Abstract
Aims: To investigate the consequences of inflating low-pressure balloon occlusion devices in native coronary arteries.
Methods and results: One hundred eighteen segments of 118 patients who were enrolled in the ASPARAGUS study were analysed post-procedure and at six months by means of quantitative coronary angiography. ASPARAGUS was a randomised study to assess the efficacy of the PercuSurge GuardWire system in acute myocardial infarction. Patients were divided into two groups; protection group (group P, n=53) and control group (group C, n=65). Matched 15 mm segments were selected for quantitative coronary angiographies using anatomical landmarks post-procedure and at six months. There were 118 matched QCA analysis (Group P 53, Group C 65). Baseline characteristics were similar between groups. The mean minimal lumen diameter (MLD) post procedure was 1.94±0.57 mm in group P and 1.92±0.57 mm in group C. The MLD at six months was 1.98±0.54 mm in group P and 1.92±0.54 mm in group C. There was virtually no late loss in both group (P: –0.04±0.38 mm, C: 0.00±0.38 mm, p=0.561).
Conclusions: The inflation of the low-pressure PercuSurge balloon in native coronary arteries was not associated with angiographic vascular response during the 6-month follow-up. This finding may suggest the safety of using similar technology such as the low-pressure balloon system in human native coronary arteries.
Introduction
Distal embolisation or slow flow/no reflow phenomenon following percutaneous coronary intervention (PCI) may result in extending myocardial damage and worsening prognosis1-3. Previous studies have demonstrated that a distal protection device is useful in reducing complications of slow flow/no reflow in PCI for saphenous vein graft4. However, the safety of inflating low-pressure balloon devices in native coronary arteries remains to be determined. This issue has become more relevant, as the number of devices using such technique is increasing (i.e., optical coherence tomography (OCT), angioscopy and proximal protection use occlusion balloons5-9).
However, few data are available regarding the vascular response to low-pressure balloon inflation injury of protection device10. The safety of inflating low-pressure balloons in native coronary arteries remains to be confirmed in large prospective studies. The purpose of this study is to determine the angiographic vascular response of the inflated segments of the protection balloon.
Method
Study patients
Consecutive angiograms of ST-segment elevation myocardial infarction (STEMI) patients, enrolled in the ASPARAGUS (ASPirAtion of LibeRated debris in Acute myocardial infarction with GUardWire Plus™ System) trial, were reviewed for this analysis. The ASPARAGUS trial was designed as a prospective, multicentre, randomised study in 341 patients to compare the effects of two procedures (stenting with and without the GuardWire Plus™ distal protection device). The enrolment criteria of this study included: (1) age >18 years, (2) STEMI within 12 hours from the onset of chest pain, (3) native coronary artery culprit lesions. Reperfusion was conducted by stenting. The exclusion criteria included: (1) culprit lesion in left main tract (LMT) disease or saphenous vein graft, (2) reference diameter of <2.5 mm, (3) patients with cardio-pulmonary arrest. Therefore, randomisation was performed after the initial coronary angiography (CAG). The study was conducted according to the principles of the Declaration of Helsinki. All patients gave written informed consent before the catheterisation.
There were 118 cases with matched post- and follow-up angiogram.
Procedure protocol
After confirmation of patient eligibility by CAG, the use of distal protection was randomly determined by sealed envelope. GuardWire Plus™ (Medtronic Corp., Santa Rosa, CA, USA) was employed as the only distal protection device. This distal protection wire consists of a 190 cm long, 0.014 inches nitinol hypo tube guidewire with a central lumen connected to a distal, low-profile compliant sphere occlusion balloon which is available in diameter from 3 to 6 mm. This distal occlusion balloon is inflated or deflated easily by using the micro-inflator, which is a dedicated inflation device for this balloon, and diluted contrast. Dye injection is used to make sure the distal flow is totally occluded. In the protected group (Group P), GuardWire Plus™ was inserted into the distal coronary artery, either directly or after first crossing with a standard steerable guidewire. The distal protection was performed before stent placement, and the occlusion balloon was inflated by 3-6 mm in line with the coronary vessel diameter to block the coronary flow. This balloon needs to be inflated until the shape of the balloon changes just from spherical to elapsed shape in order to block the coronary flow with minimal size. After coronary occlusion, balloon dilatation and stent implantation were performed per operators’ discretion. An export catheter was inserted while the coronary flow was blocked and 20-60 ml of blood was manually aspirated to remove the debris liberated from the coronary lesions. The procedure was completed when coronary flow was restored. In the control group (Group C), PCI was performed without using GuardWire Plus™.
Aspirin at 81-100 mg daily and ticlopidine 200 mg daily for at least two weeks was the Japanese standard postoperative antithrombotic regimen. Heparin use during PCI was mandatory, although the dose was decided at the operator’s discretion. IIbIIIa inhibitors was not available in Japan.
Data analysis and management
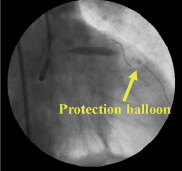
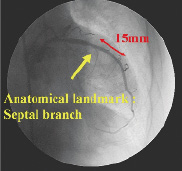
Clinical data were collected in-hospital, at 30 days and at six months. Quantitative coronary angiography (QCA) of the target segments was performed post procedure and at 6-month in both groups. In order to determine the impact of the distal protection balloon, matched 15 mm coronary segments were selected using anatomical landmarks (such as side branches, or calcifications) post-procedure and at six months using the same projection. In group P, we identified the site where the protected balloon was inflated from the baseline angiography. In group C, we defined the site where we would have placed the occlusion balloon. Then we tried to find an anatomical landmark proximal to the site (Figure 2 A, B, C). A 15 mm segment from this proximal anatomical landmark was selected as an analysed segment. At follow-up, we were able to select the matched 15 mm segment with the baseline angiogram using the same anatomical landmark. Minimal lumen diameter (MLD), reference diameter (RD), late loss and lesion length in the analysed segment were compared in the same view during post-procedure and at 6-month. QCA analysis was done using QCA-Cardiovascular Measurement System (CMS), version 5.1.
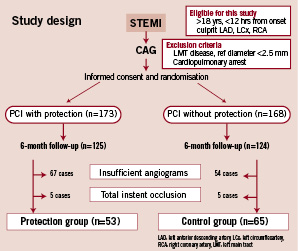
Figure 1. Flow chart of this study.
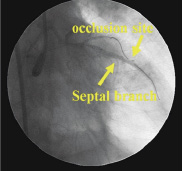
A
B
C
Figure 2. A) Marker of occlusion balloon was seen in left anterior descending artery. B) As a landmark, the septal branch would be useful in this case. C) 15 mm segments including protection site were selected using anatomical landmarks.
Statistical analysis
Data are expressed as the mean value±standard deviation or number (%) of the patients. Statistical analysis was performed using Dr. SPSS (SPSS Inc., Chicago, IL, USA) for windows software.
Results
A total of 65 segments in group C and 53 in group P were analysed. Patient characteristics were shown in Table 1. There were no significant differences between the groups with respect to baseline patient characteristics. Mean age in group C was 65 years old, and in group P was 62. Male patients represented 75% of patients in group C, and 81% in group P. Target vessel characteristics were similar in both groups (Table 2). Angiographic results were shown in Table 2. In group C, MLD was 1.92 mm both post procedure and at six month follow-up. The late loss in group C was nearly zero. Stenosis >50% at follow-up was observed only in one case in group C. In group P, MLD changed 1.94 mm to 1.98 mm during six month follow-up. The late loss was –0.04 mm. There was no segment that developed stenosis >50% in group P. No difference was observed between both groups in terms of the late loss and% diameter stenosis (Table 2, Figure 3 A&B).
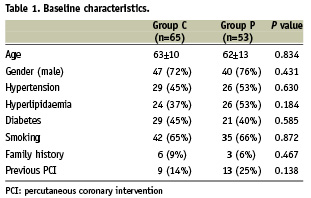
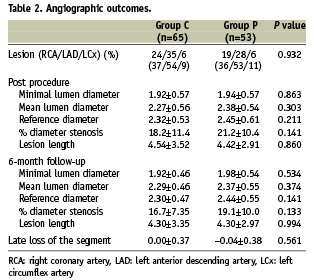
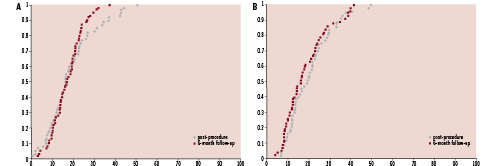
Figure 3. A) Cumulative distribution curves of the% diameter stenosis of protected segments in group C at 6-months. B) Cumulative distribution curves of the% diameter stenosis of distal to the lesions in group P at 6-months.
Discussion
This report describes the angiographic follow-up of the segments inflated by the occlusion balloon. In the GuardWire Plus™ system, it is inevitable that the occlusion balloon is inflated at the distal to the culprit lesion in order to block the coronary flow. It is well known that therapeutic balloon inflation injures the vessel wall, and may cause restenotic response. Wu et al has reported that the distal protection sites of GuardWire Plus™ developed significant stenosis in three cases10. Our results demonstrated that the inflated segments of the protection balloon did not cause late loss or coronary events during 6-month follow-up. These results may be explained by the following: First, the occlusion balloon in the GuardWire Plus™ is round, and the contact area to the vessel wall is very small. The damaged area caused to the vessel may be smaller than that of the PTCA balloon. Second, in this system, the occlusion balloon is inflated by approximately 1 atmosphere, so the damage to the vessel wall may be minimal. Previous work has shown that low pressure dilatation may reduce arterial trauma with subsequent lower restenosis, even in stenosed segment11. If we can diminish arterial trauma in the non-stenosed segment, restenotic response should be decreased, since the damage to the arterial wall caused by the low-pressure balloon inflation might be less in such non-stenosed segments than in a diseased segment. Third, those segments inflated by the occlusion balloon which appeared to have progressive obstruction had initial angiographic findings. In addition, coronary endothelium damage by low-pressure coronary devices does not necessarily lead to morphological changes if it is not accompanied with severe local vessel trauma12. Thus, if we avoid deploying the occlusion balloon in a diseased segment, and also select appropriate size for avoiding overstretching of the vessel, the frequency of late significant stenosis at the inflated segment would be small. From this point of view, further studies using intravascular ultrasound (IVUS) or OCT may be required to clarify the degree of restenotic response and long-term influences caused by the protection balloon, since minor injury induces the proliferative response at the sites of atherosclerotic plaque.
Limitations
This study has a several limitations. First, it is a retrospective study. Second, the occlusion sites are varied by the operators. Third, there were some cases that where late loss could not be analysed because the coronary angiograms did not include the protected segments. As a result, the sample size was relatively small compared to the number of patients enrolled in the ASPARAGUS trial.
Conclusion
The protection balloon of the GuardWire Plus™ wire system causes no significant late loss during the 6-month follow-up. This finding may suggest that distal protection system using occlusion balloon has no evident detrimental effect on the inflated segments of stented coronary lesions, reassuring the use of other devices with low pressure balloon occlusion.
Acknowledgements
The authors are grateful to Professor Hideki Hashimoto at Tokyo University, for his statistical assistance.

