
Mario Gaudino and David Taggart have eloquently summarised their prospective view for improving patient outcomes after coronary artery bypass grafting (CABG)1. Their perspective is optimistic. They challenge the interventional cardiology community to keep up with their evolutionary pace and suggest that “the ball is in our court”. It is exciting to respond and reassure them that we have already moved forward, arguably with longer strides than our surgical colleagues, and we will expand on how our treatments for patients with severe coronary disease should evolve together with them.
Firstly, the decision by a number of leading cardiac surgeons to participate in the SYNTAX trial facilitated much of our renewed mutual understanding about the pros and cons of percutaneous coronary intervention (PCI) vs. CABG2. Crucially, the performance of the study required a detailed assessment of the patient by the Heart Team comprising the participating surgeon and his interventional cardiology colleague. Predictably, the study showed that there was a large population of these patients with severe coronary disease who were best served with surgery and who were not considered for PCI. These patients were entered into a surgical registry, and the outcomes in this patient group were excellent and notably better than the randomised cohort. Within the cohort of patients randomised in the trial, the study demonstrated that bypass surgery was already superior to coronary stenting at one year and that the advantages of surgery continued to accrue as time passed3.
Predictably, all of our clinical practices have changed considerably in the last ten years. During that period, the EXCEL trial has suggested the probable equivalence of PCI and CABG for most patients with left main stenosis, especially those with less complex disease4. Within interventional cardiology, procedural and technological advances have been summated into the interventional approach used within the SYNTAX II trial5. This includes functional testing, improved stent technology, optimal stent deployment guided by intravascular imaging and prioritisation of complete revascularisation. Patients were selected using an algorithm derived from data acquired in the initial SYNTAX trial. This ensured that patients were only entered into the SYNTAX II registry where there was potential equipoise for outcome between CABG and PCI at four years. When CABG had a probable survival advantage it was performed preferentially. Outcomes from PCI performed using the new SYNTAX II strategy are being compared primarily with PCI outcomes from the original SYNTAX trial; however, there will also be a secondary hypothesis-generating comparison with the surgical results of SYNTAX.
When comparing revascularisation procedures performed with stents within the SYNTAX II and SYNTAX trials, there were notable differences. Physiology with pressure wire (iFR using a hybrid strategy) led to deferral of revascularisation in 31% of lesions, and only 2.64 lesions were treated in SYNTAX II compared to 4.02 lesions in SYNTAX, p<0.001 (reassuringly, rates of subsequent events attributable to these deferred lesions remain low two years after the procedure). Successful opening of completely occluded vessels was common, and consequently rates of complete revascularisation were high (successful opening of CTO in 87% vs. 53%). There was a high rate of use of stent imaging with intravascular ultrasound used in 87% vs. 4.8% and, importantly, this imaging resulted in optimisation of the result in 32% of cases in SYNTAX II. This stringent procedural technique and third-generation drug-eluting stent technology combined to give a very low rate of early stent thrombosis (0.7% vs. 2.6%) at one year. Assessment at one and more recently two years post procedure (Figure 1) shows superiority of this SYNTAX II approach to the PCI outcomes achieved with stents in SYNTAX. Further follow-up is envisaged for up to five years with comparisons with both the historical PCI and surgical outcomes.
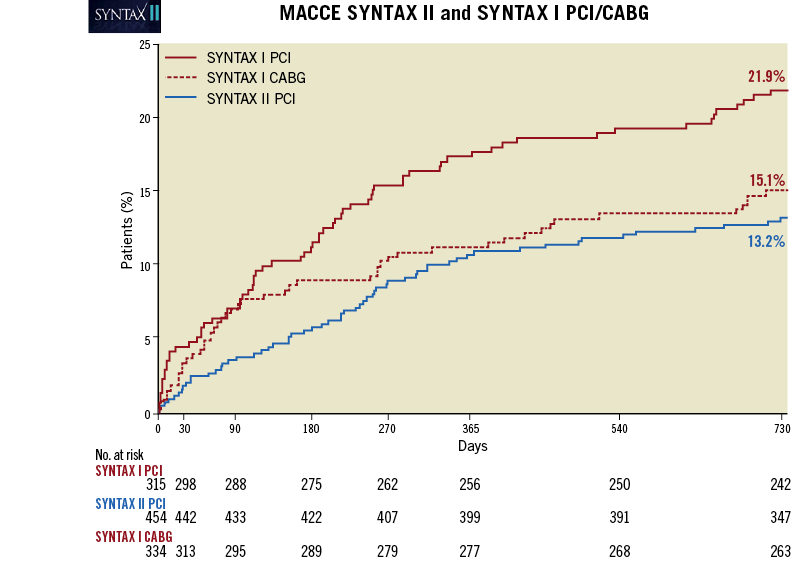
Figure 1. Two-year outcomes from the SYNTAX II trial presented by P.W. Serruys at EuroPCR, Paris, May 2018. Outcomes from PCI in SYNTAX II are shown in blue. For comparison, historical outcomes from the SYNTAX randomised cohorts are shown in red (solid line PCI and dashed line for CABG).
These emerging data from SYNTAX II will be augmented in the future by data from the FAME 3 trial6. This is a prospective randomised trial of a PCI or CABG strategy which also uses physiological assessment to ascertain which lesions to stent. The FAME 3 trial is close to completing its recruitment and the initial results will be available within a couple of years.
Non-invasive imaging of the coronary arteries is being transformed by CT scanning. Anatomical imaging is acquired accurately and quickly even in the presence of stents or complex disease in most cases. Adding data about the physiological severity of lesions from the CT scan without needing an invasive pressure wire assessment may be transformative. At EuroPCR in 2018, Patrick Serruys presented the initial results of the SYNTAX III REVOLUTION trial. In this study, 223 patients with multivessel disease were assessed using conventional angiography and then assessed with CT including FFRCT (HeartFlow, Redwood City, CA, USA). A high correlation between treatment decisions was evident, allowing observers to suggest that treatment decisions about revascularisation in multivessel disease might be based entirely on CT imaging within the near future.
Optimising medical therapy is as important for patients following PCI as it is for patients after CABG. There is still much work to do in this area, especially in patients with diabetes where the accrual of adverse events and the need for repeat revascularisation continue to exceed those in non-diabetic patients. Despite the enthusiasm for arterial grafting (of Drs Gaudino and Taggart in particular), the outcome of most CABG procedures remains placement of a single artery and two venous grafts. One could argue that rates of arterial surgery are disproportionately high (compared with standard CABG practice, especially in the UK) in both the EXCEL and SYNTAX trials. Cardiologists clearly recognise the limitations of the venous graft and welcome surgical strategies for complete arterial revascularisation. Unfortunately, practice change within surgery appears to be very slow and penetration is far from universal. The opportunity to explore hybrid revascularisation procedures recognises the variability not only of patients but also of their coronary arteries and their respective stenosis. Ensuring careful data collection and coordination between our specialist societies will consolidate any progress.
It is now over 10 years since we entered the last patient into the SYNTAX study, but the participation by a Heart Team in decision making has persisted in Oxford. In our opinion, this is the forum to decide strategy and settle the debate about optimal therapy. Previous suggestions that a patient should be offered the choice of two divergent opinions by an interventionalist and a surgeon are unworkable, divisive and confusing for the patient and their family. Our Heart Team discussions can be heated on occasion, but we have no doubt that this particular legacy of the SYNTAX trial is as important to patient care as the comparative results of the study. Looking forward, cardiac surgery and interventional cardiology practices must be drawn closer together rather than further apart. No reasonable interventional cardiologist would suggest that treatment with stents will always achieve better outcomes than CABG for all of their patients. Data from CT scanning will become more central within clinical pathways and information about myocardial viability will be more available. This will facilitate a more informed and individual decision which is based on the patient, the lesions, available expertise and, consequently, a projected outcome.
Personalised medicine is and will be as important in coronary disease as it is in oncology. Artificial intelligence and the ability to predict outcomes from previous experience should and will influence our decision making. Therapeutic partnerships occur daily when we discuss urgent and emergency cases. These relationships are optimised with scheduled regular meetings of the Heart Team. Mutual cooperation to embrace new technology facilitates the progression of therapy for our specialties but, more importantly, optimises outcome for each individual patient.
Conflict of interest statement
A. Banning is partially funded by the NHS NIHR Biomedical Research Centre Oxford and reports that the Oxford Heart Centre receives funding for an Interventional Fellowship from Boston Scientific. P.W. Serruys has no conflicts of interest to declare.

