Abstract
Aims: This study sought to assess the prognostic impact of coronary chronic total occlusions (CTO) in patients presenting with ventricular tachyarrhythmias on admission.
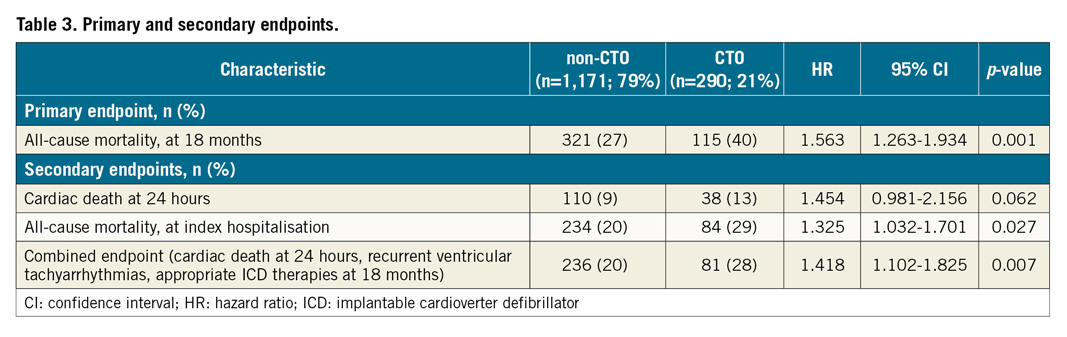
Methods and results: A large retrospective registry was used, including all consecutive patients presenting with ventricular tachyarrhythmias on admission and undergoing coronary angiography from 2002 to 2016. Patients with a CTO were compared with all other patients (non-CTO) for prognostic outcomes. Statistics comprised Kaplan-Meier and Cox regression analyses. Within a total of 1,461 consecutive patients included with ventricular tachyarrhythmias on admission, a CTO was present in 20%. At midterm follow-up of 18 months, the primary endpoint all-cause mortality had occurred in 40% of CTO patients compared to 27% of non-CTO patients (HR 1.563, 95% CI: 1.263–1.934; p=0.001). The rates of secondary endpoints were higher for in-hospital all-cause mortality at index (29% versus 20%, log-rank p=0.027) and the composite endpoint of cardiac death at 24 hours, recurrent ventricular tachyarrhythmias and appropriate ICD therapies at midterm follow-up (28% versus 20%, log-rank p=0.005). Mortality rates were highest in CTO patients with stable coronary artery disease (CAD), acute myocardial infarction and in patients surviving index hospitalisation.
Conclusions: In patients presenting with ventricular tachyarrhythmias on admission, the presence of a coronary CTO is independently associated with an increase of midterm all-cause mortality, in-hospital all-cause mortality and the composite endpoint of early cardiac death, recurrent ventricular tachyarrhythmias and appropriate ICD therapies.
Introduction
In up to 80% of patients, ventricular tachyarrhythmias and sudden cardiac death (SCD) are caused by acute myocardial infarction (AMI) and are associated with known or undiagnosed coronary artery disease (CAD) and its complications. About half of cardiac deaths after AMI are related to ventricular tachyarrhythmias, such as ventricular tachycardia (VT) or fibrillation (VF)1. The concept that ventricular tachyarrhythmias or SCD are potentially the corollary of risk of coronary chronic total occlusion (CTO) has only been looked at in a few clinical studies2,3,4,5. However, these studies evaluated the role of CTO on ventricular tachyarrhythmias and SCD in preselected and different populations, such as ischaemic cardiomyopathy, out-of-hospital cardiac arrest survivors and patients with an implanted cardioverter defibrillator (ICD)4,6,7. CTO is seen in about 18.4% of patients undergoing coronary angiography and may be linked to previous AMI or progressive CAD8. CTO may induce either acute myocardial ischaemia, varying post-AMI myocardial scarring, as well as peri-infarct changes including hibernating myocardium supplied by developing collateral connections, or adverse remodelling with myocardial dilation and dysfunction9. These pathoanatomic changes within the border zones may sustain an abnormal myocardial electrical milieu, which is characterised by slow inhomogeneous activation, ventricular repolarisation heterogeneity and ectopic activity, facilitating the development of ventricular tachyarrhythmias and consecutive cardiac death. Evaluation of the association of CTO as a potential trigger for ventricular tachyarrhythmias and early cardiac death is of great clinical interest. Therefore, this study evaluated the prognostic impact of CTO in patients presenting with ventricular tachyarrhythmias on admission.
Methods
STUDY PATIENTS, DESIGN AND DATA COLLECTION
The present study included retrospectively all patients presenting consecutively with ventricular tachyarrhythmias on hospital admission and undergoing coronary angiography from 2002 until 2016 at one institution. Using the electronic hospital information system, all relevant clinical data related to the index event were documented. The present study is derived from an analysis of the “Registry of Malignant Arrhythmias and Sudden Cardiac Death –Influence of Diagnostics and Interventions (RACE-IT)” and represents a single-centre retrospective registry including consecutive patients presenting with ventricular tachyarrhythmias and aborted cardiac arrest being acutely admitted to the University Medical Centre Mannheim (UMM), Germany (ClinicalTrials.gov identifier: NCT02982473) from 2002 until 2016. The registry was carried out according to the principles of the Declaration of Helsinki and was approved by the medical ethics committee II of the Faculty of Medicine Mannheim, University of Heidelberg, Germany.
DEFINITION OF STUDY GROUPS, INCLUSION AND EXCLUSION CRITERIA
For the present analysis, only patients presenting with ventricular tachyarrhythmias and with coronary angiography at index hospital stay were included in order to ensure reliable documentation of the presence of CAD and CTO. A coronary CTO was defined according to the European consensus document10,11. All coronary angiograms and reports were reassessed post hoc by two independent interventional cardiologists specialised in CTO-PCI for the present data analysis.
The CTO group comprised all patients with a native non-revascularised CTO in coronary vessels with a diameter >1.5 mm. Identification of CTO and CAD was based on the judgement of the investigating interventional cardiologist during routine care. The CTO group also included patients with acute revascularisation of a non-CTO vessel by PCI or coronary artery bypass grafting (CABG). Moreover, patients with an occluded bypass graft on the CTO vessel were allocated to the CTO group.
The control non-CTO group included all patients without CAD or CAD without a CTO, including CABG without a concomitant CTO and patients with acute PCI or CABG of non-CTO vessels. Patients with successfully revascularised CTOs either by CABG or PCI prior to ventricular tachyarrhythmias or SCD were included in the non-CTO group. Also, patients with successful CTO revascularisation during index hospitalisation either by PCI or CABG were included in the non-CTO group.
Overall exclusion criteria comprised patients without coronary angiography and coronary angiography after index hospital stay, patients without complete follow-up data regarding mortality and patients without documented ventricular tachyarrhythmias at index.
STUDY ENDPOINTS
The primary endpoint was all-cause mortality at midterm follow-up. Secondary endpoints were cardiac death occurring <24 hours after onset of ventricular tachyarrhythmias or an assumed unstable cardiac condition on admission, in-hospital all-cause mortality at index and the composite endpoint of cardiac death at 24 hours, first recurrent sustained ventricular tachyarrhythmias and first appropriate ICD therapies.
The overall follow-up period lasted until 2016. All-cause mortality was documented using our electronic hospital information system and by directly contacting state resident registration offices (bureau of mortality statistics) across Germany.
STATISTICAL ANALYSIS
Quantitative data are presented as mean±standard deviation, median and interquartile range (IQR), and ranges depending on the distribution of the data and were compared using the Student’s t-test for normally distributed data or the Mann-Whitney U test for non-parametric data. Deviations from a Gaussian distribution were tested by the Kolmogorov-Smirnov test. Spearman’s rank correlation for non-parametric data was used to test univariate correlations. Qualitative data are presented as absolute and relative frequencies and compared using the chi² test or the Fisher’s exact test, as appropriate. Univariable stratification was performed using the Kaplan-Meier method with comparisons between groups using univariable hazard ratios (HR) given together with 95% confidence intervals. Univariable and multivariable Cox regression models were applied and hazard ratios were given together with 95% confidence intervals. Cox regression models were applied in the entire cohort. Multivariable Cox regression models were developed using the “backward selection” option, where only statistically significant variables (p<0.05) were included and analysed simultaneously. Follow-up periods for evaluation of all-cause mortality were set when occurring within the individual index hospitalisation (in-hospital) and at 18 months (midterm) according to the median survival of CTO patients to guarantee the longest (and complete) follow-up of at least 50% of patients. Patients not meeting midterm follow-up were censored. The result of a statistical test was considered significant for p<0.05. SAS, release 9.4 (SAS Institute Inc., Cary, NC, USA), was used for statistics.
Results
STUDY POPULATION
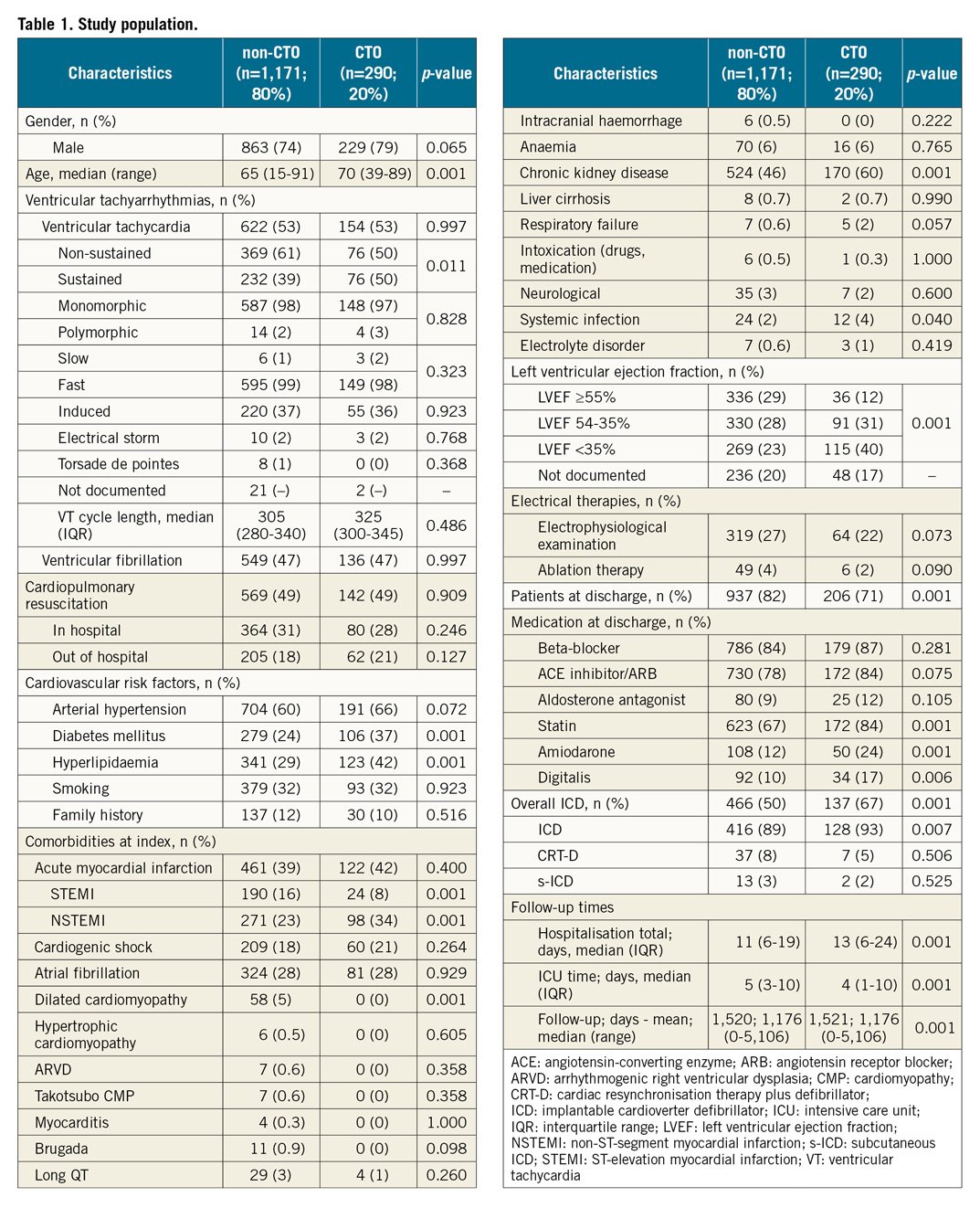
A total of 1,461 consecutive patients with ventricular tachyarrhythmias on admission at our institution underwent coronary angiography (Figure 1A). At least one CTO of a major coronary artery was found in 20% of patients. The CTO was most commonly located in the right coronary artery (RCA) in 42%, followed by the left anterior descending artery (LAD) in 17% and the circumflex (CX) in 19%, whereas 22% of patients had multiple CTOs (Figure 1B). CTO patients were more likely to suffer from diabetes, hyperlipidaemia, non-ST-elevation myocardial infarction (NSTEMI), chronic kidney disease and were more frequently treated with amiodarone and digitalis (Table 1). CTO patients revealed a higher rate of left ventricular ejection fraction (LVEF) <35% alongside a higher rate of ICD compared to non-CTO patients (67% versus 50%).
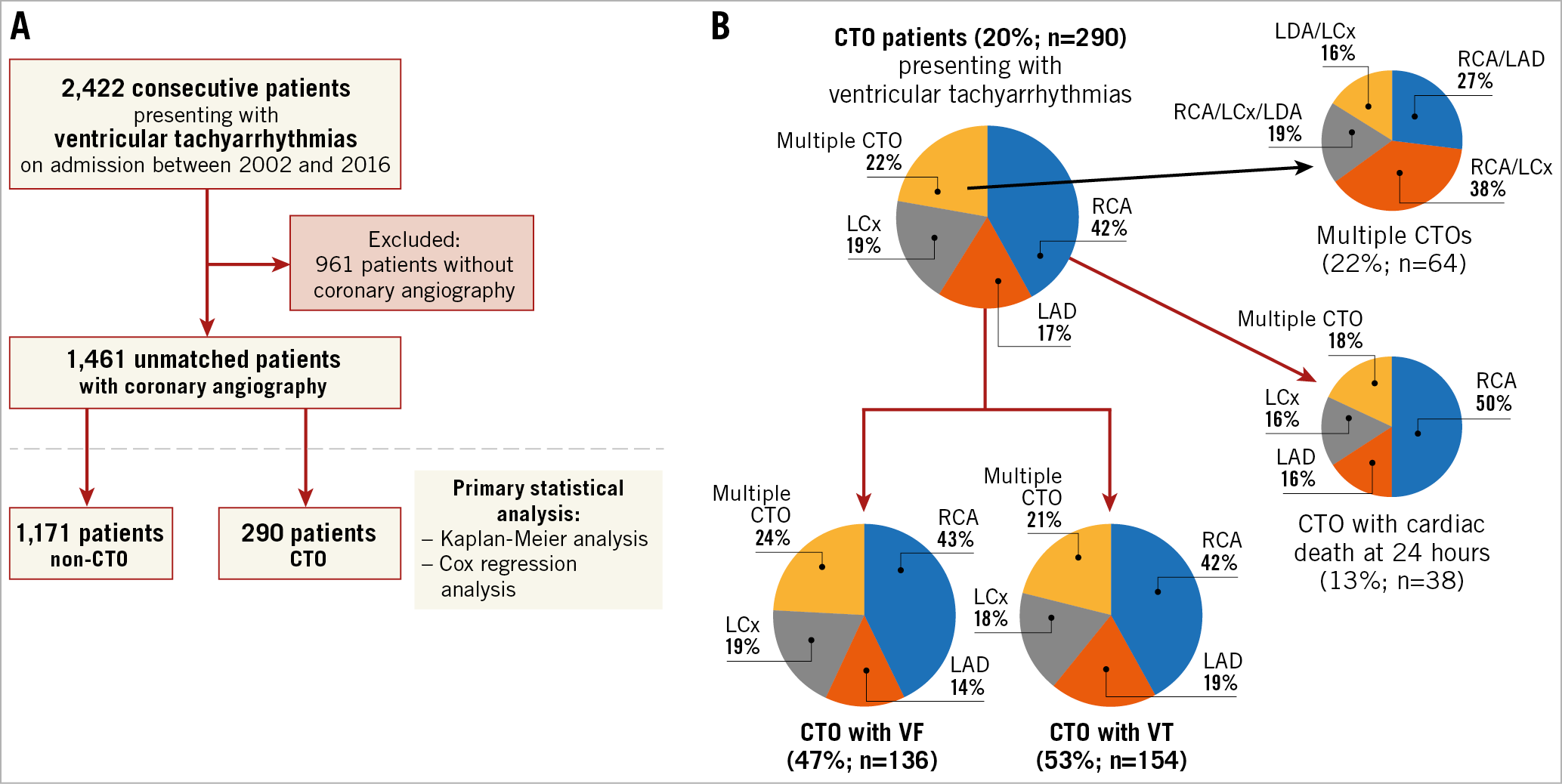
Figure 1. Patient selection and CTO distribution. Flow chart of patient selection (A). Distribution of CTO location (B).
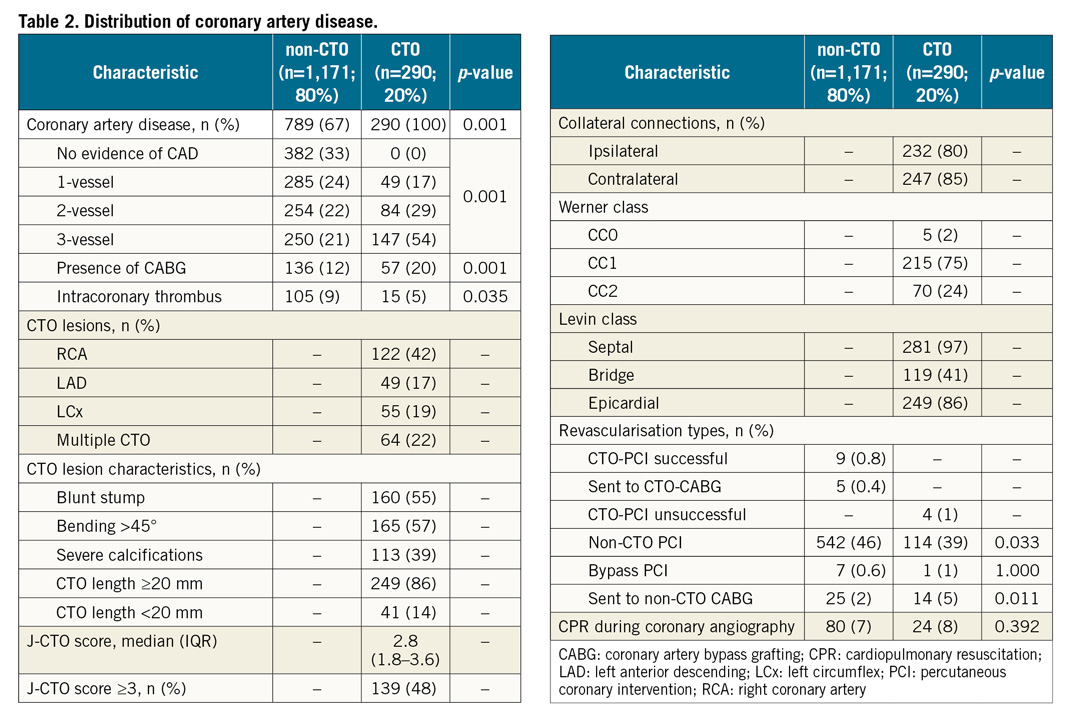
DISTRIBUTION OF CAD IN PATIENTS WITH VENTRICULAR TACHYARRHYTHMIAS
As shown in Table 2, 33% of non-CTO patients revealed no evidence of CAD, whereas CTO patients were more likely to have multivessel CAD and prior CABG. Non-CTO-PCI was more common in non-CTO compared to CTO patients (46% versus 39%, p=0.033) and PCI in bypass grafts was rarely performed. CTO revascularisation was performed rarely (in 14 patients, allocated to the non-CTO group: 9 with CTO-PCI and 5 with CTO-CABG). The median J-CTO score was 2.8 (IQR 1.8-3.6) in CTO patients presenting with ventricular tachyarrhythmias.
PROGNOSTIC IMPACT OF CTO
At midterm follow-up (18 months, IQR 5 days to 5.7 years), CTO patients had a higher all-cause mortality compared to non-CTO patients (mortality rate 40% versus 27%; log-rank p=0.001; HR 1.563, 95% CI: 1.263-1.934; p=0.001) (Figure 2), which was still evident after multivariable adjustment (HR 1.412, 95% CI: 1.081-1.843; p=0.011) (Figure 3).
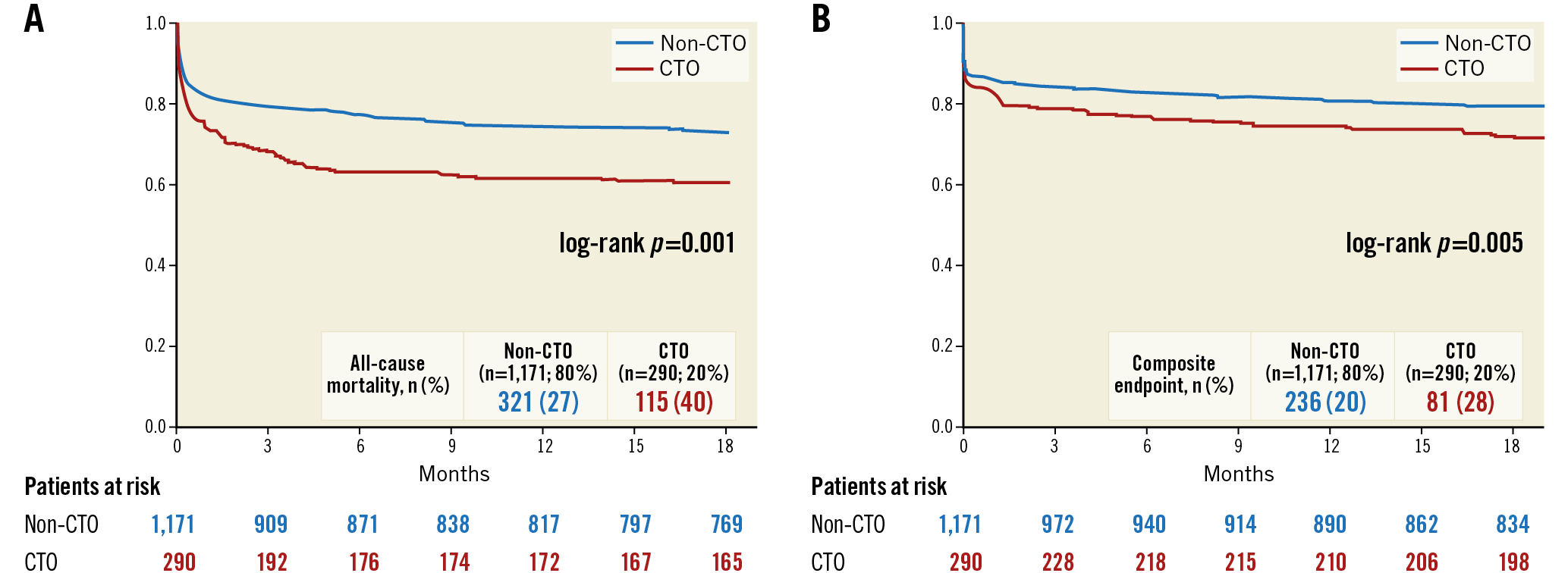
Figure 2. Kaplan-Meier analyses. Presence of a coronary CTO was associated with increased rates of the primary endpoint all-cause mortality at midterm follow-up (A), and the composite endpoint of cardiac death at 24 hours, recurrent ventricular tachyarrhythmias and appropriate ICD therapies at 18 months (B).
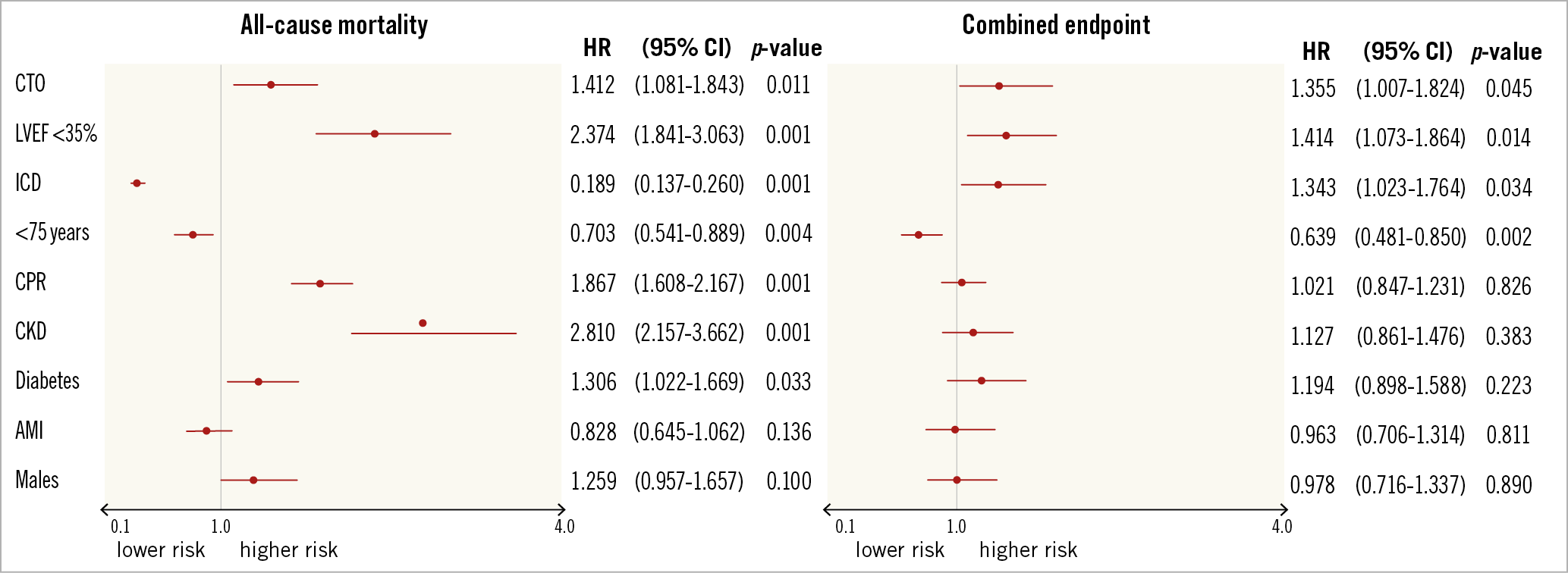
Figure 3. Multivariable Cox regression analyses. The presence of a coronary CTO was still associated with the primary endpoint all-cause mortality at midterm follow-up (after two steps of backward elimination) (left panel), as well as with the composite endpoint of cardiac death at 24 hours, recurrent ventricular tachyarrhythmias and appropriate ICD therapies at midterm follow-up (after six steps of backward elimination) (right panel).
The presence of a CTO was still univariably associated with increased midterm all-cause mortality in the subgroups of females (HR 2.072; p=0.001), males (HR 1.437; p=0.004), VT (HR 1.505; p=0.028) VF (HR 1.614; p=0.001), LVEF ≥35% (HR 1.792; p=0.002), non-ICD (HR 1.977; p=0.001), AMI (HR 1.424; p=0.017) and stable CAD patients (HR 1.540; p=0.013) (data not shown).
Regarding secondary endpoints, CTO patients revealed higher rates of in-hospital all-cause mortality at index (29% vs 20%, HR 1.325, 95% CI: 1.032-1.701; p=0.027) and higher rates of the composite endpoint of cardiac death at 24 hours, recurrent ventricular tachyarrhythmias and appropriate ICD therapies at midterm follow-up compared to non-CTO patients (28% versus 19%, log-rank p=0.005, HR 1.418, 95% CI: 1.102-1.825; p=0.007) (Figure 1B, Table 3). Associations of a CTO with the secondary composite endpoint were still univariably seen in the subgroups of males (HR 1.398; p=0.025), VT (HR 1.491; p=0.028), LVEF ≥35% (HR 1.721; p=0.012), non-ICD (HR 1.566; p=0.013) and stable CAD (HR 1.507; p=0.029) (data not shown).
Discussion
The present study evaluates the prognostic impact of coronary CTO in consecutive patients presenting with ventricular tachyarrhythmias on admission. These real-world data suggest that coronary CTO are common findings in up to 20% of patients presenting with ventricular tachyarrhythmias. The presence of at least one CTO is an important prognostic factor, associated with an increased risk of midterm all-cause mortality, in-hospital all-cause mortality at index and the composite endpoint of cardiac death at 24 hours, recurrent ventricular tachyarrhythmias and appropriate ICD therapies. The adverse prognostic value of a CTO was still evident in the subgroups of patients with stable CAD and AMI, as well as after multivariable adjustment, even in the entire study cohort. Therefore, this study consistently identifies the presence of a native non-revascularised CTO as a robust predictor of adverse outcomes in patients presenting with ventricular tachyarrhythmias on admission1.
Recent data have shown that sustained monomorphic VT in patients with previous AMI were less likely to be affected by coronary revascularisation1. Furthermore, myocardial revascularisation appeared to be unlikely to prevent SCD in patients with extensive myocardial scarring as well as in the presence of a markedly depressed LVEF1. Hence, VT was shown to be still inducible after surgical revascularisation in survivors of cardiac arrest in 80% of patients with multivessel CAD with a prevalence of VT and VF at index of 66%. Accordingly, VT recurrence occurred in post-AMI patients after successful revascularisation either by PCI or CABG even in the presence of LV dysfunction below 30%. Notably, VT and VF were still inducible in CAD patients independently of a complete or incomplete revascularisation by PCI or CABG. In contrast, catheter ablation only proved efficacious in reducing the rates of VT recurrence (with a higher recurrence rate in patients with CTO as compared to non-CTO patients)2, ICD therapy and symptom-free follow-up, but has never been proven to show better survival in patients presenting with VT and CAD1.
Whether CTO might be associated with the development of ventricular tachyarrhythmias has so far been investigated in only a small number of retrospective observational studies. The VACTO studies demonstrated significantly higher rates of mortality and ventricular tachyarrhythmias in 71 native CTO patients compared with 91 patients without CTO, and revealed a CTO as being an independent predictor for appropriate ICD therapy in ICD recipients for both primary and secondary prevention3,5. In contrast, Raja et al found no difference in mortality or ICD therapy for sustained VT between ICD patients with native CTO or revascularised CTO (total CTO patients n=213) and those without CTO (n=95). Notably, in this study the absence of a CTO in the left circumflex was protective with regard to ventricular tachyarrhythmias4. Surprisingly, the presence of a CTO in the territory of a previous AMI was shown to be associated with a higher rate of VT recurrence after VT ablation, as well as a higher repeat ablation rate2. In contrast, the major strength of the present study consists in the consecutive recruitment of patients with ventricular tachyarrhythmias and CTO straight from the admission scenario, where the adverse prognostic impact of a CTO was demonstrated both in the initially admitted study cohort and in those patients surviving and discharged from index hospitalisation.
Di Marco et al identified the presence of larger border zones in patients with an infarct-related CTO artery, along with reduced LVEF and renal impairment, as significant predictors for VT recurrence in 47 patients with and 37 patients without infarct-related CTO arteries2,7. VF originates mostly from an ischaemic substrate, whereas VT represents a scar-related substrate in the presence of ischaemic cardiomyopathy with a prior history of AMI, or in the context of structural or inflammatory heart disease1. Additionally, mechanisms such as early reperfusion, reduction of scars and infarct size, limitation of infarct expansion, recovery of function and improved collateral flow may in turn lead to better electrical stability within the myocardium9. It can be speculated that the presence of a CTO may adversely accentuate the above effects and may –unless revascularised– sustain a milieu of permanent electrical instability.
Study limitations
This observational and retrospective registry-based analysis reflects a realistic picture of consecutive healthcare supply of high-risk patients presenting with ventricular tachyarrhythmias immediately on hospital admission. The total number of patients with LVEF <35% and surviving index hospitalisation without further implantation of an ICD was low (19%, n=73), which may be attributed to improvement of LVEF above 35% at follow-up for the most part and lack of data documentation to a lesser degree. Myocardial scarring was not assessed within the present study, for instance by cardiac MRI, in all patients. Therefore, the prognostic benefit of potential “scar-related” responders to CTO revascularisation compared to non-responders was not assessed. Furthermore, rates of CTO revascularisation were very low (only 5%), and reliable conclusions about its prognostic effect in patients presenting with ventricular tachyarrhythmias are not possible.
Conclusions
In patients presenting with ventricular tachyarrhythmias on admission, the presence of a coronary CTO is independently associated with an increase of midterm all-cause mortality, in-hospital all-cause mortality and the composite endpoint of early cardiac death, recurrent ventricular tachyarrhythmias and appropriate ICD therapies.
|
Impact on daily practice In high-risk patients presenting with ventricular tachyarrhythmias on admission undergoing coronary angiography, the presence of a native non-revascularised CTO represents a consistently robust predictor of midterm all-cause mortality, irrespective of stable CAD or acute myocardial infarction, as well as of in-hospital index all-cause mortality and the composite endpoint of early cardiac death, recurrent ventricular tachyarrhythmias and appropriate ICD therapies. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.