Abstract
Aims: Several studies have evaluated the impact of a CTO on short- and long-term mortality in STEMI patients. It has been speculated that the adverse effect on prognosis could differ per coronary location. The purpose of this study was to evaluate whether the long-term prognosis of STEMI patients differs according to the coronary location of the CTO.
Methods and results: Between 2000 and 2012, a total of 480 STEMI patients with a CTO in a non-infarct-related artery were included. The primary outcome for the present analysis was three-year all-cause mortality, evaluating the impact of the coronary CTO and infarct location. Four hundred and thirteen patients had a single CTO in a non-infarct-related artery, whereas 67 patients had more than one CTO and in this group mortality was higher. In patients with a single CTO, the highest risk of mortality was observed when the culprit lesion was located in the LAD or proximal LCX or when the CTO lesion was located in the proximal LAD.
Conclusions: We previously reported that STEMI patients with a CTO have a worse prognosis than STEMI patients without a CTO. We now show that, in these patients, LAD or proximal LCX location for the culprit lesion, or proximal LAD location for the CTO lesion, is associated with the highest risk. As a result, almost all CTO patients are at increased risk for mortality due to the combination of the culprit and CTO artery location.
Introduction
Increased angiographic severity and the extent of coronary artery disease are associated with higher mortality1-4. Coronary chronic total occlusions (CTO) are often considered the most complex expression of coronary artery disease (CAD). In patients with significant coronary artery disease a CTO is present in approximately 16%5,6. Previously, several studies in patients with stable coronary artery disease have reported that successful versus failed elective CTO revascularisation has been associated with symptom relief7, reduced need for coronary artery bypass surgery8, improvement of electrical stability9,10 and left ventricular function and even reduced mortality. A recent meta-analysis reported an increment of 4.44% in left ventricular ejection fraction and reduced long-term mortality after successful versus failed CTO revascularisation (OR: 0.52)11. However, it has been postulated that these beneficial effects might vary according to the anatomical location of the CTO, showing only an improved survival after treatment of the left anterior descending coronary artery (LAD) and left circumflex (LCX) but not the right coronary artery (RCA)12,13.
Several studies have shown a strong association between the presence of a concurrent CTO in ST-elevation myocardial infarction (STEMI) patients and short- and long-term mortality14-17. The purpose of this study was to evaluate whether the long-term prognosis of STEMI patients differs according to the coronary location of the CTO.
Methods
STUDY COHORT
From January 2000 to December 2012, STEMI patients with a CTO in a non-infarct-related artery (IRA) treated with primary percutaneous coronary intervention (PCI) in our hospital, for whom the diagnostic angiography was available, were entered into a dedicated database after informed consent was obtained and approval by our institutional review committee granted. Acute STEMI was diagnosed when patients had symptoms of an acute myocardial infarction lasting 30 minutes to 12 hours, accompanied by an electrocardiogram with ST-segment elevation >1 mm (0.1 mV) in ≥2 contiguous leads. Patients were immediately transported to the cardiac catheterisation laboratory and underwent coronary angiography with a view to performing primary PCI. PCI was performed using standard techniques, provided the coronary anatomy was suitable.
Prior to PCI, all patients were treated with heparin (5,000 IU) and aspirin (500 mg). Adjunctive treatment with glycoprotein IIb/IIIa inhibitors was at the discretion of the operator. Post-PCI antiplatelet therapy was prescribed according to the guidelines: clopidogrel, prasugrel or ticagrelor. Duplicate patients due to recurrent STEMI or patients lost to follow-up were excluded. Patients with previous CABG surgery were excluded due to the complexity of interarterial connections and patency of the graft and native vessel.
DATA COLLECTION
Baseline characteristics were collected prospectively in the aforementioned dedicated database. Information on vital status was obtained from the Dutch national population register (Statistics Netherlands, Voorburg, The Netherlands). Patient data were checked for inconsistency and completeness.
ANGIOGRAPHIC ANALYSIS
All coronary angiograms were reviewed by an experienced CTO operator (J. Henriques) and an interventional research fellow (L. Hoebers).
DEFINITIONS
A CTO was defined as a 100% luminal narrowing in a non-IRA before PCI without antegrade flow or with antegrade or retrograde filling through collateral vessels. Proximal lesions were considered segment 6 or 7 for the LAD coronary artery and segment 11 for the LCX coronary artery.
PRIMARY OUTCOME
The primary outcome for the present analysis was three-year all-cause mortality in STEMI patients with a CTO, evaluating the impact of the coronary CTO location corrected for the location of the culprit artery, with the exclusion of left main lesions and multiple CTO patients due to their low prevalence.
STATISTICAL ANALYSIS
Discrete variables were summarised as frequencies and percentages. Differences in baseline characteristics between the groups were tested for significance by the χ2 test. Statistical significance was defined as a p-value <0.05. Cumulative event rates of all-cause death were estimated using the Kaplan-Meier method and compared using the log-rank statistic. Follow-up for mortality was censored at the date of last follow-up by checking vital status in the Dutch population register, or at three years, whichever came first. Hazard ratios for all-cause mortality were calculated using Cox proportional hazards regression analyses after verification of the proportional hazards assumption. The multivariable model was built by adding covariates from the baseline characteristics table with a p-value <0.10 in univariate analysis. All variables with a p-value >0.10 were removed from the model.
Results
Between 2000 and 2012, 6,771 unique STEMI patients underwent primary PCI in our hospital, of whom 744 (11%) had a CTO (Figure 1). In 172 (23%) CTO patients the coronary angiogram was irretrievable and in seven (1%) patients the quality of the angiogram was insufficient for analysis. Of the remaining patients, 72 (10%) were excluded due to previous CABG and 13 (2%) patients did not receive primary PCI, resulting in a CTO cohort of 480 patients.
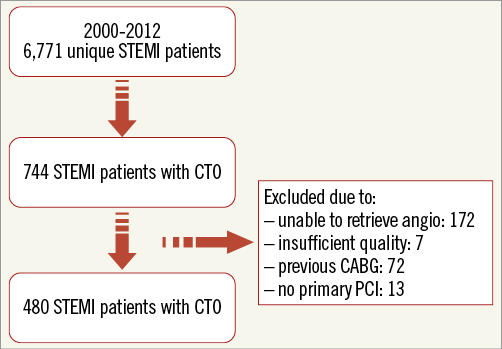
Figure 1. Flow chart. CABG: coronary artery bypass graft surgery; CTO: chronic total occlusion; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction
PATIENT CHARACTERISTICS
Of these 480 patients, 413 had a single CTO in a non-IRA whereas 67 patients had more than one CTO (Table 1). The majority of the CTO patients were male (76%) with a mean age of 64 years (55-74). Approximately one quarter of the patients had a previous MI and a similar proportion of patients were in cardiogenic shock on presentation. The culprit lesion was in the LAD in 44% of patients, in the RCA in 32% of patients, in the LCX in 23% of patients, and in the left main in 1%. The last group was excluded from the primary analysis due to its low prevalence. The culprit lesion was most often treated with stent placement (90%), with a post-procedural Thrombolysis In Myocardial Infarction flow grade 3 in 85%. Among patients with a single CTO in a non-IRA, the CTO was most often located in the RCA (47%) and less often in the LCX (30%) and LAD (23%). There were no significant differences regarding the baseline characteristics among these groups.
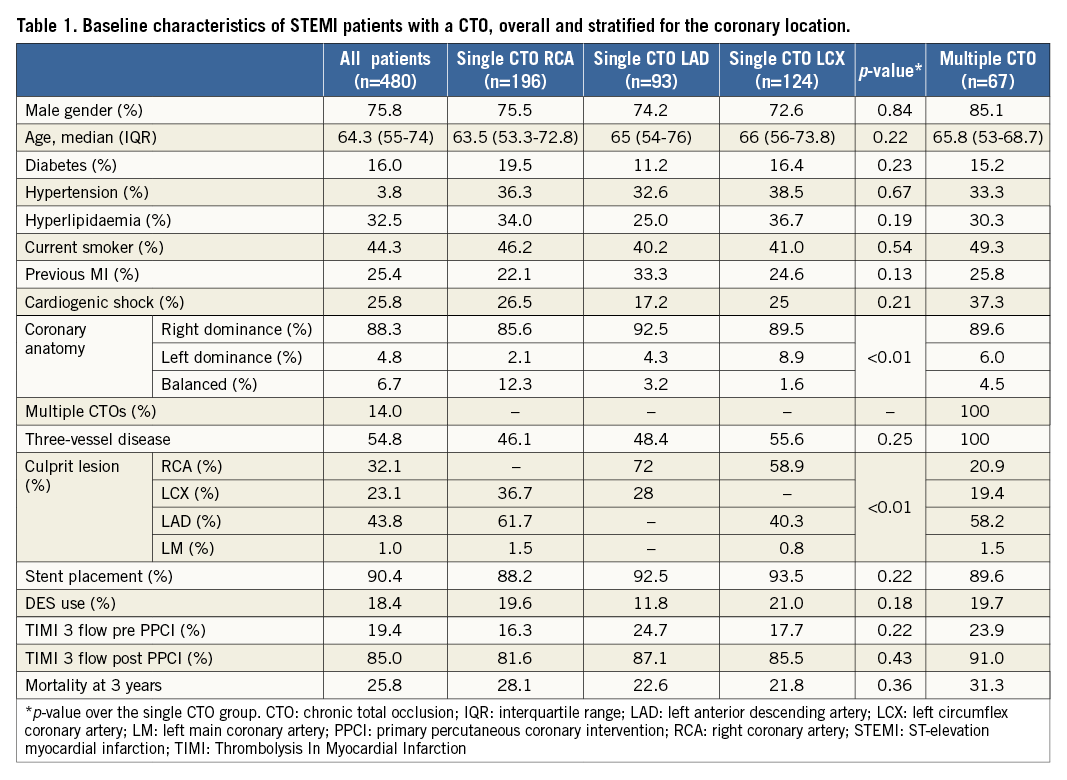
Figure 2 shows the three-year mortality of the STEMI cohort stratified according to single versus multiple CTO. Long-term mortality was higher in the latter group. Since these patients have an increased risk compared to single CTO patients, they were excluded from the primary analysis.
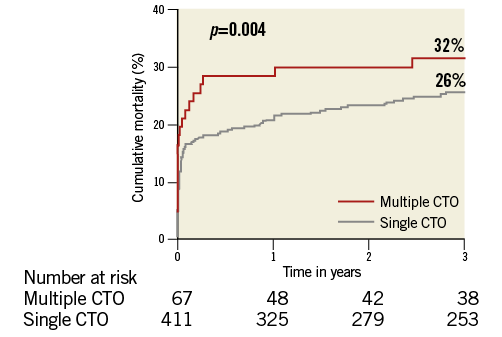
Figure 2. Mortality in STEMI patients with a single versus multiple CTO. CTO: chronic total occlusion; STEMI: ST-segment elevation myocardial infarction
PROGNOSTIC IMPACT ACCORDING TO CORONARY LOCATION
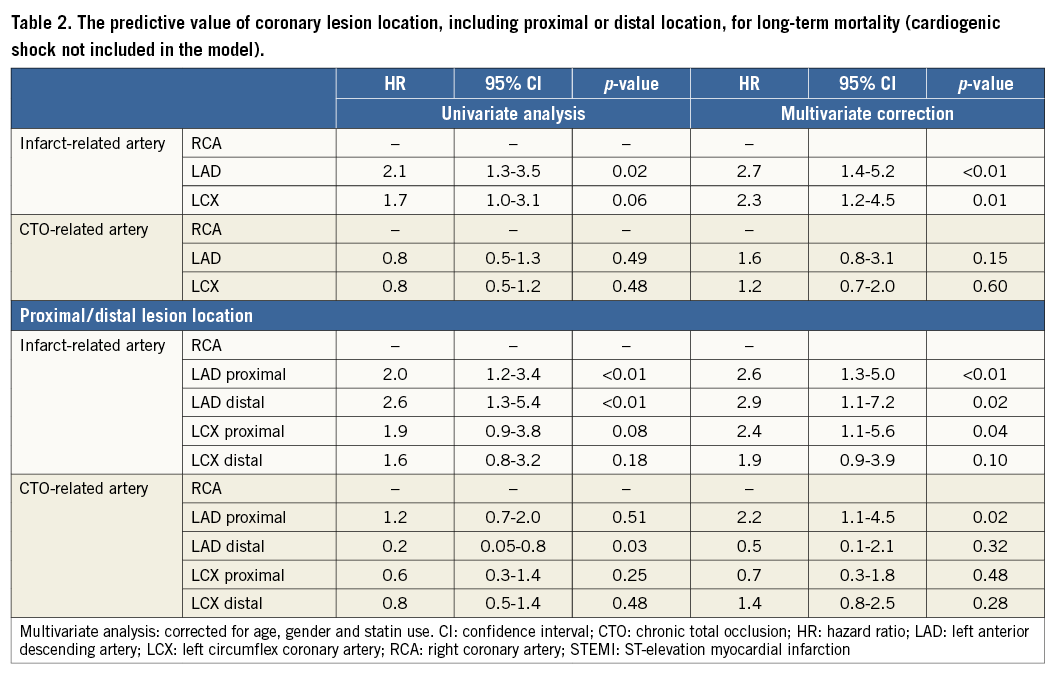
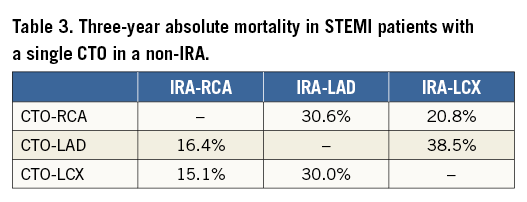
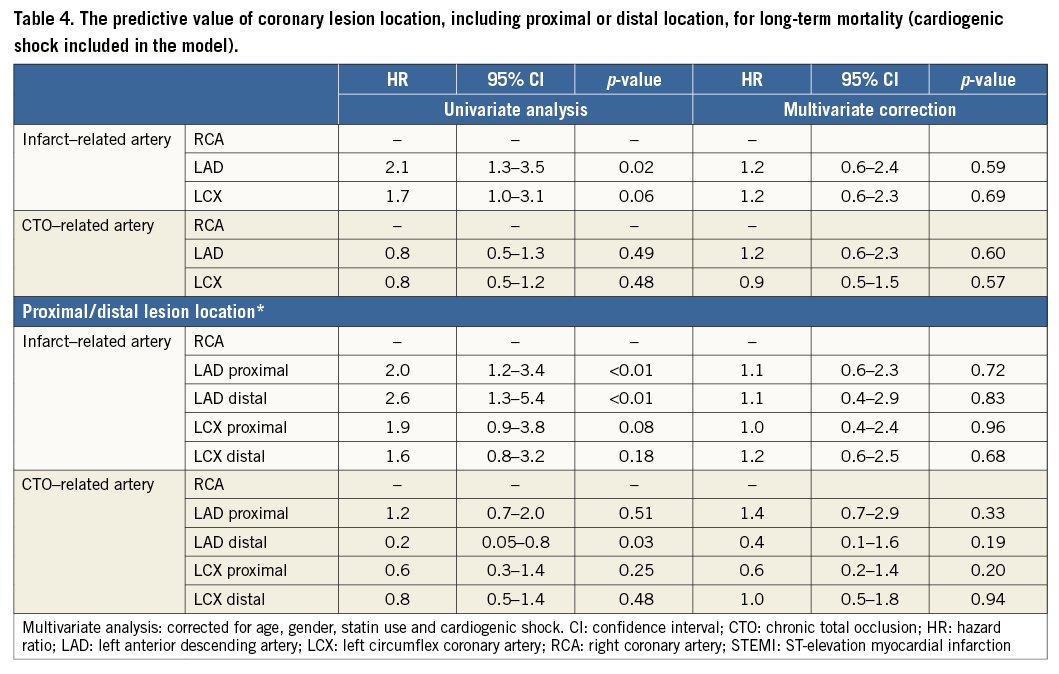
Figure 3 shows long-term mortality according to the location of the culprit artery and Figure 4 shows mortality after stratification of the cohort according to the CTO artery. In this cohort the mortality of STEMI patients with a CTO and the culprit artery in the LAD (31%) or LCX (26%) was comparable, while mortality in the RCA group was lower (16%). When the cohort was stratified according to the location of the CTO (Figure 4), the highest mortality was observed in STEMI patients with a CTO located in the RCA (28%), and the lowest mortality in patients with a CTO in the LAD (23%) or LCX (21%). When corrected for the location of the culprit artery and other significant variables, a CTO located in the LAD was associated with a non-significant increased risk for mortality compared to a CTO located in the RCA or LCX (HR: 1.6, 95% CI: 0.8-3.1, p=0.15, HR 1.2, 95% CI: 0.7-2.0, p=0.60) (Table 2). When the left coronary system was stratified into a proximal and distal part, a CTO located in the proximal LAD was associated with significantly increased mortality compared with a CTO located in the RCA (HR: 2.2, 95% CI: 1.1-4.5, p=0.02) (Table 2). For the culprit lesion, a location in the LAD or proximal LCX was associated with a worse survival compared to the RCA (Table 2). As a result, when the CTO is located in the RCA, the culprit artery must be situated in the LAD or LCX and thus, through the combination of CTO and the location, the majority of the cohort was at a high risk for mortality (Table 3). Patients with the culprit artery in the RCA and a concurrent CTO in the LAD or LCX had the lowest absolute three-year mortality rate. In all other combinations, the mortality rate was at least twice as high, with the highest mortality rate in patients with a culprit artery located in the LCX and the CTO artery located in the LAD. When cardiogenic shock was included in the model, only age remained a significant predictor for mortality (Table 4).
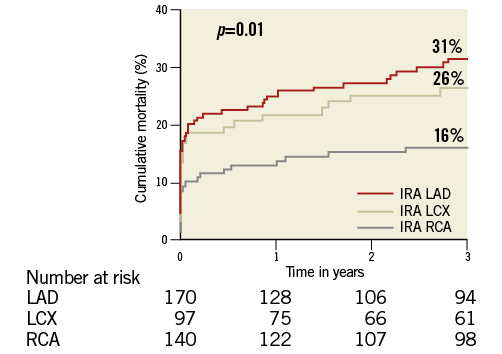
Figure 3. Mortality in STEMI patients with a single CTO stratified according to culprit-related artery. CTO: chronic total occlusion; LAD: left anterior descending artery; LCX: left circumflex artery; RCA: right coronary artery; STEMI: ST-segment elevation myocardial infarction
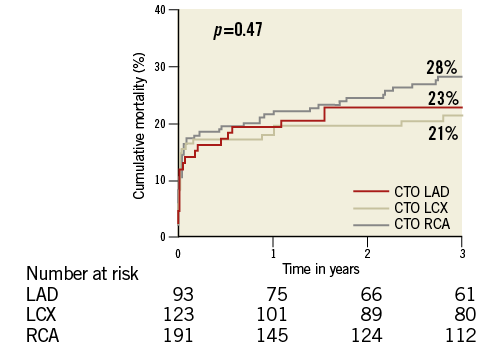
Figure 4. Mortality in STEMI patients with a single CTO stratified according to CTO-related artery. CTO: chronic total occlusion; LAD: left anterior descending artery; LCX: left circumflex artery; RCA: right coronary artery; STEMI: ST-segment elevation myocardial infarction
Discussion
Previous literature has shown increased mortality in STEMI patients with versus without a CTO in a non-IRA. In this paper, we showed that in these patients the highest mortality was observed when a CTO was located in the proximal LAD or the culprit artery in the LAD or proximal LCX. Until now, there have been no reports in the literature in which mortality has been evaluated in STEMI patients with a CTO in a non-IRA according to the coronary location of the CTO and the culprit artery, although the importance of the LAD seems intuitive, as reduced mortality might be explained by the prognostic significance of left ventricular function. As left ventricular function is related to cardiogenic shock, it could explain our finding that all prognostic significance of CTO or culprit location was lost after adding cardiogenic shock into the multivariate model. The importance of the anterior wall of the left ventricle on prognosis, which is for the most part dependent on the LAD for blood supply, has been well documented both in stable coronary artery disease and in patients with myocardial infarction18-20. Compared with a myocardial infarction not related to the LAD, or distal versus proximal LAD-related myocardial infarction, those patients have a worse clinical outcome in terms of mortality, haemodynamic instability, and need for left ventricular assist devices, which is probably due to lower residual left ventricular ejection fraction (LVEF), caused by a larger final infarct size19,21-26. In addition, the observed lower myocardial blush grade (MBG) in proximal LAD culprit lesions could be related to a larger infarct size, more oedema, higher filling pressures, and increased downstream microvascular resistance27. Comparable findings have been observed in STEMI patients with a CTO in whom mortality, residual left ventricular function, haemodynamic stability, ST-segment resolution and MBG were worse compared to non-CTO STEMI patients15-17,27,28; however, these endpoints have never been specified according to coronary location.
Another explanatory mechanism could be an alteration in the balance of the autonomic nervous system owing to the location of coronary occlusion, which has been associated with life-threatening ventricular arrhythmias and cardiac death in survivors of myocardial infarction29. Sympathetic innervation is less pronounced in the inferior compared with the anterior myocardial wall, whereas vagal afferent receptors have a preferential distribution on the posterior wall of the left ventricle30,31. In animal experiments, vagal stimulation or sympathetic inhibition reduces the threshold for ventricular fibrillation32. Therefore, patients with an acute inferior occlusion after myocardial infarction might be relatively protected from ventricular fibrillation in contrast to patients with an acute anterior occlusion who might have a higher frequency of ventricular arrhythmia. In a small cohort (n=23), CTO PCI has proven to have a beneficial effect on the autonomic nervous system in the LAD artery, which was not observed after CTO PCI of the RCA33. These findings suggest a potential antiarrhythmic effect after LAD revascularisation, resulting from a shift in the autonomic balance in favour of the parasympathetic nervous system.
Our cohort presents a group with high mortality rates of between 15.1% and 38.5%, depending on the combination of coronary location. In a large cohort of STEMI patients treated with primary PCI, the five-year mortality rates for single-vessel disease (SVD), multivessel disease (MVD) without CTO and MVD with CTO were 14%, 20% and 38%, respectively15. Our data emphasise the need for further assessment of the optimal treatment strategy in these challenging patients.
At present, no randomised data exist as to whether revascularisation of a CTO in STEMI or stable angina patients can actually reverse the observed worse outcome. Currently, three randomised trials are enrolling patients, one in STEMI patients, the EXPLORE trial34, which will evaluate whether CTO PCI in a non-IRA within seven days of primary PCI can improve LVEF and reduce left ventricular end-diastolic volume at four-month follow-up, compared with optimal medical therapy in 300 STEMI patients. The other two randomised clinical trials are currently enrolling patients with CTO and stable coronary artery disease, namely the EuroCTO trial35, which will randomly assign 1,200 patients to receive either PCI with DES and optimal medical therapy or optimal medical therapy alone. The primary endpoint is quality of life at one year and major cardiovascular events at three years. Similarly, the DECISION-CTO trial36 will randomly assign 1,284 patients to receive PCI with DES and optimal medical therapy or optimal medical therapy alone. The primary endpoint is a composite of all-cause mortality, myocardial infarction, stroke, and any revascularisation at three-year follow-up. Although randomised data are lacking, observational studies have shown several beneficial effects after CTO revascularisation in patients with stable angina, such as improvement in angina and quality of life7, a potential improvement in electrical myocardial stability9,10, a reduced need for CABG surgery8, enhanced tolerance of future coronary events, increased left ventricular function, and a substantial increase in survival11. Two observational studies evaluated the difference in survival after CTO revascularisation in patients with stable CAD according to the target vessel and found only a survival benefit after successful CTO PCI in either the LAD or the LCX artery, but not in the RCA12,13. As mentioned above, survival data in STEMI patients after CTO revascularisation are absent.
Limitations
Several limitations are applicable to this study. Importantly, our study was limited by its observational nature and its modest cohort size. Due to the unbalanced known IRA distribution in a general STEMI population, with the LCX being the least frequent IRA and the RCA being the most frequent CTO artery, there is an overall unbalanced distribution of combinations of (CTO/IRA) arteries. Although this is in accordance with daily clinical practice, it may be a limitation upon interpreting the presented results6. Furthermore, although multivariate Cox proportional hazards models were constructed, unknown or unmeasured confounders may still have introduced bias. No complete data were available on possible mechanisms explaining the observed difference in mortality by target vessel, such as infarct size and left ventricular function. More research is needed to elucidate these mechanisms. Last, the coronary angiograms were not analysed by an independent core lab.
Conclusions
In conclusion, we previously reported that STEMI patients with a CTO have a worse prognosis than STEMI patients without a CTO. We now show that in these patients LAD or proximal LCX location for the culprit lesion or proximal LAD location for the CTO lesion is associated with the highest risk. As a result, almost all CTO patients are at increased risk for mortality due to the combination of the culprit and CTO artery location.
| Impact on daily practice This report shows that the highest risk of mortality was observed when the culprit lesion was located in the LAD or proximal LCX or when the CTO lesion was located in the proximal LAD. In clinical practice, these patients constitute a very high risk group. Whether CTO intervention in addition to primary PCI could improve prognosis will be answered shortly in the EXPLORE trial. The patients who would theoretically benefit the most regarding mortality are those in whom the culprit lesion is located in the LAD or proximal LCX or those in whom the CTO lesion is located in the proximal LAD. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
References