Introduction
Before starting below the knee (BTK) interventions, one should consider the treatment of patients with critical limb ischaemia (CLI). The goal for this procedure is limb salvage. The prognosis of CLI is very poor. Six to 12 months after diagnosis, only 50% of patients with CLI will preserve both their limbs.
Background
CLI presentation is chronic ischaemic rest pain, ulcer or gangrene. CLI, the most important clinical indication for a BTK intervention, is caused by multilevel arterial disease in the majority of cases, and therefore BTK lesions are very often part of lower limb arterial involvement. Clinical goals in critical limb ischaemia treatment are ensuring wound healing to avoid amputation, decreasing ischaemic rest pain, increasing mobilisation of the patient and finally improving survival.
Treatments in CLI are performed with the objective of optimising blood flow to the foot by revascularisation of, at the very least, one vessel, though patients may benefit from two or even three patent vessels. Whenever possible, revascularisation of tibial arteries should be preferred to peroneal artery. In CLI commonly involves occlusions: more than 10 cm in around 50% of patients; in 30%, three-vessel occlusive lesions and in 50% at least one patent distal foot vessel.
The six angiosomes of the foot and ankle are supplied by three main arteries: the posterior tibial artery (PTA) supplies the plantar aspect of the toes, the web spaces between the toes, the sole of the foot and the inside of the heel. Three main branches of the PTA supply distinct portions of the sole: the calcaneal branch to the heel, the medial plantar artery to the instep, and the lateral plantar artery to the lateral midfoot as well as the forefoot. The anterior tibial artery (ATA) leads into the dorsalis pedis artery that supplies the dorsum of the foot. The peroneal artery (PA) supplies the lateral border of the ankle and the outside of the heel. Two branches of the PA supply the anterolateral part of the ankle and the hind foot: the anterior perforating branch to the anterolateral part of the upper ankle and the calcaneal branch to the plantar aspect of the heel.1
Indications
In patients presenting with severe limb ischaemia due to infrainguinal disease and who are suitable for surgery and angioplasty, abypass-surgery-first and a balloon-angioplasty-first strategy are associated with broadly similar outcomes in terms of amputation free survival. There is increasing evidence to support a recommendation for angioplasty in patients with CLI and infrapopliteal artery occlusion where inline flow to the foot can be re-established and where there is medical comorbidity.2 Therefore, limb salvage is the primary indication for endovascular treatment of infrapopliteal lesions, while angioplasty of these arteries is usually not indicated in patients with intermittent claudication.
The limb salvage rate is significantly higher than the angiographic patency rate after initially successful intervention below the knee. Therefore, long-term patency is not obligatory in CLI patients with persistent clinical improvement. Stent implantation in infrapopliteal vessels is generally reserved for cases with a suboptimal outcome after PTA.
BTK angioplasty step by step procedure
Pre-procedure investigations
Although physical examination alone is of relatively poor sensitivity, specificity and reproducibility, the feet must be inspected. The colour, temperature, and integrity of the skin, and the presence of ulcerations must be recorded as well. The primary noninvasive test for the diagnosis of low extremity artery disease (LEAD) is the ankle brachial index (ABI). In healthy persons, the ABI is 1.0. An ankle pressure less than 0.50 mmHg is usually recommended as a diagnostic criterion because it includes most patients for whom rest pain or ischaemic lesions do not improve spontaneously without intervention. An ABI raise of more than 0.15 is generally required to consider improving after revascularisation. Toe pressure at 30 mmHg replaces the ankle pressure criteria in case of medial calcinosis.
Duplex ultrasound (DUS) studies both the arterial anatomy and blood flow. DUS can also visualise run-off vessels, especially when using the colour mode. Combined with the ABI, DUS provides all the information necessary for management decisions in the majority of patients with LEAD, it confirms the diagnosis, and provides information on lesion location and severity.
Computed tomography angiography (CTA) allows imaging with high resolution and is quite comparable in visualising vessels. It can provide much of the diagnostic information of the lower-extremity arteries that can be obtained with conventional angiography. CTA has a sensitivity of 95% and specificity of 91% in the detection of below-knee arteries stenosis.
Magnetic resonance angiography (MRA) can noninvasively visualise the lower limb arteries, even in the most distal parts. Nevertheless, gadolinium contrast agents cannot be employed when severe renal failure (GFR less than 30 mL/min) is present. MRA cannot visualise arterial calcifications, which may be a limitation for the selection of the anastomotic site for a surgical bypass.
Considered as the gold standard for decades, digital subtraction angiography (DSA) is now reserved for patients undergoing interventions, especially concomitant to endovascular procedures. Indeed, the noninvasive techniques provide satisfying imaging in almost all cases, with less radiation, and avoid complications inherent to the arterial puncture, reported in 1% of cases.
Vascular access
Choosing the best access is primordial to ensure success. Measure the distance from the access site to the lesion intended for treatment before the sheath is inserted in order to select the appropriate length. Placing the sheath tip close to the lesion helps to minimise contrast required, and also supports any rapid exchange devices that might be used. Most below the knee interventions are performed using either an “up-and-over the aortic bifurcation” approach through the contralateral common femoral artery, or using an antegrade approach through the ipsilateral common femoral artery. Today, all the technical equipment available for infrapopliteal angioplasty make this procedure safe, feasible and durable.
Angioplasty
How to treat a BTK stenosis or occlusion? Treatment options remain controversial and are shown in Figure1.
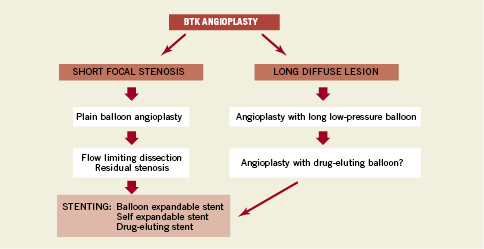
Figure 1. BTK angioplasty strategy.
Wire selection depends on the lesion subset. Most cases will be treated using 0.014” wire. In case of a short or long stenosis, dedicated wires for chronic total occlusion are not mandatory. Working with an introducer sheath, it is possible to use 0.018” wire. For long occlusions, one should use dedicated CTO wires and, at the same time, advance an over-the-wire balloon with the wire to increase support.
Short lesions
Therapeutic options in case of focal stenosis begin with plain old balloon angioplasty, and secondly –only in case of limiting flow dissection or residual stenosis– the possibility of implanting astent. The type of stent to be used is still a matter of debate, with some favouring balloon expandable stents, while others self-expandable stents. From Rand et al3, six months patency is 83.7% using stenting versus 61.1% plain balloon angioplasty. Overall limb salvage at six months is 98%.
Drug-eluting stents have been demonstrated to be effective in lowering the restenosis rate below the knee (BTK). Their design for coronary arteries makes them apractical option, more suited to shorter, tibial lesions. In short, for BTK lesions, primary stenting with DES could be recommended.
Figures2 and 3 showed an example of focal stenoses.
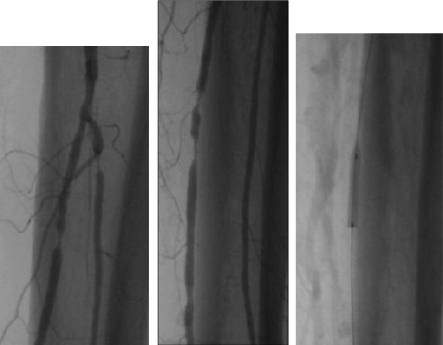
Figure 2. Short focal stenosis of the peroneal and posterior tibial artery: 0.014” wire. Coronary 2.5x20 mm balloon.
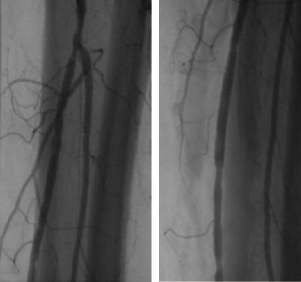
Figure 3. Stenting using a coronary stent for residual stenosis on the posterior tibial artery.
Long lesion
Dedicated long balloons (8-21 cm) to reduce procedure times and dissection are available. In a matched population treated with standard angioplasty, the restenosis rate at three months was 69%, showing a 61% relative reduction of restenosis. This was still associated with a remarkable clinical improvement (Rutherford class shift) and a 75% wound healing at 12 months.4,5
For long-segment BTK disease, drug eluting balloons (DEBs) have been designed to reduce the restenosis rate. A recent registry investigated a recently approved DEB for its application to infrapopliteal arteries.6 The one year clinical results are promising, and seem to confer a durable benefit. However, more studies are required to confirm whether DEB are superior to the standard treatment of plain old balloon angioplasty in patients with CLI from BTK disease.
Self-expandable stents have some advantages when compared to coronary stents due to their longer length and greater conformability. Bosiers et al studied the use of the Xpert stent (Abbott Vascular, Santa Clara, CA, USA) for a mean lesion length of 43.2mm. Primary patency is 76.3% at one year and 54.4% at two years. The limb salvage rate is 95.8% at one year and 90.8% at two years.7
Complications
During retrograde tibial recanalisation, it is possible to infuse nitroglycerine or prostanoids by antegrade access to avoid spasm at the puncture site. After sheath removal, use gentle balloon angioplasty by antegrade access.
In the case of infra-popliteal arterial perforation, the first step is repeat balloon inflation (5 minutes low pressure 6 atmospheres). At the same time administer protamine iv to antagonise heparin. After the balloon angioplasty, if the perforation is still present, it is possible to implant a covered stent (Graftmaster from Abbott). Coil embolisation should only be performed if the perforation is unresolved.
In the case of infrapopliteal arterial abrupt occlusion, there are different options. To manage embolic distal occlusion intra-arterial infusion of 100000 UI urokinase is safe and feasible. A combined strategy with thrombo-aspiration using 5 Fr MP guiding catheter or coronary aspiration devices (Pronto; Vascular Solutions Inc, Minneapolis, MN, USA or Export AP aspiration catheter; Medtronic, Minneapolis, MN, USA) are efficient.
To avoid complications an adequate pre-treatment is required.
Conclusion
BTK angioplasty is dedicated for CLI patients. One has to deal with multivessel disease, a high proportion of diabetics and patients of advanced age with the involvement of the deep femoral artery (DFA) as well as infrapopliteal artery involvement with media-calcinosis.
The treatment of CLI in diabetic patients requires an interdisciplinary approach. In our experience, the keys for a successful BTK endovascular procedure are the choice of the vascular approach, the selection of materials and the knowledge of all available techniques. The clinical outcome depends mainly on a proper infection management, and the success of the procedure of revascularisation. Combination of the latest interventional technologies and the use of alternative interventional approaches, such as the transpedal, result in a very acceptable acute success-rate.
DES and DEB have the potential to further improve the results of interventional recanalisation.