In this chapter of Tools and Techniques Clinical, percutaneous intervention of calcific coronary lesions is discussed using a stepwise approach. The following is a summarised overview of this technique. The complete, unabridged version with images is available online at www.eurointervention.org .
Background
With an increasingly ageing population and a higher prevalence of diabetes mellitus and kidney disease, fibrocalcific lesions are more likely to be encountered in everyday clinical practice.
Indications
Prior to proceeding to the percutaneous treatment of a calcified lesion it is important to ensure there is a clear indication for treating this, especially in view of the fact that in many cases the use of more specialised equipment, which can be associated with a higher risk of complications, is necessary. It is therefore important to follow current revascularisation guidelines.
Difficulties
Heavily calcified lesions can be resistant to simple balloon predilatation. This is evident angiographically by suboptimal balloon expansion or the presence of a “waist” during balloon inflation. This can lead to stent underexpansion, thus increasing the risk of stent thrombosis and in-stent restenosis.
Methods
Rotational atherectomy (RA) can play a pivotal role in achieving good lesion preparation, as demonstrated by the recently published ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. RA can be performed via either the femoral or radial route especially when burr size is compatible with a 6 Fr introducer sheath (up to 1.75 mm). Good guiding catheter support and the use of verapamil/nicardipine aiming to reduce coronary spasm during the procedure can be very helpful in ensuring a successful outcome and reducing the risk of complications. Crossing the lesion first with a conventional coronary wire followed by a wire exchange can reduce complications related to the less steerable rotablator wire. Following rotablation the procedure continues with a regular coronary wire (Figure 1). Laser atherectomy can also be of use in fibrocalcific lesions although we prefer to reserve this for calcified in-stent restenotic lesions. In patients with low left ventricular ejection fraction and one remaining vessel where distal embolisation can have detrimental effects, atherectomy should be avoided and alternative means of lesion preparation should be used. RA should also be used with caution in highly tortuous and angulated vessels where the risk of perforation is higher. In such cases predilatation at high pressure with non-compliant balloons and the use of specialised balloons can be particularly helpful. Specialised balloons include the ultra-high-pressure non-compliant OPN NC® balloon (SIS Medical AG, Winterthur, Switzerland), the AngioSculpt® scoring balloon catheter (AngioScore Inc., Fremont, CA, USA) and the Flextome™ Cutting Balloon™ device (Boston Scientific, Natick, MA, USA). The OPN balloon consists of a unique twin-layer balloon technology with ultra-low compliance. Rated burst pressure for this balloon is 35 atm with each balloon tested at 42 atm. The AngioSculpt balloon on the other hand is surrounded by a spiral nitinol element that works in combination with the balloon in order to “score” the target lesion upon balloon inflation (Figure 2). The cutting balloon can achieve a similar result as it incorporates three or four radially directed microsurgical blades on the surface of the balloon that help to “crack” the calcium upon balloon inflation. All the aforementioned devices are important tools for achieving adequate plaque modification, especially as we enter an era of increasing bioresorbable vascular scaffold use. The complete, unabridged online version discusses in depth the identification of the challenging calcium lesion, the access site, guiding catheters and guidewire selection, lesion preparation with devices and specialised balloons, and finally stent delivery and deployment.
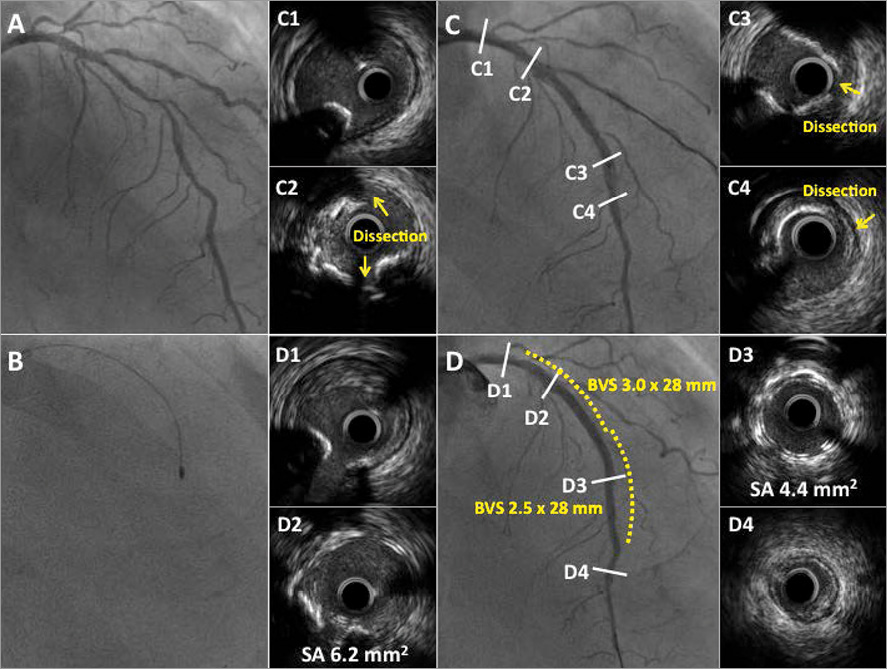
Figure 1. A case of rotational atherectomy in the left anterior descending artery followed by the implantation of a bioresorbable vascular scaffold (BVS). A) Initial angiographic image. B) Rotational atherectomy (RA) with 1.5 mm burr. C) Angiographic and intravascular images following RA with evident dissection thus demonstrating successful lesion modification. D) Angiographic and intravascular images following BVS implantation. SA: scaffold area
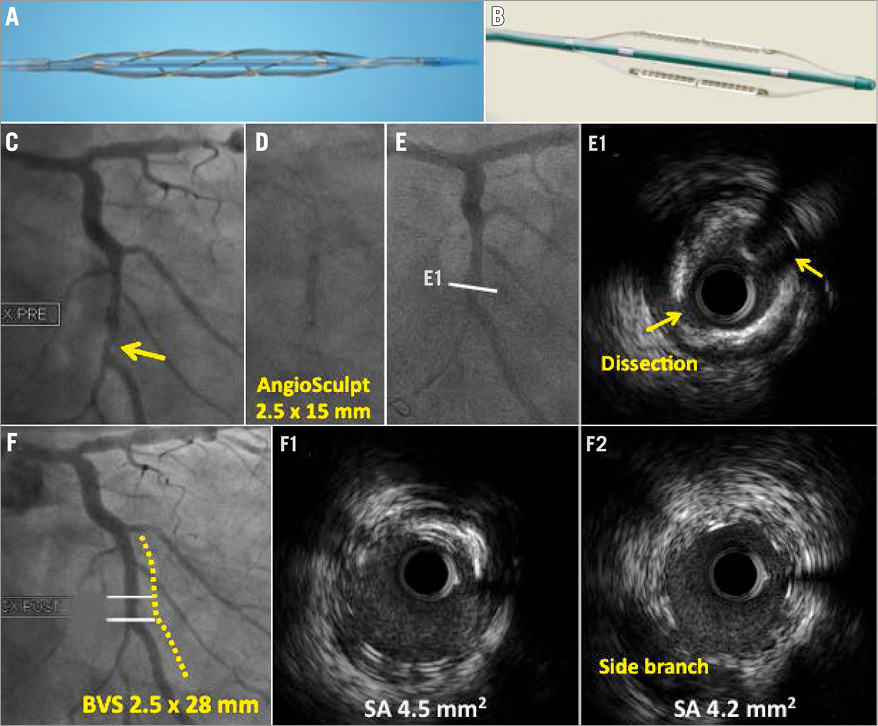
Figure 2. A case of bioresorbable vascular scaffold (BVS) implantation on a circumflex artery following lesion preparation with AngioSculpt. A) AngioSculpt balloon. B) Flextome Cutting Balloon. C) Initial angiographic image. D) AngioSculpt inflation demonstrating adequate balloon expansion. E) Angiographic and intravascular ultrasound images following AngioSculpt balloon inflation. F) Final angiographic and intravascular images following BVS implantation. SA: scaffold area
Conflict of interest statement
The authors have no conflicts of interest to declare.