I haven’t been back to the United States since 2020, before the pandemic and the start of all those restrictions on our freedom to travel. Anyone who has travelled in the last two years knows that every departure has seen an increase in the coefficient of logistical difficulty, taking into account COVID-19 testing, the online forms that need to be filled out, the printed ones you need to show and, in some cases, even the quarantine that needs to be foreseen. The restrictions, however, were not only practical but also psychological, given that, on top of all these travel difficulties, there remains the feeling of risking something every time you are exposed to encounters in confined spaces such as on an aircraft. But can we resist the urge to travel, even in the era of digital conferences? Certainly not, and Ron Waksman and the Cardiovascular Research Technologies (CRT) organisation must be acknowledged for having focused courageously and decisively on restarting face-to-face meetings, precisely in the place where everything had stopped, Washington, D.C.
CRT 2022 was all it needed to be and in a certain sense indistinguishable from their editions prior to 2020 – that is, except for the comforting use of masks by all the participants. And here we were again, grappling with the countless face-to-face sessions, eight-minute lectures, racing from room to room, “VIP watching”, networking, and following late-breaking trials. It was as if the last two years had been a bad nightmare, as if time had stopped. And in a certain sense it had stopped all right, since so many of these sessions and so many of these topics could have fit just as well in a 2020 session, considering the general slowdown in science and studies over the last two years. So, the questions were “where were we?” or “where did we leave off?”, both useful in order to reset and start again.
I had numerous doubts before leaving (“What if I catch COVID-19 in the United States and am not able to return to my country for a while?”), but I also became more certain that if I didn’t go, I would have regretted it. Because after travelling again, finally being overseas was simple, both logistically and psychologically, just as it was two years ago, before the world had changed. A great thanks is due to Ron Waksman for believing it and, recently, to the American College of Cardiology (ACC) organisers for the same reason, and for showing us that yes, the system of medical conferences can indeed start again.
Next month it will be our turn, and the Palais des Congrès of Paris will reopen its doors, giving us a EuroPCR transformed by these past events, but no less vital and eager to restart. To celebrate this “rebirth”, we are preparing a special issue of EuroIntervention to accompany EuroPCR, but beware: the current issue too is no exception to our tradition and full of great articles, as I will immediately illustrate in what follows.
In this issue our mini focus concerns left main revascularisation. Robert-Jan van Geuns, Keith G. Oldroyd and colleagues present the IDEAL-LM randomised trial. The continued evolution in stent technology both in their design and types of biodegradable coating have led to lower rates of repeat revascularisations and could allow for shorter dual antiplatelet therapy (DAPT) duration, post-percutaneous coronary intervention (PCI). This trial compared long-term clinical outcomes after implantation of a biodegradable polymer platinum-chromium everolimus-eluting stent (BP-PtCr-EES) followed by 4 months of DAPT compared to a durable polymer cobalt-chromium everolimus-eluting stent (DP-CoCr-EES) followed by 12 months of DAPT in patients undergoing PCI of unprotected left main coronary artery disease (LMCAD). While BP-PtCr-EES was shown to be non-inferior to BP-PtCr-EES, due to lower than predicted event rates, the trial remained underpowered. This article is accompanied by an editorial by Gregg W. Stone and Chandrashekar Bohra.
Continuing with our mini focus, from the SYNTAXES study, authors Hironori Hara, Patrick W. Serruys and colleagues examined the association of preprocedural biomarkers on long-term survival in patients treated for de novo three-vessel disease and/or LMCAD either percutaneously or by surgery. At 10-year follow-up, the predictive importance of creatinine clearance was seen, together with high preprocedural C-reactive protein and low haemoglobin, regardless of the revascularisation technique. Statin therapy was associated with decreased risk of mortality no matter what the preprocedural lipid profile was. Similarly, HbA1c, when diabetes was properly controlled, was not predictive of 10-year mortality underlining the importance of pharmacological treatment. This article is accompanied by an editorial by Martha Gulati and Sonya Burgess.
Also in the coronary section, Alexandra N. Nowbar, Rasha Al-Lamee and colleagues present the design of the ORBITA-2 trial, developed to assess the efficacy of PCI on angina frequency in patients with single- or multivessel disease with no antianginal therapy. This new trial will use patient-oriented innovations such as daily symptom reporting using a smartphone application and offer researchers the possibility of proving the efficacy of PCR in these patients, as well as recognising predictors of the placebo-controlled effect of PCI.
The international FAST II study evaluated the accuracy of calculating fractional flow reserve (FFR) using 3D quantitative coronary angiography comparing it to pressure wire-based FFR. Authors Kaneshka Masdjedi, Joost Daemen and colleagues found the vessel FFR technique to offer an equal diagnostic performance to wire-based FFR while offering the possibility of a less invasive choice in making haemodynamic assessment of lesions.
Treating complex calcified coronary lesions often requires the use of rotational atherectomy (RA), but the specific lesion characteristics that would require its use have not been fully defined. This was the aim of the research presented in an article by Sean Fitzgerald, Mohamed Abdel-Wahab and colleagues, who developed an independently validated angiographic scoring tool to predict the need for rotational atherectomy involving four lesion characteristics: lesion length, bifurcation lesion, severe calcification and tortuosity greater than 45°.
Transaxillary access has become a common alternative to transfemoral transcatheter aortic valve implantation (TAVI). In this article, authors Christine J. Chung, James M. McCabe and colleagues studied whether there was a difference in outcomes when performing transaxillary access TAVI using percutaneous access as opposed to surgical cutdown. They observed that while the rates at 30 days of all-cause mortality and stroke were similar, there were differences. For instance, patients undergoing percutaneous access were more likely to receive conscious sedation, had less need for the intensive care unit, and experienced higher rates of major vascular complications, though not life-threatening bleeding.
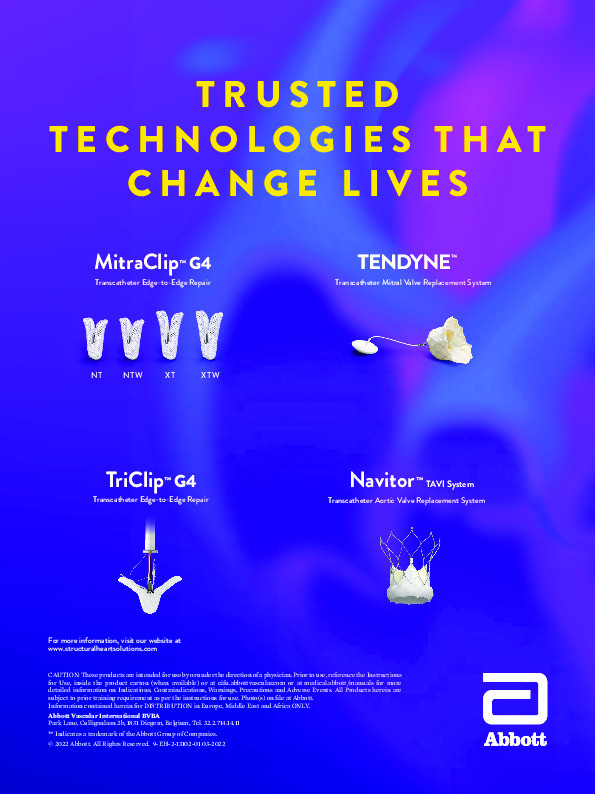
In a research letter, authors Mario Gössl, Paul Sorajja and colleagues looked at outcomes using the novel Tendyne valve (Abbott Structural) in patients with mitral regurgitation linked to severe mitral annular calcification. Early outcomes were relatively promising with noted clinical improvement, but the high mortality rate calls for careful patient selection when using this device.
Finally, in the field of hypertension and stroke Kolja Sievert, Horst Sievert and colleagues looked at the first interatrial septal occluder with a bioresorbable framework, the Carag device. In a research letter, they found the Carag to be safe for use in small to medium atrial septal defects (ASD) as well as in patent foramen ovale (PFO), with no late complications for either of these. Further studies, in larger ASDs and PFOs are needed, with the possibility of looking towards possible device modifications.
Now, let’s turn to the articles themselves.
Supplementary data
To read the full content of this article, please download the PDF.