Knock, knock. Who is there? Me, Ms. Transcatheter Aortic Valve looking for low-risk patients, can I come in? Okay… but we are not ready (yet). Well, I am coming…
The updated European1 and American2 guidelines for patients with valvular heart disease support transcatheter aortic valve implantation (TAVI) for patients who are at intermediate risk for surgical aortic valve replacement (SAVR), or who have other risk factors not captured by the preprocedural risk scores such as frailty, porcelain aorta, hostile chest/radiation1,2. While the American2 guidelines place a class I recommendation for SAVR and a class IIa recommendation for TAVI, the European guidelines1 place a class I recommendation for TAVI, and stress the benefits of transfemoral access in elderly patients1.
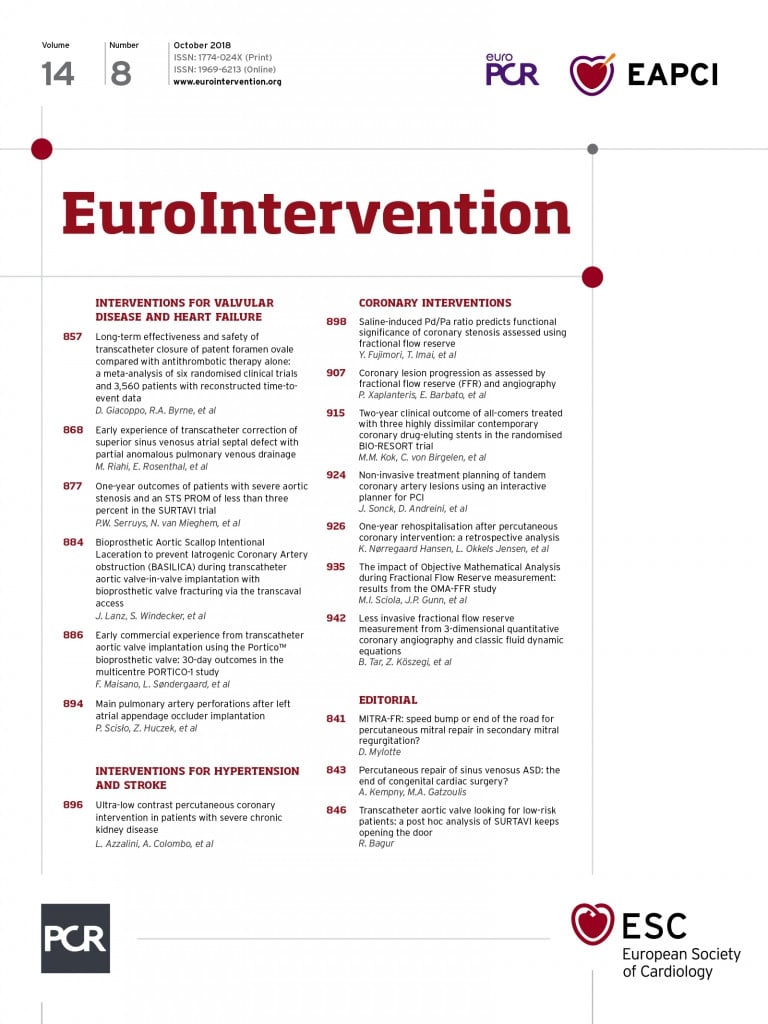
Guidelines recommend SAVR as class I in patients at low risk (and who have no other risk factors not included in the scores)1,2. In this issue of EuroIntervention, Serruys and colleagues3 report the one-year outcomes of patients with a Society of Thoracic Surgeons (STS) score <3% enrolled in the Surgical Replacement and Transcatheter Aortic Valve Implantation (SURTAVI) trial4.
Overall, SURTAVI showed that TAVI was statistically non-inferior to SAVR in intermediate-risk patients4. The present post hoc analysis risk-stratified patients (for clinical relevance) into three strata: STS <3% (TAVI=131, SAVR=123), STS 3-5% (TAVI=480, SAVR=405), and STS ≥5% (TAVI=253, SAVR=268)3. In the stratum of STS <3%, the primary outcome of all-cause death or disabling stroke was significantly lower in TAVI as compared to SAVR (1.5% versus 6.5%, p=0.042), whereas similar results were observed in the STS 3-5% and STS ≥5% strata. Likewise, no statistical significance was observed when analysing all-cause mortality or disabling stroke separately across the three strata. Importantly, lower-risk patients had more valve reintervention: STS <3% (4.6% versus 0.9%, p=0.071), STS 3-5% (1.9% versus 0.3%, p=0.024), and STS ≥5% (0.8% versus 0.8%, p=0.949).
ARE LOWER-RISK PATIENTS THE SAME AS YOUNGER PATIENTS? PROBABLY, BUT NOT ALL
The Nordic Aortic Valve Intervention (NOTION) trial was the first to randomise all-comer lower-risk patients (n=276) to TAVI with the CoreValve® (Medtronic, Minneapolis, MN, USA) or SAVR5. The mean age was 79 years, mean STS score 3.0±1.7%, and 82% of patients had an STS score <4%5. No differences were observed between TAVI and SAVR in the composite endpoint of all-cause mortality, stroke, myocardial infarction, or separately, at one year5, two years6, and five years (Thyregod HG. Five-Year Outcomes From the All-Comers Nordic Aortic Valve Intervention Randomized Clinical Trial in Patients with Severe Aortic Valve Stenosis. Presented at the American College of Cardiology Annual Scientific Session, 10-12 March, 2018; Orlando, FL, USA). At five years, new permanent pacemaker implantation (PPI) following TAVI trended to be associated with increased mortality (p=0.07), and 2.5% of TAVI patients required valve reintervention whereas none did with SAVR (p=0.09). A subgroup analysis of patients with an STS score ≥4 showed a marginal benefit (p=0.05) in terms of mortality at five years after SAVR.
The preprocedural clinical risk profile of TAVI patients has been considerably decreasing over the years. The FRANCE-TAVI registry7 showed that, in 2015, 70% of the patients were at intermediate/low risk, among whom 30% were at low risk. The present post hoc analysis of SURTAVI shows favourable results in terms of the primary composite endpoint of all-cause death or disabling stroke at one year, from a large randomised cohort of patients at lower risk3. This study also highlights a considerable decrease of age among the three STS strata, with a mean age of 75 years in the STS score <3% stratum as compared to 80 years and 82 years in the 3-5% and ≥5% strata, respectively. This is in line with the latest transcatheter valve therapy registry data showing that >20% of patients were <75 years old8.
The continuous expansion of TAVI to lower-risk patients is already happening. In fact, many “healthy” octogenarians presenting with an STS score <3% are being treated with TAVI without much hesitation. However, for younger patients, structural valve deterioration (SVD), bioprosthetic valve failure (BVF) and the need for valve reintervention9-11 are important issues when making an informed decision between TAVI and SAVR. As mentioned above, SURTAVI patients with an STS score of <3% and those with scores between 3 and 5% had substantially higher rates of valve reintervention as early as one year. Although 84% of the patients received a CoreValve and 16% an Evolut™ R (Medtronic), and a newer generation of TAVI devices has evolved since then, the need for valve reintervention was relatively low in the STS score ≥5 stratum and showed similar rates to SAVR.
Anatomical features inherent to a patient’s age, notably the common prevalence of bicuspid aortic valves in younger adults12, pose technical challenges that are prone to suboptimal results (e.g., significant paravalvular leakage) with TAVI. Moreover, with conflicting data thus far, the long-term impact of new PPI requirements in younger patients is unknown. Therefore, the decision to offer TAVI rather than SAVR to low-risk and young patients must be carefully weighed against life expectancy9, also bearing in mind the excellent results achieved with SAVR13 and its well-known long-term durability14.
ONGOING TRIALS EVALUATING LOW-RISK PATIENTS
Randomised controlled trials are currently ongoing and have been designed to evaluate the safety and efficacy of TAVI versus SAVR in low-risk patients. The Medtronic Evolut TAVR trial (NCT02701283) includes patients with an STS score of <3%, and the Placement of Aortic Transcatheter Valves 3 (PARTNER 3) trial (NCT02675114) includes patients with an STS score <4%. The NOTION-2 trial (NCT02825134) includes patients with an STS score of <4% but who are also ≤75 years, hence this trial will provide important information regarding younger patients. The Randomized Trial of TAVI versus SAVR in Patients With Severe Aortic Valve Stenosis at Intermediate Risk of Mortality (DEDICATE), though not entirely low-risk, includes all-comers (STS score 2-6%), and set its primary efficacy endpoint as overall survival at five years. Unlike the two industry-sponsored trials, the NOTION-2 and DEDICATE trials allow any type of device with a CE mark. The results of these four trials will also help to determine the very long-term (i.e., 10 years) durability of contemporaneous TAVI devices.
In summary, it is reasonable to proceed with TAVI in low-risk octogenarians and it might be reasonable to start considering it in patients ≥75 years old, probably soon. However, in younger patients, it is possible that TAVI SVD will occur when the patient is still otherwise in good shape. TAVI-in-TAVI might be possible if the mechanism of BVF is stenosis, but it is unlikely to be solved if there is paravalvular leakage. Hence, beyond the safety of TAVI, its efficacy should also be seen in terms of long-term durability; thus, of major importance for younger patients at low risk. After the completion of low-risk trials, we might end up talking about TAVI in “all-comers”. Then, all the proposed risk score stratifications might perhaps remain for statistical adjustments (only?) rather than for decision making.
Conflict of interest statement
The author has no conflicts of interest to declare.