Introduction
Coronary artery fistulae (CAF) represent an abnormal communication bypassing the myocardial capillary bed between a coronary artery and either a cardiac chamber (coronary-cameral CAF) or a vascular structure from systemic or pulmonary circulation (coronary-vascular CAF). CAF represent a congenital anomaly in 0.2% of the population, but are more frequently found in heart transplant recipients (8%), mostly as coronary-right ventricle (RV) CAF caused by endomyocardial biopsy used for monitoring of rejection1,2. Other complications of myocardial biopsy include perforation of the RV wall and tricuspid valve damage2. Several case reports have shown successful transcatheter closure of CAF3,4. We aimed to analyse the indications for transcatheter closure and the long-term prognosis of CAF in heart transplant recipients.
Methods
All patients aged ≥18 years who were transplanted at the Erasmus Medical Center, Rotterdam, from the start of the heart transplantation (HT) programme in June 1984 until January 2018 were included in the study. Clinical data after transplantation were prospectively collected from the start from clinical records and office visits with permission from the patients. The institutional board approved the use of anonymised data for the present study.
Rejection was monitored by endomyocardial biopsy obtained percutaneously. All biopsies were performed on the RV septum under fluoroscopic guidance using a 50 cm Jawz™ 2.2 mm bioptome (Argon Medical Devices, Frisco, TX, USA) inserted through a 7 Fr sheath placed into the right internal jugular or right femoral vein. In the first decade of the HT programme each patient underwent 30 to 40 biopsies, while in the last decades the number of biopsies decreased to 15 to 20 for each patient. Coronary angiography (CAG) was performed per protocol every year until 1990. After 1990, CAG was performed at the 1st year and the 4th year after transplantation. Thereafter, patients annually underwent single-photon emission computed tomography (SPECT) for assessment of ischaemia, or cardiac CT angiography. Follow-up CAG was only performed in case of ischaemia. All coronary angiograms were reviewed independently by two cardiologists. The incidence of CAF to the RV was calculated from all heart transplant recipients who had at least one CAG.
STATISTICAL ANALYSIS
Data were analysed using SPSS software, Version 17.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean±standard deviation (SD) and were compared using the Student’s t-test. Non-parametric variables were compared using the chi-square test. Cumulative survival was estimated according to the Kaplan-Meier method and compared using the log-rank test; p<0.05 was considered statistically significant.
Results
From a total of 711 heart transplant recipients, there were 565 adult patients who underwent at least one CAG and were included in the analysis. Forty-one patients (7.3%) had coronary-RV CAF. The clinical characteristics of the transplanted patients with and without CAF are presented in Table 1. There was no difference in the age of the recipient or the donor, the number of rejection episodes, coronary allograft vasculopathy and development of heart failure between the two groups. Of the eight cardiac deaths in the group of patients with CAF, seven were due to cardiac allograft vasculopathy, while one death was caused by severe aortic valve stenosis.
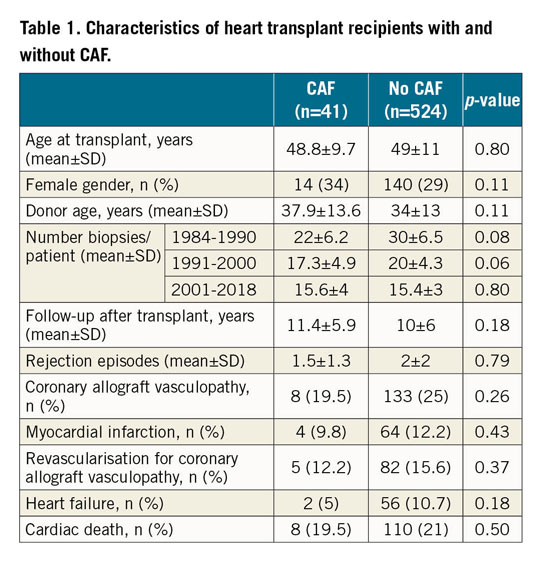
The anatomic distribution of CAF is presented in Figure 1. Of the four untreated fistulae originating from the left anterior descending (LAD) artery, two remained unchanged, while two disappeared at follow-up due to cardiac allograft vasculopathy. The characteristics of the individual patients with CAF from the LAD who underwent transcatheter intervention are presented in Table 2. Moving image 1 and Moving image 2 show transcatheter closure of CAF in patient 7. CAF closure by covered stent or coils for myocardial ischaemia preserved the patency of the LAD during a follow-up of 10±4 years. The survival of patients with CAF was not different from the whole HT cohort (Figure 2).
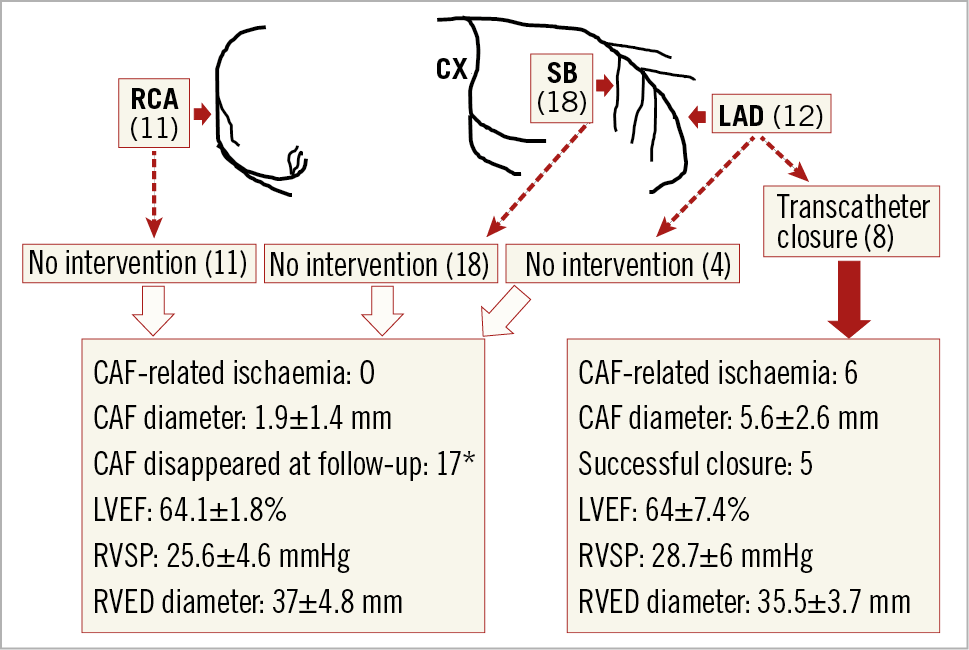
Figure 1. Distribution of CAF (number of patients) and treatment. *Follow-up CAG was performed in only 27 patients in the No intervention group. CX: circumflex coronary artery; LVEF: left ventricle ejection fraction; RVED diameter: right ventricular end-diastolic diameter at the tricuspid annular plane; RVSP: right ventricular systolic pressure, measured by right heart catheterisation; SB: septal branches
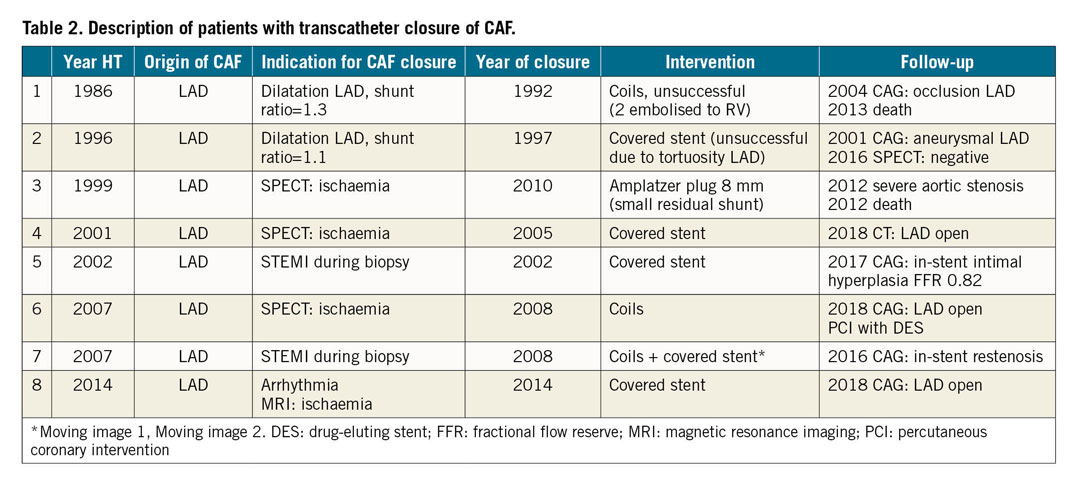
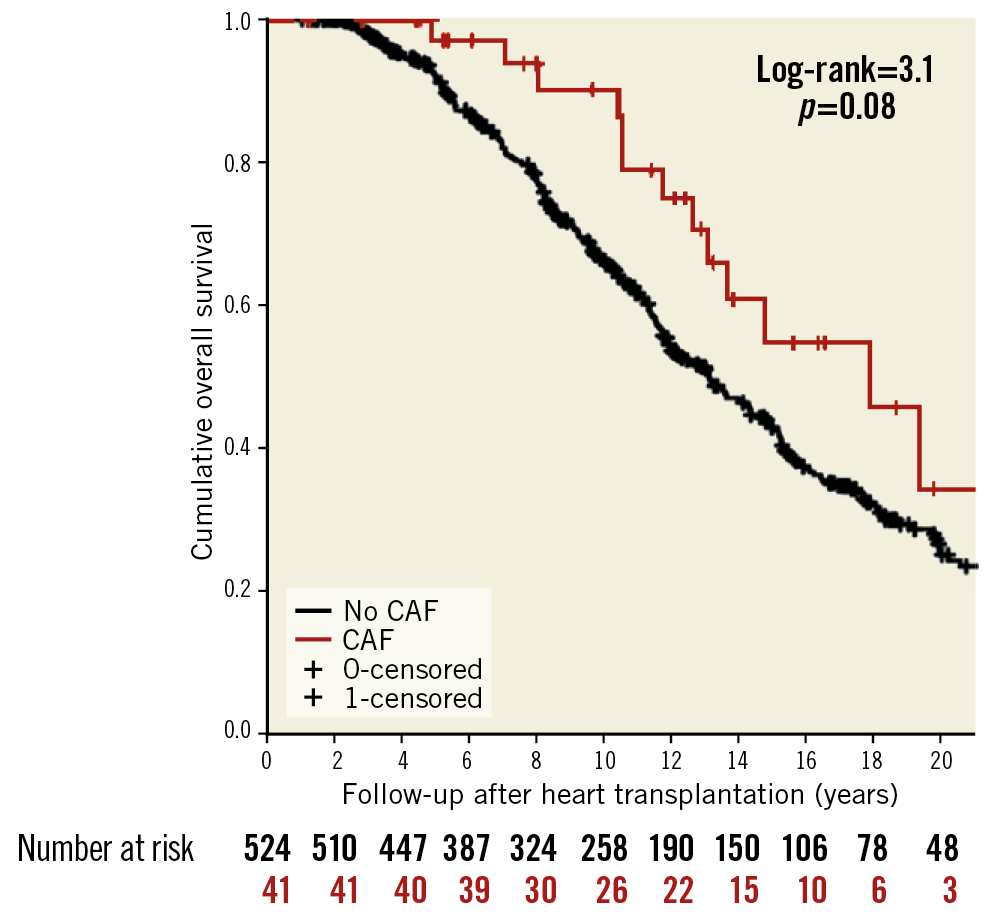
Figure 2. Cumulative overall survival of patients with CAF and without CAF.
Discussion
Although the incidence of coronary-RV CAF was 7.3%, CAF-related clinical events occurred in only six patients (1%), caused by impaired perfusion of the distal LAD. Fistulae originating from the LAD could be clinically diagnosed by the presence of a continuous cardiac murmur peaking in diastole.
Historically, right-sided volume overload due to left-right shunt, myocardial ischaemia, and aneurysmal dilatation of the proximal coronary artery were potential indications for CAF closure3,4. In the first decade of the transplantation programme at our centre, the indication for transcatheter closure was progressive dilatation of the proximal LAD. However, in the absence of ischaemia, the need for CAF closure is questionable as many fistulae disappear at follow-up due to either a small calibre or development of coronary allograft vasculopathy. Even when CAF from the LAD persisted in some patients in the long term, they did not develop RV failure. Two patients with CAF developed heart failure with preserved ejection fraction due to cardiac allograft vasculopathy.
Limitations
Follow-up CAG was not available in all patients with CAF. Left-right shunt measurement was performed in only a few patients, which hampered the evaluation of CAF haemodynamics. The low number of CAF did not permit a multivariate analysis to detect risk factors.
Conclusion
The majority of CAF after HT are asymptomatic. Transcatheter closure is indicated for myocardial ischaemia and to maintain the coronary patency in the long term. Overall CAF does not affect survival after heart transplantation.
|
Impact on daily practice Transcatheter closure of CAF is indicated for myocardial ischaemia due to coronary steal. The long-term outcome after heart transplantation is not affected by the presence of CAF. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Coronary-RV CAF in patient 7.
Moving image 2. CAF closure by coils and covered stent.