARISON
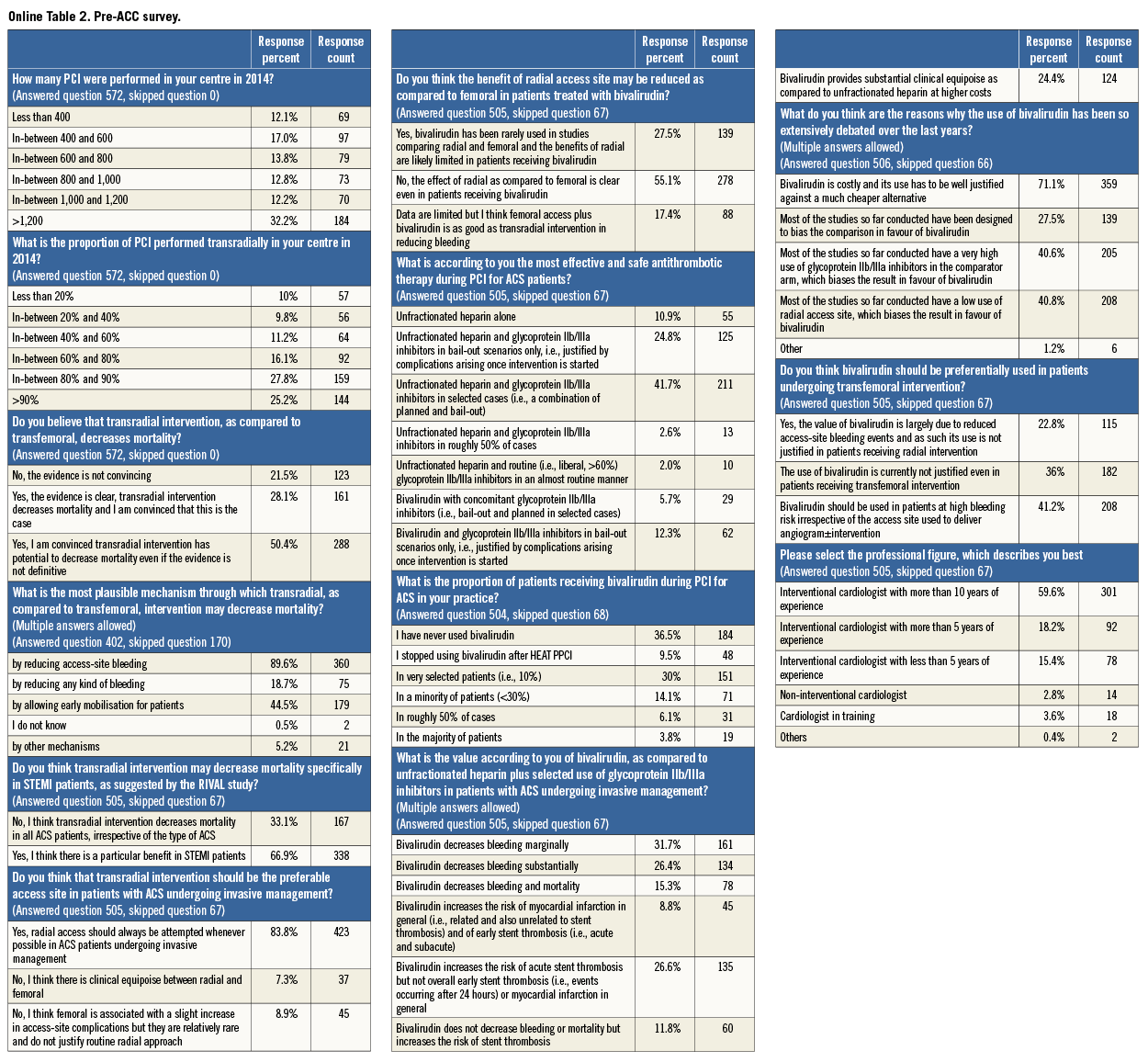
The overall findings of the pre- and post-ACC surveys are shown in Online Table 2 and Online Table 3.
CLINICAL SETTING AND OPINIONS OF PARTICIPANTS IN THE PRE-ACC SURVEY
Among respondents to the first part of the survey, more than 40% worked in high-volume PCI centres (>1,000 in the year 2014) and roughly 50% of them declared practising in institutions performing more than 80% transradial PCI. The majority of respondents (83.8%) believed that the transradial approach should be the preferred access site in ACS patients undergoing invasive management (Figure 1A). Europeans (Figure 1B) or cardiologists working in high-volume radial PCI centres (Figure 1C) were more likely to give preference to a transradial intervention. On the other hand, overall PCI volume did not affect the choice for a preferred access site (Figure 1D).
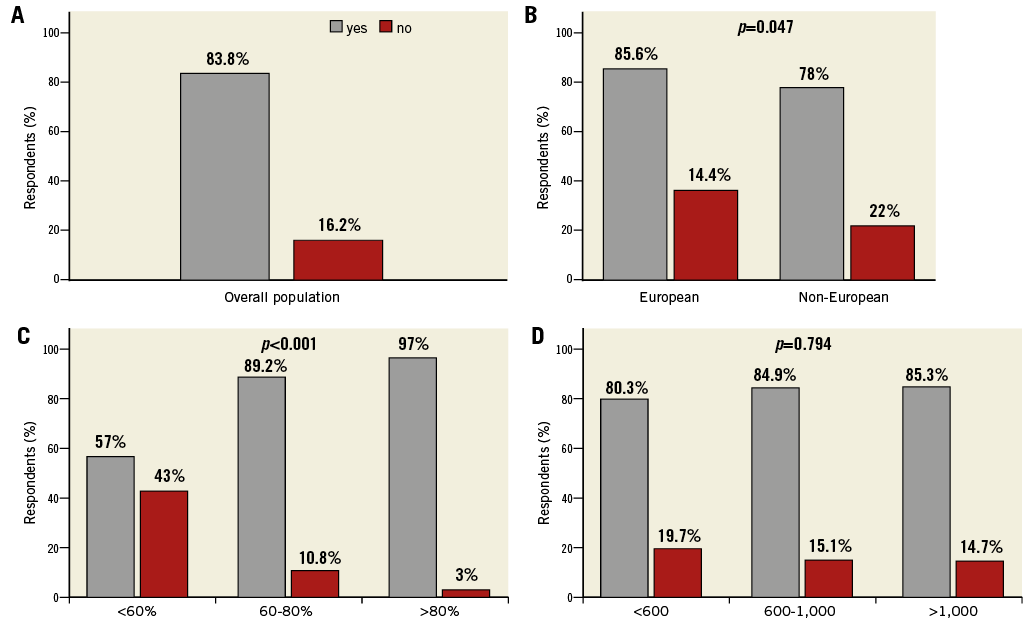
Figure 1. Do you think that transradial intervention should be the preferable access site in patients with ACS undergoing invasive management? The answers of overall respondents (A) and of population stratified by country (B) radial PCI volume (C) and PCI volume (D) are shown. In panel C, radial PCI volume is reported as percentage of transradial PCI performed at the centre in 2014. In panel D, PCI volume is reported as number of PCI performed at the centre in 2014.
More than three quarters of the respondents (78.5%) believed that a transradial intervention has potential to decrease mortality (Figure 2A). This opinion was highly related to the declared radial PCI volume in practising institutions (57.6% vs. 77.2% vs. 91.1% in low, medium and high radial PCI volume centres, respectively; p<0.001) (Figure 2B). Of note, participants older than 50 years were less frequently convinced that transradial as compared to transfemoral intervention might decrease mortality (73.9% vs. 81.8% in younger than 50 years; p=0.042) (Figure 2C).
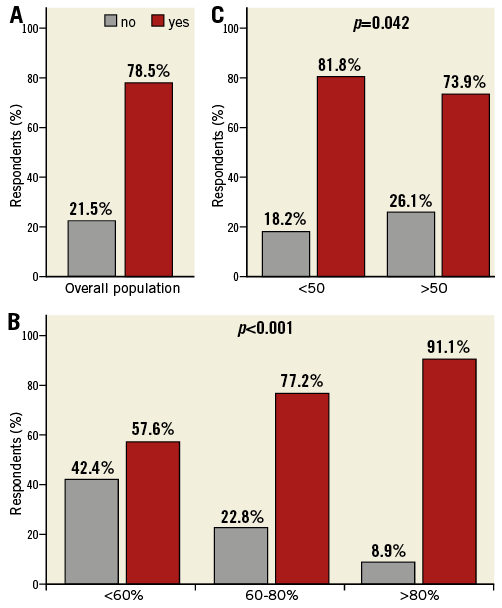
Figure 2. Do you believe that transradial intervention, as compared to transfemoral, decreases mortality? The answers of overall respondents to the pre-ACC survey (A) and of population stratified by radial PCI volume (B) and age (C) are shown. No=the evidence is not convincing Yes=the evidence is clear, transradial intervention decreases mortality and I am convinced that this is the case or I am convinced transradial intervention has potential to decrease mortality even if the evidence is not definitive. In panel B, radial PCI volume is reported as percentage of transradial PCI performed at the centre in 2014.
Reducing access-site bleeding was the most prevalent putative explanation for mortality reduction after transradial intervention (89.6%), followed by early mobilisation (44.5%).
Two thirds of respondents (66.9%) thought that mortality benefit observed after radial intervention may largely depend on the clinical presentation. Finally, more than half of respondents (55.1%) were convinced that the benefits of the radial approach are independent of bivalirudin use in practice with gradients observed in European vs. non-European participants (58.9% vs. 43.1%; p=0.004), cardiologists working at high vs. medium or low radial PCI volume centres (64.6% vs. 50.6% and 40.4%, respectively; p<0.001) and interventional vs. non-interventional cardiologists (56.8% vs. 31.4%; p=0.011).
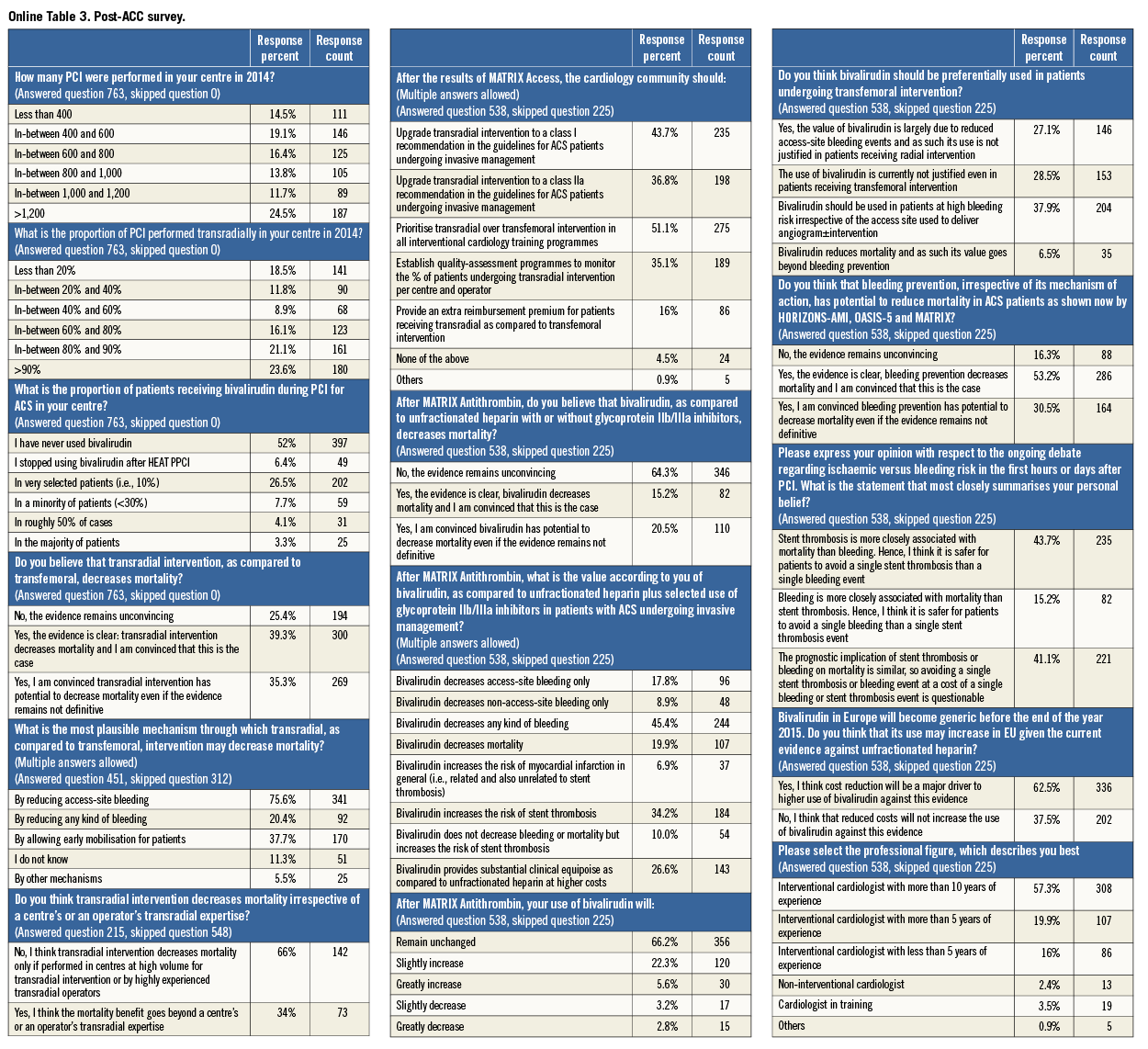
CLINICAL SETTING AND OPINIONS OF PARTICIPANTS IN THE POST-ACC SURVEY
The percentage of respondents working at high PCI or high radial PCI volume centres was significantly lower in the post- as compared to the pre-ACC survey (44% vs. 36.2%; p=0.010 and 53% vs. 44.7%; p=0.004, respectively).
No difference was noted between the pre- and post-ACC survey with respect to percentages of respondents who believed (78.5% vs. 74.6%) or disbelieved (21.5% vs. 25.4%) that the radial approach may reduce mortality (p=0.096). These results were consistent after stratification by age, country, professional figure and PCI or radial PCI volume. However, among respondents who vouched for a possible mortality benefit conferred by the radial approach, the proportion of those who interpreted the evidence as definitive significantly increased in the post-ACC survey (35.9% vs. 52.7%; p<0.001) (Figure 3).
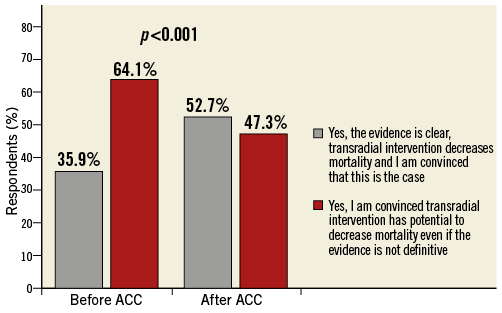
Figure 3. Do you believe that transradial intervention, as compared to transfemoral, decreases mortality? Only respondents who believed that transradial intervention, as compared to transfemoral, decreases mortality are reported (449 out of 572 in the pre-ACC survey; 569 out of 763 in the post-ACC survey).
Consistent with the pre-ACC survey results, cardiologists working at low radial PCI volume centres, a non-European –in particular North American– work setting and age more than 50 were associated with a higher disbelief among respondents that the radial approach has potential to decrease mortality risk. Reducing access-site bleeding remained the single most frequently chosen reason (75.6%) to explain mortality benefit after transradial access, followed by early mobilisation (37.7%). The percentage of respondents who were unsure about the reasons behind the mortality reduction after the radial approach increased from 0.5% before ACC to 11.3% (p<0.001) after ACC 2015. Trends were noted based on the age of respondents (1.3% vs. 6.7% vs. 12.3% in physicians younger than 40, between 40 and 50 and older than 50, respectively; p<0.001) and respondents working at high versus non-high radial PCI volume centres (3.2% vs. 4.9% and 11.4% in high, medium and low radial PCI volume centres, respectively; p<0.001).
After ACC 2015, two thirds of respondents were convinced that a transradial intervention decreases mortality only if performed by expert operators practising in centres with a high volume for transradial procedures, with a significant difference between European and non-European respondents (73.2% vs. 55.7%; p=0.007).
Half of the participating physicians, mostly working at high-volume radial PCI centres (p<0.001), believed that in the light of the results of the MATRIX Access trial the cardiology community should prioritise the training of transradial over transfemoral procedures. More than 40% of participants, mainly European (p=0.003) and coming from high-volume radial PCI centres (p<0.001), declared that, after the MATRIX Access trial, the transradial approach should be upgraded to a class I recommendation in the guidelines for ACS patients undergoing invasive management (Figure 4).
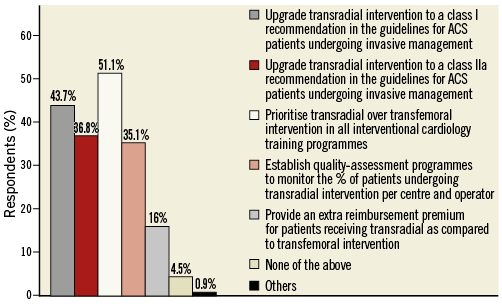
Figure 4. After the results of MATRIX Access, the cardiology community should… (Multiple answers allowed).
ANTITHROMBIN TYPE COMPARISON
The overall findings of the pre- and post-ACC surveys are shown in Online Table 2 and Online Table 3.
CLINICAL SETTING AND OPINIONS OF PARTICIPANTS IN THE PRE-ACC SURVEY
Slightly less than half of respondents declared no prior use of bivalirudin or having discontinued it in practice after the HEAT PCI study results, with a significant gradient observed in the European vs. North American respondents (89.5% vs. 65.4%; p<0.001). The vast majority of physicians identified heparin±GPI as the most effective and safe antithrombotic therapy during PCI in ACS patients (Figure 5A), with a gradient of convincement based on prior use of the drug (90.9% in non-bivalirudin users vs. 81.2% and 44% in low and high bivalirudin users, respectively; p<0.001) (Figure 5B).
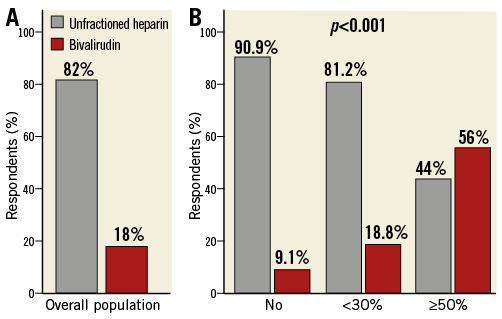
Figure 5. What is according to you the most effective and safe antithrombotic therapy during PCI for ACS patients? The answers of overall respondents (A) and of population stratified by prior bivalirudin use (B) are shown. Unfractionated heparin (UHF)=UHF alone or UHF+glycoprotein IIb/IIIa inhibitors (GPI) in bail-out scenarios only, i.e., justified by complications arising once intervention is started or UHF+GPI in selected cases (i.e., a combination of planned and bail-out) or UHF+GPI in roughly 50% of cases or UHF+routine (i.e., liberal, >60%) GPI in an almost routine manner. Bivalirudin=bivalirudin with concomitant GPI (i.e., bail-out and planned in selected cases) or bivalirudin with GPI in bail-out scenarios only, i.e., justified by complications arising once intervention is started. In panel B, No=no prior bivalirudin use; <30%=bivalirudin use in less than 30% of patients; ≥50%=bivalirudin use in at least 50% of patients.
Higher cost, as compared to unfractionated heparin, was the single mostly frequently chosen explanation for the limited drug use in clinical practice (71.1%) (Figure 6). Results were consistent in the population stratified by age, country, radial or total PCI volume and bivalirudin use.
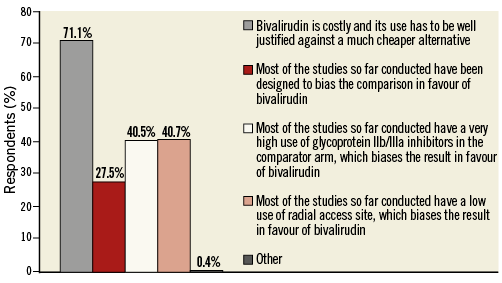
Figure 6. What do you think are the reasons why the use of bivalirudin has been so extensively debated over the last years? (Multiple answers allowed).
Almost half of respondents (45.7%) acknowledged a bleeding benefit conferred by bivalirudin as compared to heparin±GPI, with similar proportions of those who interpreted this reduction as clinical marginal or relevant. Twelve point five percent of respondents believed that bivalirudin decreases both bleeding and mortality and 23.4% were convinced that bivalirudin increases the risk of stent thrombosis without bleeding or mortality benefit. Finally, 18.4% of participants declared that bivalirudin provides a substantial clinical equipoise as compared to UFH at higher costs.
More than 40% of participants were convinced that bivalirudin should be used in patients with a high bleeding risk, irrespective of the access site. However, more than one third declared that the use of bivalirudin is not justified even in patients receiving a transfemoral intervention. These opinions were highly related to the declared bivalirudin use in practice.
CLINICAL SETTING AND OPINIONS OF PARTICIPANTS IN THE POST-ACC SURVEY
The proportion of respondents who declared never having used bivalirudin or having discontinued it after the HEAT PCI study results was higher in the post- as compared to the pre-ACC survey (58.5% vs. 45.9%; p<0.001). Consistent with the pre-ACC survey results, the percentage of Europeans who did not use bivalirudin was significantly higher compared with North Americans (50% vs. 7.7%; p<0.001).
Roughly one third of respondents (35.7%) believed that bivalirudin, as compared to unfractionated heparin, reduces mortality, with significant gradients noted in younger vs. older than 50 years (38.7% vs. 29.2%; p=0.033) (Figure 7A), non-European vs. European (41.3% vs. 30.6%; p=0.010) (Figure 7B), non-interventional vs. interventional cardiologists (59.5% vs. 33.9%; p=0.002) (Figure 7C) and high vs. low or non-bivalirudin users (51.1% vs. 37.7% and 32.1%; p=0.036) (Figure 7D).
Consistent with the pre-ACC survey results, 46.5% of respondents recognised a bleeding benefit of bivalirudin as compared to UFH±GPI; 21.2% believed that bivalirudin increases the risk of stent thrombosis and half of them declared that bivalirudin does not confer any bleeding or mortality benefit. Roughly one quarter of physicians (24.3%) were convinced that bivalirudin provides a substantial clinical equipoise as compared to UFH at higher costs.
After MATRIX, 37.9% of respondents stated that bivalirudin should be used in patients at high risk of bleeding, irrespective of the access site. However, 27.1% declared that bivalirudin should not be used in patients undergoing a transradial intervention, as its value is mainly limited to the reduction of access-site bleeding, and 28.5% declared that bivalirudin use is not justifiable irrespective of the access site. Only 6.5% of respondents believe that bivalirudin reduces mortality irrespective of bleeding benefit, and as such its use should not be affected by perceived bleeding risk or access site. A significant gradient was noted stratifying the population by country, professional figure or bivalirudin use.
The majority of participants (62.5%) reported that the cost reduction of bivalirudin could be the major driver to higher use of the drug in the future. Younger, non-European, non-interventional cardiologists, working at low-volume radial PCI centres or more frequently using bivalirudin, more frequently expressed this opinion (Figure 8).
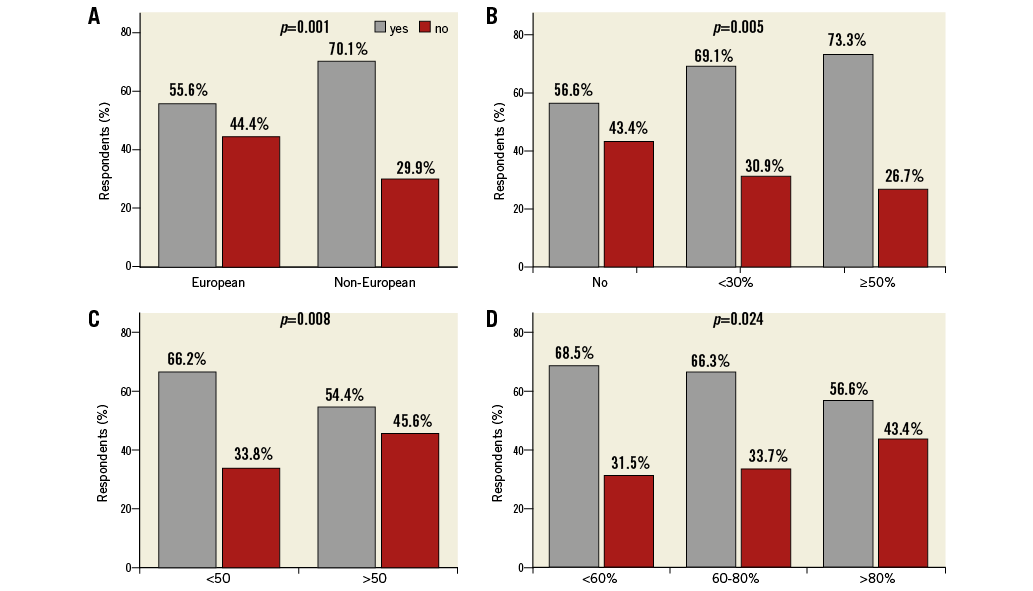
Figure 8. Bivalirudin in Europe will become generic before the end of the year 2015. Do you think that its use may increase in EU given the current evidence against unfractionated heparin? The answers of population stratified by country (A), prior bivalirudin use (B), age (C) and radial PCI volume centre (D) are shown. Yes=I think cost reduction will be a major driver to higher use of bivalirudin against this evidence. No=I think that reduced costs will not increase the use of bivalirudin against this evidence. In panel B, No=no prior bivalirudin use; <30%=bivalirudin use in less than 30% of patients; ≥50%=bivalirudin use in at least 50% of patients. In panel D, radial PCI volume is reported as percentage of transradial PCI performed at the centre in 2014.
Slightly more than one quarter of respondents (27.9%) reported that the anticipated bivalirudin use in the future would increase after MATRIX Antithrombin (Figure 9A) with differences observed between non-interventional cardiologists and interventional cardiologists with less than five vs. interventional cardiologists with more than five or 10 years of experience (40.5% and 34.9% vs. 29.9% and 23.7%; p=0.047) (Figure 9B), non-European vs. European (34.6% vs. 21.8%; p=0.001) (Figure 9C), and physicians working at low or medium volume vs. high-volume radial PCI centres (31.5% and 37.3% vs. 22.1%; p=0.010) (Figure 9D).
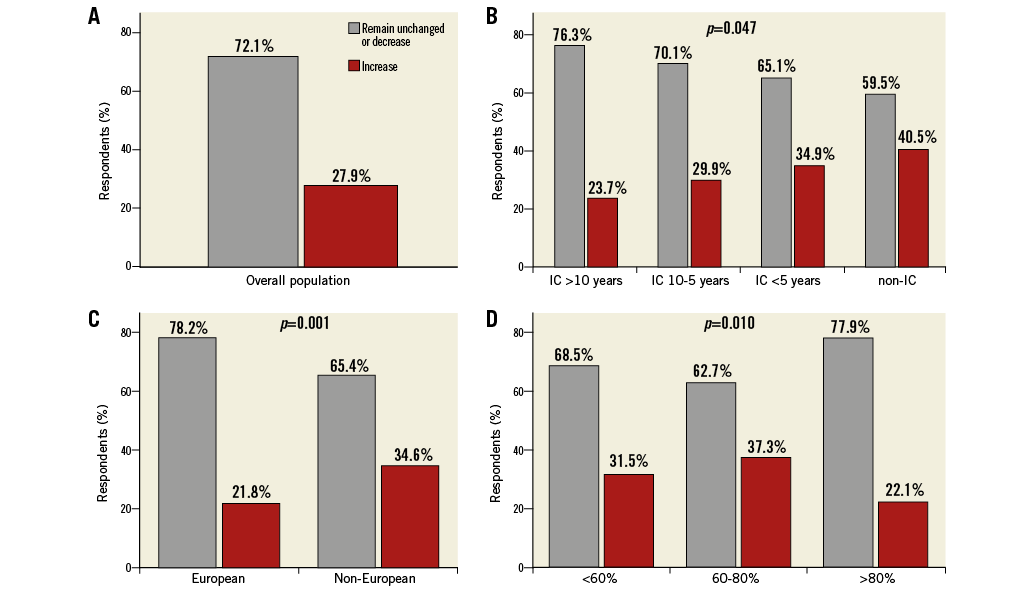
Figure 9. After MATRIX Antithrombin, will your use of bivalirudin remain unchanged or decrease, or increase? The answers of overall population (A) and of population stratified by professional figure (B), country (C) and radial PCI volume centre (D) are shown. In panel B, IC=interventional cardiologist. The interventional cardiologists were stratified according to the years of experience. In panel D, radial PCI volume is reported as percentage of transradial PCI performed at the centre in 2014.
Bleeding and mortality
The vast majority of participants (83.7%) declared that bleeding prevention, irrespective of its mechanism of action, has the potential to reduce mortality in ACS patients as shown by HORIZONS-AMI, OASIS-5 and MATRIX. A notable gradient among respondents based on age (89.3% vs. 84.1% vs. 77.8% in less than 40, between 40 and 50 and more than 50 years, respectively; p=0.018) was observed. Moreover, 15.2% of respondents declared that bleeding is potentially more worrisome for mortality risk than stent thrombosis itself. Among physicians who reported that stent thrombosis is more closely associated with mortality than bleeding, a significant gradient between Europeans and North Americans was noted (42.6% vs. 15.4%; p<0.001).
Interpretation of the survey results
The main findings of this EAPCI survey can be summarised as follows:
– The vast majority of respondents reported the radial approach as the preferred access site for invasive treatment of ACS patients. On the other hand, only 18% declared that bivalirudin is the safest and most effective antithrombin therapy.
– The majority of respondents were convinced that a transradial intervention has potential to decrease mortality mainly by access-site bleeding reduction. Slightly less than 40% of respondents agreed on a possible mortality benefit with bivalirudin.
– The radial approach is most frequently supported by European physicians, younger than 50 years or practising at high-volume radial PCI centres. Non-European –in particular North American– physicians, younger than 50 years, practising at low-volume radial PCI centres or at centres with high bivalirudin utilisation, more frequently endorsed the use of bivalirudin.
– High cost was the most frequently chosen reason to explain the limited use of bivalirudin in current clinical practice. Accordingly, the majority of respondents were convinced that cost reduction could be the main driver to a higher use of bivalirudin in future.
– More than half of the respondents believed that radial benefit is independent of bivalirudin use, whereas roughly 40% were convinced that bivalirudin should be used in high bleeding risk patients irrespective of access site.
– After the MATRIX Access trial:
- An increased proportion of respondents interpreted the evidence on mortality benefit after transradial intervention as definitive.
- Almost half of respondents believed that the transradial approach should be upgraded to a class I recommendation in the guidelines for ACS patients undergoing invasive management.
– After the MATRIX Antithrombin trial:
- Almost 30% of respondents declared that their prior bivalirudin use would increase.
- Roughly one third of participants believed that bivalirudin decreases mortality as compared to UFH.
- Physicians who practise at low-volume radial PCI centres, non-interventional cardiologists, non-Europeans or those younger than 50 years more frequently believed in the mortality benefit of bivalirudin, and they more frequently declared a greater use of the drug in the near future.
– After MATRIX overall study results:
- The vast majority of participants (83.7%) declared that bleeding prevention, irrespective of its mechanism of action, has potential to reduce mortality in ACS patients, and 15.2% of respondents declared that bleeding is potentially more worrisome for mortality risk than stent thrombosis itself.
Limitations
This survey has a number of important limitations which should be carefully weighed when interpreting the results. Firstly, only a small percentage of invited practitioners took part in this survey (3.8% and 5% for pre- and post-ACC survey, respectively); only 59 physicians completed both surveys (10.3% and 7.3% of respondents to pre- and post-ACC survey, respectively); and in the stratified analysis the same subgroups included a very limited number of respondents (i.e., North American). Therefore, the results are not necessarily representative of the whole community. However, low participation rates are a common feature of surveys in general; this survey included participation from a large and potentially representative sample of practising physicians. Secondly, the use of multiple-choice questions may have led to question bias. To reduce this effect, respondents were able to add open answers if they felt it was appropriate. Finally, the second survey was administered after the MATRIX results presentation at ACC 2015 and after MATRIX Access publication. However, the MATRIX Antithrombin results were not yet published in a peer-reviewed journal, which may have negatively affected the proper dissemination of the study results among survey participants.
Conclusions
In this EAPCI survey, the radial approach has emerged as the preferred access site for ACS patients undergoing invasive management with roughly every other responder interpreting the evidence for mortality benefit as definitive and calling for a guidelines upgrade to class I after MATRIX Access. After MATRIX Antithrombin, the most frequently preferred anticoagulant option in ACS patients undergoing PCI remains UFH±GPI. Higher cost was by far the most frequently reported reason for limiting a broader use of bivalirudin in practice. Only a minority of participants interpreted the evidence for a possible mortality benefit conferred by bivalirudin as definitive, whereas 30% of them declared their use of the drug would increase in the future especially in high bleeding risk patients undergoing transfemoral intervention. Finally, the vast majority of participants declared that bleeding prevention, irrespective of its mechanism of action, has potential to reduce mortality in ACS patients, and roughly one participant out of six declared that bleeding is potentially more worrisome for mortality risk than stent thrombosis itself.
|
Impact on daily practice According to this European Association of Percutaneous Cardiovascular Interventions (EAPCI) survey, the evidence for a mortality benefit of transradial as compared to transfemoral intervention in ACS patients undergoing invasive management is largely reinforced by the results of the MATRIX Access trial. One participant out of every two believes there is no need for additional studies to prove the superiority of the radial over the femoral approach and calls for a class I upgrade within guidelines. On the other hand, the cardiology community largely embraces UFH as the preferred anticoagulant. While acknowledging a bleeding benefit conferred by bivalirudin as compared to UFH, higher costs and concerns for greater thrombotic risk limit a broader use of the former over the latter in practice. |
Acknowledgements
The authors would like to express their gratitude to the staff of Europa Organisation/EuroPCR for the support given during the survey development.
Conflict of interest statement
The authors have no conflicts of interest to declare.