Abstract
Aims: The aim of the current study was to investigate the impact of a chronic total occlusion (CTO) in a non-infarct-related coronary artery (non-IRA) on one-year mortality and occurrence of cardiac arrhythmia in patients with cardiogenic shock (CS) complicating acute myocardial infarction (AMI).
Methods and results: In a retrospective sub-analysis of the Intraaortic Balloon Pump in Cardiogenic Shock II trial (IABP-SHOCK II) and its accompanying registry, 201 (26%) of 761 patients had a CTO in a non-IR major coronary artery. Mortality was significantly higher in the CTO group at day of admission (19% vs. 11%; p=0.005), 30 days (53% vs. 41%, p=0.002), and 12 months (63% vs. 51%, p=0.002). In the adjusted multivariate Cox regression analysis, a CTO in a non-IRA was an independent predictor of mortality at 12 months (hazard ratio 1.30, 95% confidence interval [CI]: 1.02-1.67, p=0.03). At 30-day follow-up, ventricular arrhythmias requiring defibrillation occurred more frequently in patients with non-IRA CTO in the univariate analysis (33% vs. 21%, odds ratio 1.83, 95% CI: 1.28-2.62, p=0.002).
Conclusions: In patients with CS complicating AMI, the presence of CTO in a non-IRA is associated with a higher incidence of ventricular arrhythmias and is an independent predictor of mortality at 12-month follow-up.
Abbreviations
AMI: acute myocardial infarction
CI: confidence interval
CS: cardiogenic shock
CTO: chronic total occlusion
IABP-SHOCK II: Intraaortic Balloon Pump in Cardiogenic Shock II
Non-IRA: non-infarct-related coronary artery
OR: odds ratio
PCI: percutaneous coronary intervention
STEMI: ST-segment elevation myocardial infarction
TIMI: Thrombolysis In Myocardial Infarction
Introduction
The presence of a chronic total occlusion (CTO) in a non-infarct-related coronary artery (non-IRA) is an independent predictor of mortality in haemodynamically stable ST-elevation myocardial infarction (STEMI) patients1-3. Theoretically, the extent of myocardial dysfunction and ischaemic damage could be increased in the presence of non-IRA CTO due to a reduced collateral circulation to the acutely occluded infarct-related artery. Moreover, pre-existing collaterals perfusing the myocardium supplied by the non-IRA CTO are compromised in the setting of acute myocardial infarction (AMI) which again increases myocardial damage by increasing the area at risk. In addition, the presence of a non-IRA CTO appears to be associated with worse left ventricular function, potentially leading to a higher susceptibility to life-threatening arrhythmias, which again triggers haemodynamic instability4. Data on the association of CTO in non-IRA in patients with infarct-related cardiogenic shock (CS) are scarce and led to inconclusive results2,5,6. The aim of the current study was therefore to analyse the impact of a CTO in a non-IRA on clinical outcome based on data derived from the largest prospective randomised trial in patients with CS complicating AMI, the Intraaortic Balloon Pump in Cardiogenic Shock II (IABP-SHOCK II) trial, and its corresponding registry.
Methods
STUDY POPULATION AND PROTOCOL
The design of the IABP-SHOCK II trial and its accompanying registry as well as short- and long-term results have been published previously7-9. The trial was a multicentre, open-label, randomised study investigating the role of IABP in patients with CS and AMI (with or without ST-segment elevation). CS was defined as a systolic blood pressure of less than 90 mmHg for more than 30 minutes or need of infusion of catecholamines to maintain a systolic pressure above 90 mmHg, presence of clinical signs of pulmonary congestion and impaired end-organ perfusion. Exclusion criteria were resuscitation for more than 30 minutes; no intrinsic heart action; onset of shock more than 12 hours before screening; mechanical cause of CS; shock as a result of a condition other than AMI; massive pulmonary embolism; severe peripheral arterial disease precluding insertion of an IABP; aortic regurgitation >II° in severity; comatose patients with fixed dilatation of pupils not induced by drugs; patients older than 90 years of age and severe concomitant disease associated with a life expectancy of less than six months. Patients in CS not eligible for randomisation were enrolled in the prospective IABP-SHOCK II registry7. All patients were expected to undergo early revascularisation (primary PCI or bypass grafting) and to receive the best available medical treatment according to guidelines10. Haemodynamic stability was defined as systolic blood pressure above 90 mmHg for at least 60 minutes without catecholamine support and in the absence of signs of end-organ hypoperfusion7. The trial is registered with ClinicalTrials.gov, NCT00491036. All patients or their legally authorised representatives provided written informed consent and the ethics committee at each participating centre approved the trial design.
In this retrospective sub-analysis, a CTO in a non-IRA was defined as the presence of an occluded major coronary artery for at least three months with Thrombolysis In Myocardial Infarction (TIMI) flow grade 0. Duration of vessel occlusion was estimated based on a history of sudden chest pain, a previous MI in the same target vessel territory, or a previous coronary angiography. In a pooled cohort of both the randomised trial and the registry, patients were divided according to the presence or absence of a CTO in a non-IRA. A CTO of a side branch <2 mm in diameter or a CTO of a major coronary artery with a functional bypass graft to the distal vessel territory was not included in the CTO group. Endpoints were occurrence of ventricular arrhythmias at 30 days and one-year mortality between the two groups.
STATISTICAL ANALYSIS
Differences between the two groups were assessed with use of Fisher’s exact or the chi-square test for binary variables and the Student’s t-test or Mann-Whitney U rank-sum test for quantitative variables as appropriate. Quantitative variables are presented as medians with interquartile ranges.
Odds ratios (OR) and 95% confidence intervals (CI) were calculated for mortality throughout the first 12 months. Cumulative mortality was characterised with the use of Kaplan-Meier plots with log-rank testing used for the comparison between the two groups. The influence of baseline demographic and angiographic variables on one-year mortality was evaluated with Cox proportional hazards regression, and the results expressed as hazard ratio with 95% CI.
The multivariable Cox regression analysis model for one-year mortality was built by stepwise selection. All baseline patient variables related to one-year mortality in univariable analysis defined by p<0.1 were entered into the model. Data were maintained at the Institut für Herzinfarktforschung, Ludwigshafen, Germany, where all the statistical analyses were performed by independent personnel using SAS statistical package, Version 9.3 (SAS Institute Inc., Cary, NC, USA). Differences with a p-value <0.05 were considered statistically significant.
Results
BASELINE CHARACTERISTICS
The total cohort of the IABP-SHOCK II trial and registry included 783 patients (n=600 randomised trial, n=183 registry). In 761 (97%) patients, information about the degree of stenosis in non-IRAs was available. Of these, 201 (26%) had a CTO in a non-IRA and 560 (74%) did not (Figure 1).
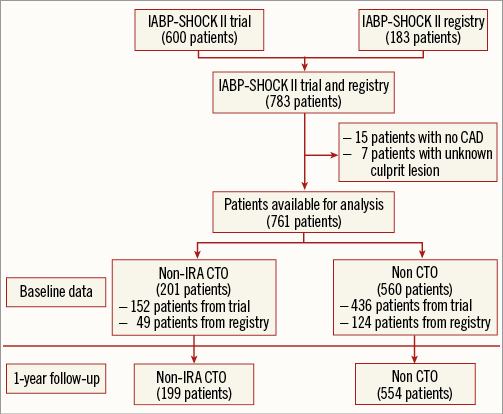
Figure 1. Study flow chart. CAD: coronary artery disease; CTO: chronic total occlusion; IABP-SHOCK II: Intraaortic Balloon Pump in Cardiogenic Shock II; Non-IRA: non-infarct-related artery
Baseline characteristics differed significantly between the two groups (Table 1).
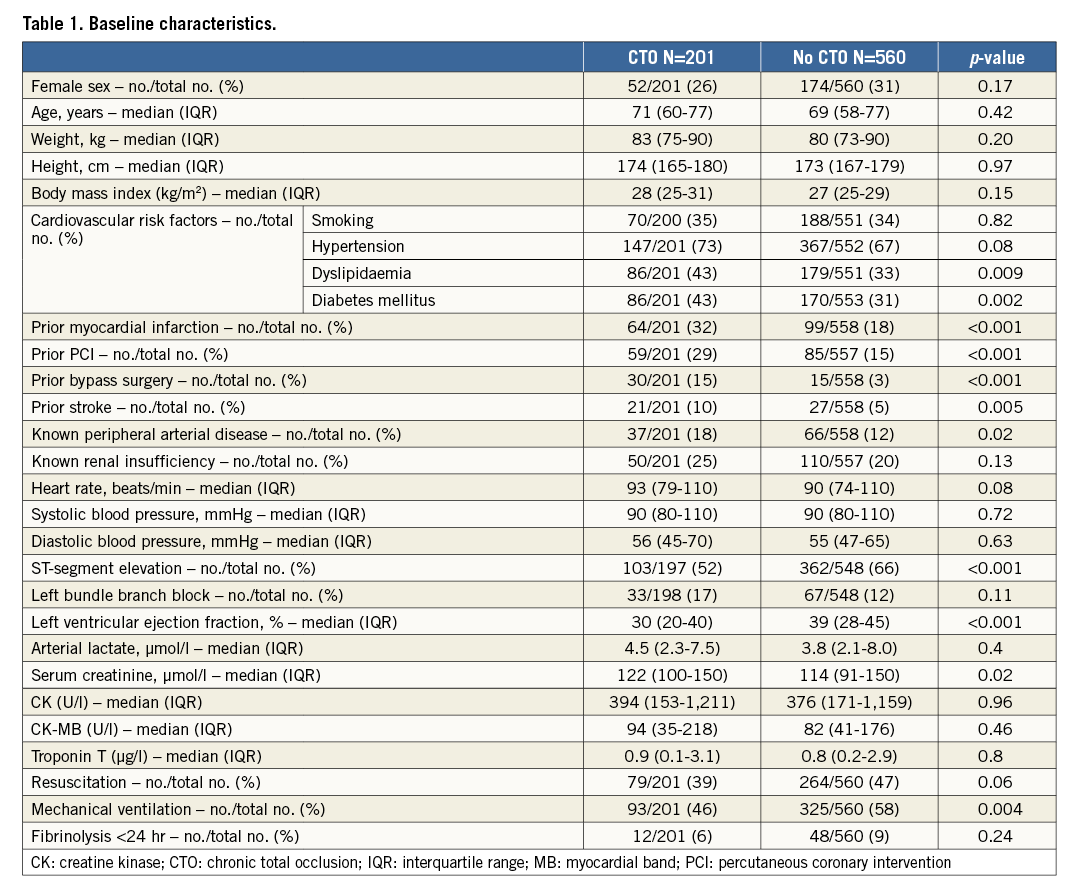
Patients with CTO had more hyperlipidaemia, diabetes mellitus, increased serum creatinine and more severe comorbidities including prior AMI, prior coronary revascularisation, stroke as well as peripheral vascular disease. Left ventricular ejection fraction was significantly lower in CTO patients.
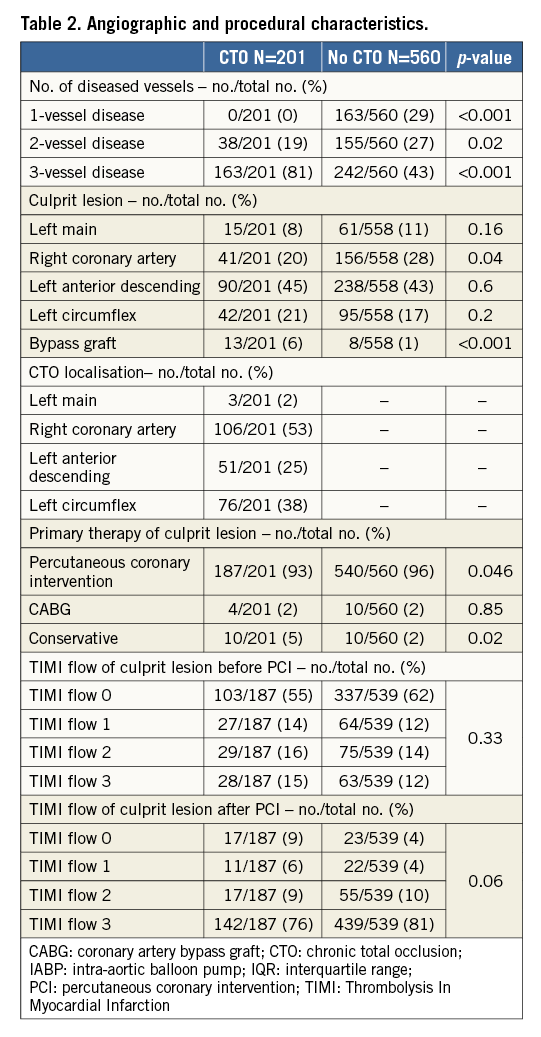
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic features and procedural details of the patients are shown in Table 2. Reperfusion success was reduced in patients with non-IRA CTO with a higher rate of TIMI flow 0 in the culprit lesion after PCI.
Clinical outcome
In unadjusted analysis, mortality was significantly higher in the group with a CTO in a non-IRA at the day of admission (19% vs. 11%, OR 1.89, 95% CI: 1.21-2.96, p=0.005), 30 days (53% vs. 41%, OR 1.65, 95% CI: 1.19-2.29, p=0.002), six months (61% vs. 48%, OR 1.7, 95% CI: 1.23-2.37, p=0.001), and 12 months (63% vs. 51%, OR 1.68, 95% CI: 1.20-2.34, p=0.002) (Figure 2). There was no interaction between allocation to the IABP treatment arm and the presence of a non-IRA CTO in terms of mortality.
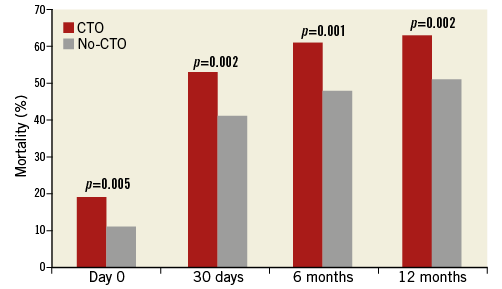
Figure 2. Mortality over the first 12 months in patients with and without a chronic total occlusion (CTO) in a non-infarct-related artery.
In multivariable stepwise Cox regression analysis adjusting for significant variables in univariable testing, a CTO in a non-IRA was an independent predictor of mortality at 12 months (hazard ratio 1.30, 95% CI: 1.02-1.67, p=0.03) (Table 3, Figure 3).
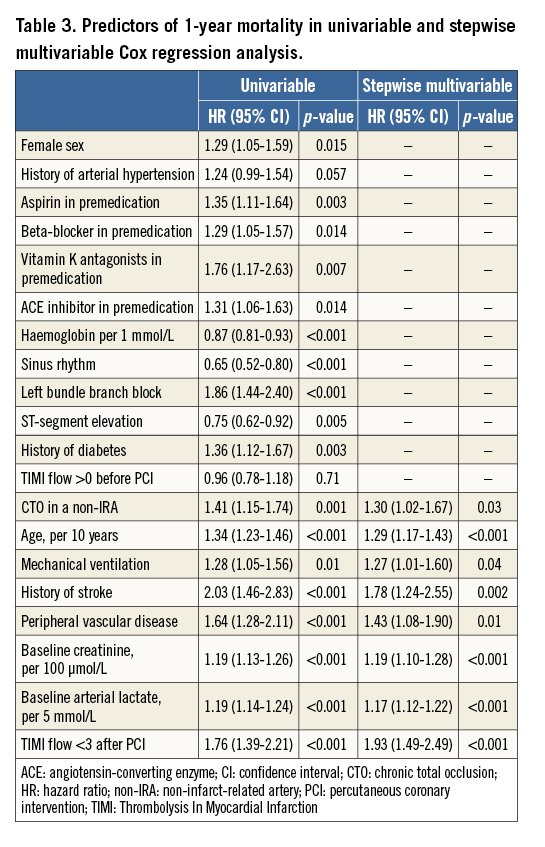
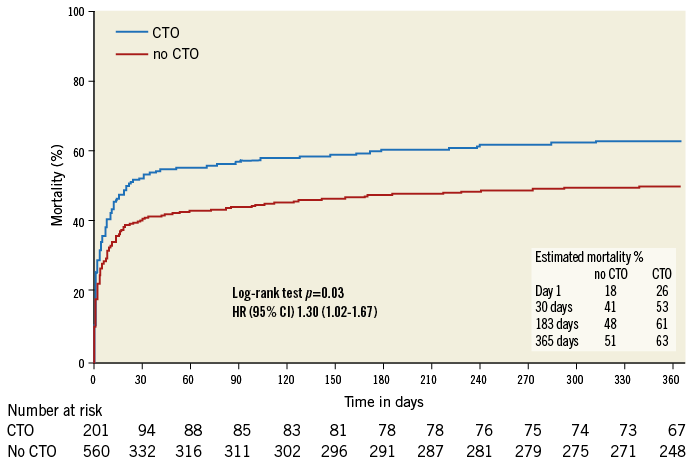
Figure 3. Adjusted Kaplan-Meier curve according to Cox regression model displaying one-year mortality difference between patients with and without a chronic total occlusion (CTO) in a non-infarct-related artery (blue line: with CTO; red line: without CTO).
The higher mortality at 12 months in the CTO group was mainly attributed to the higher mortality rate in the first 30 days. After day 30, there was no significant difference in mortality rates between the two groups (Figure 4).
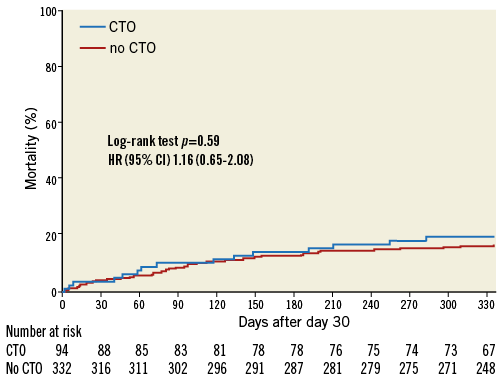
Figure 4. Adjusted Kaplan-Meier curve according to Cox regression model displaying mortality differences after 30 days between patients with and without a chronic total occlusion (CTO) in a non-infarct-related artery (blue line: with CTO; red line: without CTO).
In the first 30 days, patients with a CTO in a non-IRA suffered more ventricular arrhythmias requiring defibrillation (33% vs. 21%, OR 1.83, 95% CI: 1.28-2.62, p=0.002). The OR for ventricular fibrillation was 1.51 (95% CI: 1.01-2.25, p=0.04) and for ventricular flutter 2.22 (95% CI: 1.23-4.0, p=0.007). Occurrence of ventricular arrhythmias was significantly associated with higher mortality in patients with non-IRA CTO in comparison to patients without CTO (Figure 5). Furthermore, patients with CTO less often achieved haemodynamic stability (59% vs. 70%, OR 0.60, 95% CI: 0.43-0.84, p=0.003) than patients without a CTO in a non-IRA.
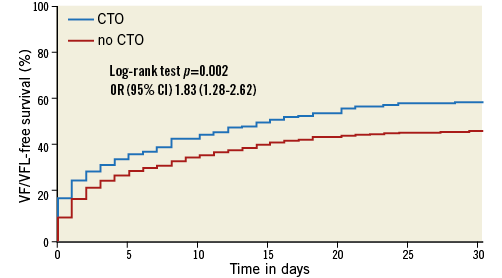
Figure 5. Kaplan-Meier curve showing impact of ventricular fibrillation (VF)/ventricular flutter (VFL) on survival in patients with and without a chronic total occlusion (CTO) in a non-infarct-related artery.
Discussion
The present substudy from the largest randomised study in CS published so far, the IABP-SHOCK II trial, and its accompanying registry showed a prevalence of a CTO in a non-IRA of 26%. Presence of a non-culprit lesion CTO was associated with an increased one-year mortality.
INCIDENCE AND CLINICAL RELEVANCE OF NON-IRA CTO IN CS
The currently observed prevalence of CTO in a non-IRA (26%) is in line with other reports ranging from 24 to 29%2,5,6. The development of CS after AMI is largely dependent on the extent of ischaemia. Collateral blood supply to the myocardium at risk limits the extent of ischaemic injury. In patients with CTO in a non-culprit lesion, the compensating capacity of collateral circulation is likely to be compromised. Furthermore, additional myocardium might be at risk due to impairment of collaterals from an IRA to the territory supplied by the CTO.
PROGNOSTIC RELEVANCE OF NON-IRA CTO IN CS PATIENTS
Recently, three published retrospective studies investigated the impact of a CTO in a non-IRA in STEMI patients presenting with CS2,5,6. Results of two of them showed that the presence of a CTO in a non-IRA was independently associated with increased mortality but both studies were limited by small sample size with only 292 and 141 patients included2,5. In contrast to the current findings, the third trial published by Hoebers et al included 609 patients with CS complicating STEMI. In this trial, multivessel disease but not CTO in a non-IRA was associated with 30-day mortality6. In our cohort of both STEMI and non-STEMI patients with CS, we observed a significantly higher unadjusted early (day of admission and 30-day), six-month, and cumulative one-year mortality in patients with a CTO in a non-IRA in comparison to patients without a CTO. In multivariable analysis, a CTO in a non-IRA was an independent predictor of mortality at 12 months, mainly attributed to the higher mortality rate in the first 30 days. A number of mechanisms may explain the markedly increased mortality rate in these patients including more pronounced negative left ventricular remodelling1, impaired reperfusion after primary PCI11, larger infarct size11 and increased susceptibility for life-threatening arrhythmias4. We reported previously and repeatedly in this analysis that multivessel disease was not an independent predictor of one-year mortality in our cohort8.
LEFT VENTRICULAR EJECTION FRACTION
In patients with CS complicating AMI, previous studies reported lower left ventricular ejection fraction in patients with associated CTO in a non-IRA2,5. This is consistent with our findings with a significantly lower left ventricular ejection fraction at admission in patients with a CTO in comparison to the group without CTO (30% vs. 39%, respectively; p<0.001). Again, Hoebers et al related the reduced ventricular function in patients with CS to the effect of multivessel disease rather than to the presence of a CTO in a non-IRA. Although this retrospective study included 609 patients with CS, one of its limitations is that echocardiography within 10 days was performed in only 177 patients (29%) of the overall CS cohort6.
REVASCULARISATION OF NON-IRA CTO
Current ESC guidelines recommend revascularisation of non-culprit lesions only in STEMI patients who are haemodynamically compromised with persistent ischaemia after PCI of the supposed culprit lesion12. In the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial, patients who underwent surgical revascularisation had a relatively favourable prognosis compared with patients who underwent PCI. This was explained by the higher degree of revascularisation achieved in the surgically treated patients13. However, treatment of a CTO during the index admission is probably not realistic and leads to the inability to use refined CTO techniques in long and complex procedures poorly tolerated soon after STEMI and/or infarct-related CS. In the recently published Percutaneous Intervention for Concurrent Chronic Total Occlusions in Patients With STEMI (EXPLORE) trial, in patients with STEMI and concurrent CTO, early PCI of the CTO did not show any benefit in terms of left ventricular function or volumes. However, major limitations of the EXPLORE trial are the insufficient power to detect differences in clinical endpoints as well as exclusion of high-risk patients such as those with CS14. In our trial patients, multivessel PCI was performed in about 37% of patients with multivessel disease with or without CTO in a non-IRA and was not associated with a survival benefit15. Clearly, data on the impact of complete revascularisation including revascularisation of CTO in the acute setting of CS on clinical outcome are lacking. However, this is being studied in the ongoing Prospective Randomized Multicenter Study Comparing Immediate Multivessel Revascularization by PCI Versus Culprit Lesion PCI With Staged Non-culprit Lesion Revascularization in Patients With Acute Myocardial Infarction Complicated by Cardiogenic Shock (CULPRIT-SHOCK) trial (ClinicalTrials.gov Identifier: NCT01927549)16.
VENTRICULAR ARRHYTHMIAS
We observed a higher incidence of ventricular arrhythmias requiring defibrillation at 30-day follow-up in CTO patients, which has never been investigated previously2,5,6. Increased susceptibility to arrhythmias after AMI is probably aggravated in the presence of a CTO in a non-IRA due to the fact that virtually all CTOs are associated with subsequent chronic ischaemia when tested by fractional flow reserve regardless of the maturity of collateral channels17. The heterogeneity of the ventricular excitability after AMI, which can be measured by prolonged QT dispersion, is presumed to increase the propensity for arrhythmic manifestations and arrhythmic death18. This is supported by the findings of Erdogan et al who reported that successful revascularisation of CTO results in improved regional heterogeneity of myocardial repolarisation reflected by decreased QT dispersion after PCI19. On long-term follow-up, presence of a CTO was associated with higher rates of ventricular arrhythmia and death in patients with ischaemic heart disease receiving an implantable cardioverter defibrillator for primary or secondary prevention of sudden cardiac death4. The presence of a CTO in a non-IRA was also independently associated with appropriate intracardiac defibrillator therapy4.
Limitations
The present study has several important limitations. Due to its retrospective nature, selection bias cannot be fully ruled out. The study follow-up duration was one year; more prolonged follow-up may be needed to investigate whether the hazardous effects of CTO in a non-IRA persist over time. Furthermore, we did not assess whether a CTO was successfully recanalised or not, which might have affected clinical outcome. Data regarding collaterals to the non-IRA CTO and angiographic core lab assessment were not available. Finally, an adequately powered randomised trial is needed to investigate whether complete revascularisation including CTO in the treatment of AMI complicated by CS leads to improved clinical outcomes.
Conclusions
The prevalence of a CTO in a non-IRA in patients with CS complicating AMI is high and associated with a significantly higher incidence of ventricular arrhythmias and a lower left ventricular function. Furthermore, in this high-risk group of patients, the presence of a CTO is an independent predictor of one-year mortality.
| Impact on daily practice The presence of a chronic total occlusion (CTO) in a non-infarct-related coronary artery is reported to be associated with worse prognosis in patients with CS complicating AMI. We observed a higher incidence of ventricular arrhythmias requiring defibrillation at 30-day follow-up in patients with a CTO in comparison to patients without a CTO, which may partly explain the worse prognosis in this high-risk group. Whether the prognosis of this high-risk group of patients can be improved by elective or immediate revascularisation of the CTO has to be addressed in randomised trials. |
Conflict of interest statement
The authors have no conflicts of interest to declare.