Introduction
In congenitally corrected transposition of the great arteries (CCTGA) the right ventricle (RV) is the systemic ventricle. RV dysfunction and significant regurgitation of the systemic tricuspid valve are common and associated with worse outcomes. Management of tricuspid regurgitation (TR) in CCTGA is challenging. In acquired cardiovascular disease, percutaneous repair of mitral valve regurgitation (MR) is established. Data on CCTGA with TR are limited1. We report our experience with this technique in these patients.
Methods
CCTGA patients with moderate-severe TR were eligible if surgery was deemed high-risk. Interventional therapy was offered, and patients provided written informed consent. Percutaneous TR repair was performed according to protocols for MR repair. In two patients (dextrocardia n=1, situs inversus n=1), clip insertion was performed 180° counter-clockwise. Transoesophageal echocardiography (TOE) served to localise the implantation site, and confirmed the correct grasping of the leaflets and appropriate TR reduction. At the site of the maximal regurgitation jet the first clip was placed (4/6 anteroseptal, 2/6 posterior septal leaflet). If no satisfactory reduction was achieved, another clip was placed (1/6 posterior septal, 2/6 anteroseptal leaflet). Procedural success was defined as TR reduction of at least one grade or to TR grade ≤2.
This study complied with the Declaration of Helsinki and was approved by the local ethics committee.
Results
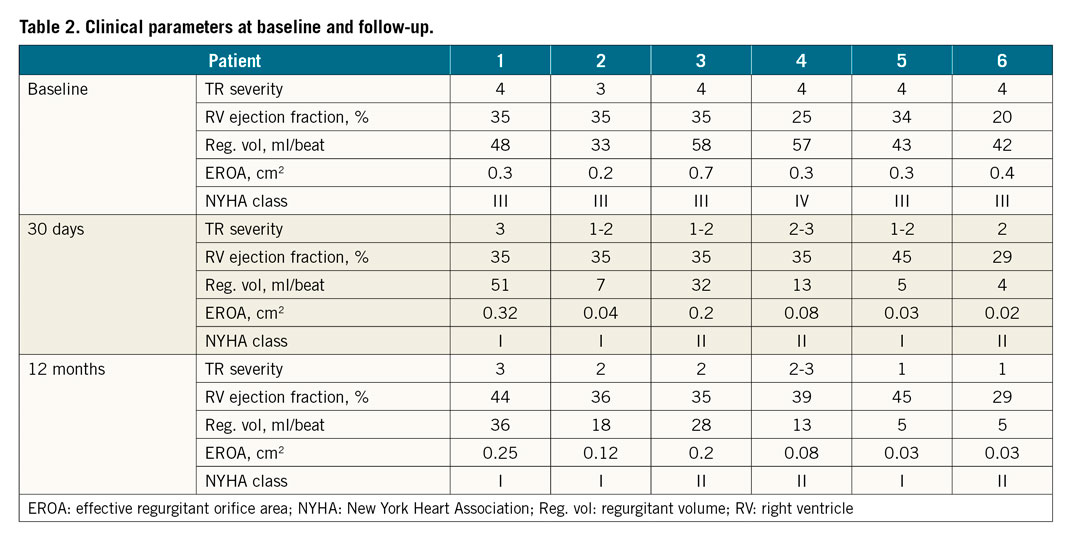
Between June 2016 and January 2018 six patients were included (Table 1). Percutaneous repair of TR was safe and successful in all (Figure 1). A reduction to TR grade ≤2 was achieved in five patients and to 3 in one, in whom further reduction was not possible due to leaflet abnormalities. The procedure time was longer than for percutaneous MR repair due to the complex anatomy.
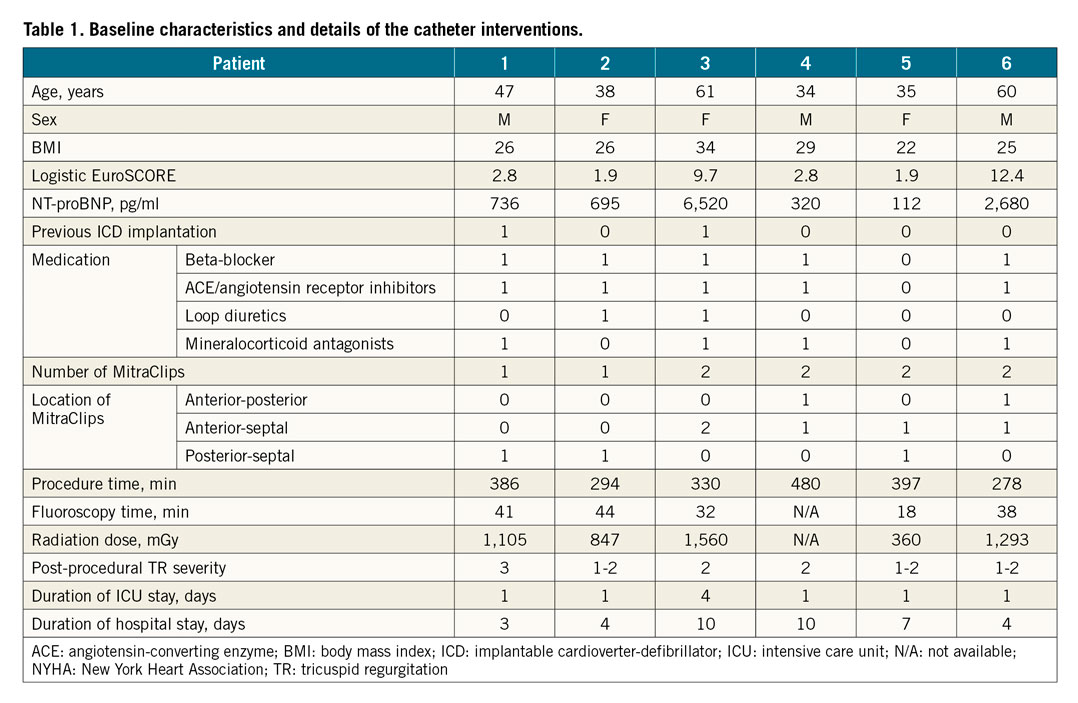
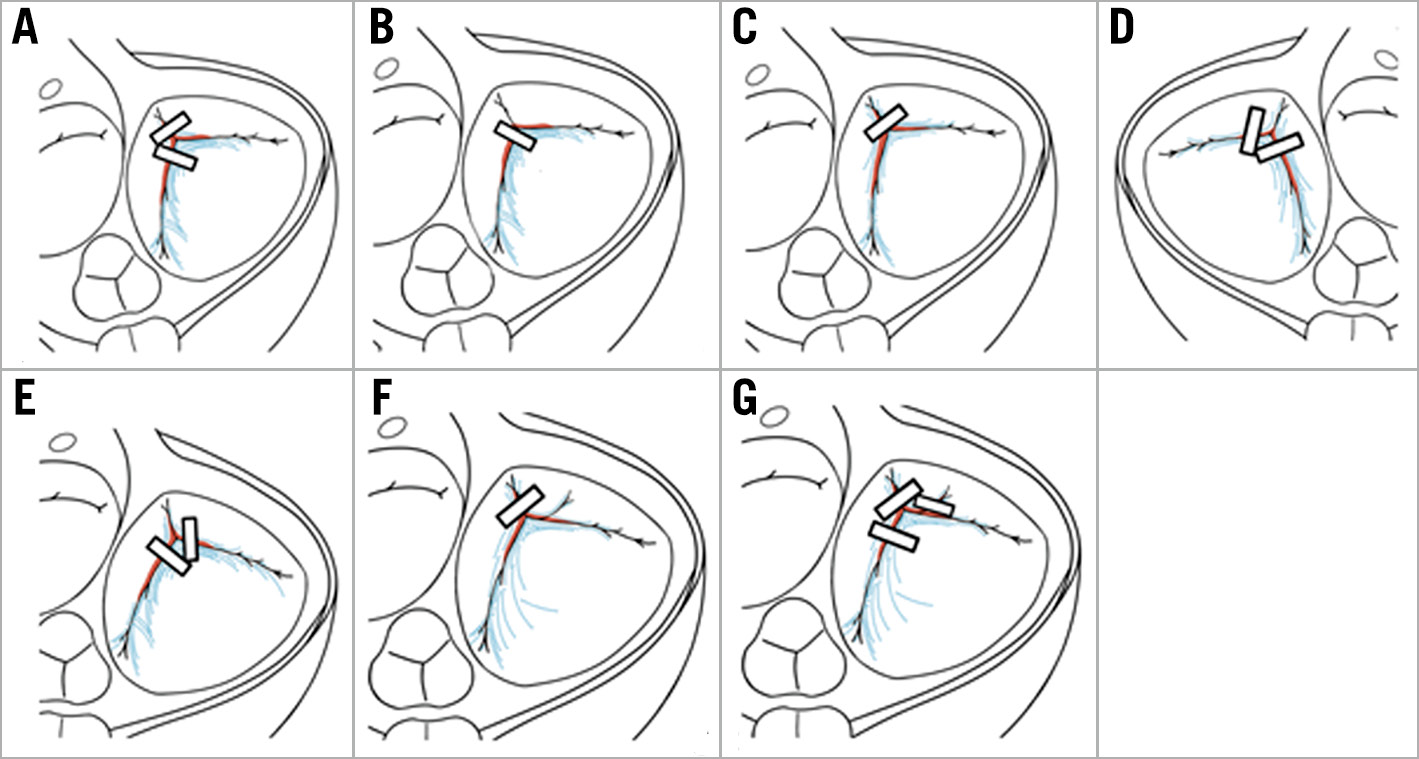
Figure 1. MitraClip positions in six patients (A-F). One patient had a reintervention (initial procedure shown in panel F, reintervention in panel G).
After twelve months, severe TR reoccurred in one patient and two additional MitraClips (MitraClip®; Abbott Vascular, Santa Clara, CA, USA) were implanted to close a posterior leaflet cleft and stabilise the initial clip with TR reduction to grade 3. After one week, partial leaflet detachment occurred. Surgery was not an option, and the patient was treated medically. NYHA class at baseline was ≥III in all patients and improved to ≤II in all (Table 2).
Discussion
Percutaneous repair of TR is feasible in CCTGA, and provides a reduction in TR severity and heart failure symptoms over a one-year follow-up.
Treatment with the MitraClip has already shown promising results for TR in acquired cardiovascular disease2. Additionally, the safety and efficacy of a modified TriClip™ (Abbott) system has been demonstrated3. Data regarding percutaneous repair of TR in CCTGA are limited1. In our cohort, it was feasible. The majority of patients showed an improvement in NYHA class and reduced TR severity. Interestingly, RV ejection fraction improved, as reported in patients with MR and reduced left ventricular ejection fraction4. Whether this translates into a long-term improvement remains speculative. However, it is reassuring that RV function did not deteriorate.
The timing of intervention for severe TR is crucial in CCTGA, since ventricular dysfunction and TR are determinants of outcome. Valve repair is often not feasible, while valve replacement can be associated with significant mortality if severe RV dysfunction is present5. Other treatment options include pulmonary artery banding and cardiac resynchronisation therapy, with limited and sometimes divergent evidence6. Often, only heart transplantation remains. An interventional approach could provide a much needed alternative.
The use of the MitraClip on the tricuspid valve aims to clip together two of the three leaflets to create a double orifice. The choice of leaflets depends on the location of the regurgitation jet and ease of imaging. Optimal grasping views may require significant modifications of standard TOE views. 3D-TOE imaging is helpful for positioning and orientation of the clip, but the leaflet insertion/grasping attempts require 2D imaging or X-plane mode due to the better image and temporal resolution. Nevertheless, leaflet insertion may be difficult to assess. Moreover, the use of multiple clips may be required.
Limitations
Limitations of our study are the small number of patients and the fact that exercise tests were not performed in all.
Conclusions
Percutaneous valve repair with MitraClips is safe and feasible in CCTGA with severe TR. Optimal timing and long-term outcome need to be studied. It should be reserved to centres experienced in both congenital heart disease and transcatheter valve repair.
|
Impact on daily practice In CCTGA with severe TR, percutaneous edge-to-edge repair is safe, feasible and effective. This might open the door to interventional treatments of atrioventricular valve regurgitations in adult congenital heart disease. |
Conflict of interest statement
P.M. Rumpf reports lecture fees from Abbott and proctor fees from Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.