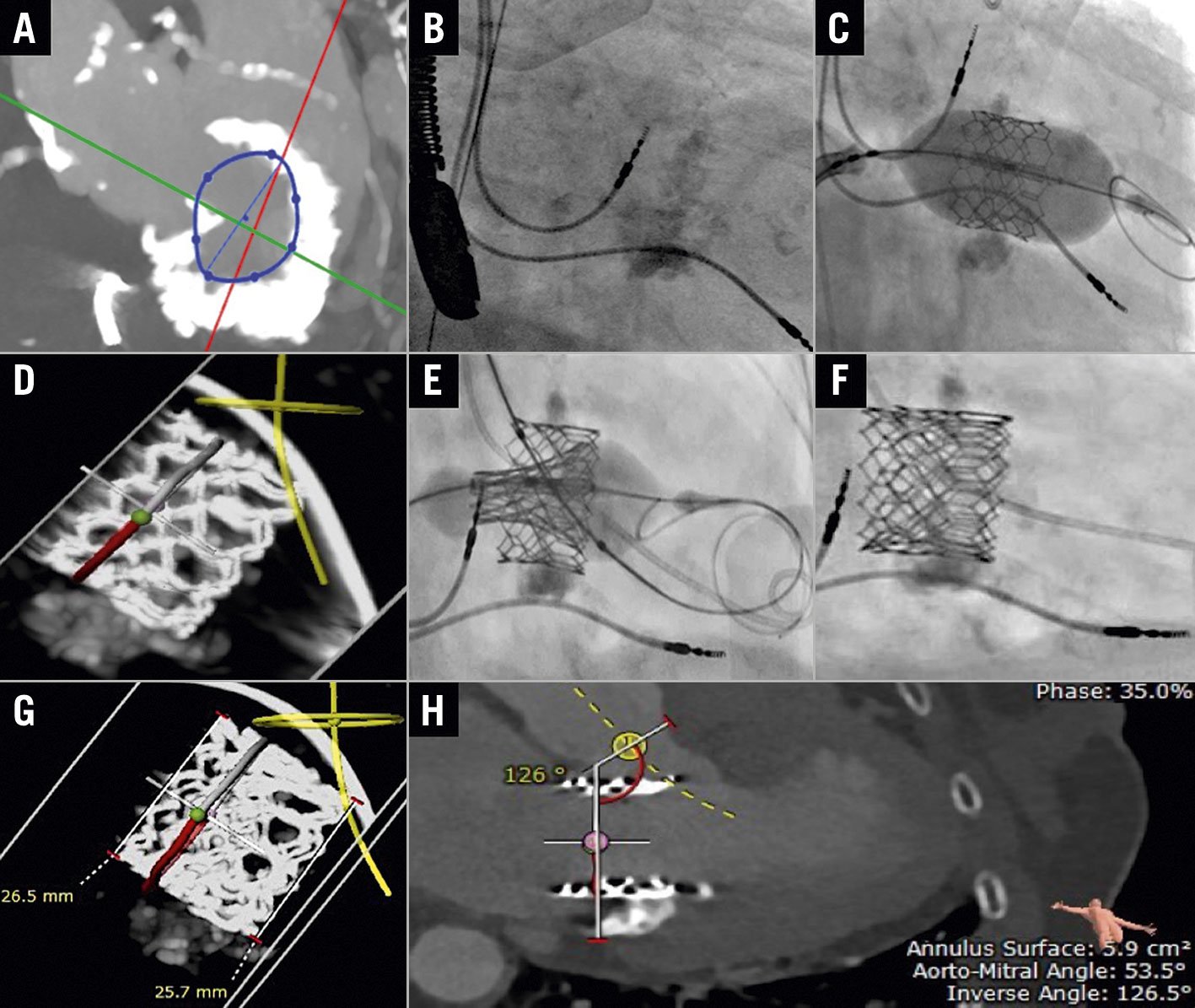
Figure 1. Redo transcatheter mitral valve replacement in mitral annular calcification for early valve failure. A) Severe mitral annular calcification (MAC) on computed tomography (CT). B) Severe MAC on fluoroscopy. C) Transseptal transcatheter mitral valve replacement (TMVR) in MAC using the first SAPIEN 3 valve on fluoroscopy. D) CT planning showing the first failed SAPIEN 3 valve. E) & F) TMVR valve-in-valve SAPIEN 3 26 mm deployment on fluoroscopy. G) & H) TMVR valve-in-valve SAPIEN 3 26 mm on CT scan.
We present the case of a 78-year-old female patient with a history of atrial fibrillation, severe calcific mitral valve stenosis (MS), and recurrent flash pulmonary oedema. She was deemed inoperable due to multiple comorbidities and dense mitral annular calcification (MAC) (Figure 1A, Figure 1B, Moving image 1).
She underwent a transseptal (TS) transcatheter mitral valve replacement (TMVR) in MAC in 2019 using a 26 mm SAPIEN 3 (Edwards Lifesciences) valve (Figure 1C, Moving image 2). Despite a neo-left ventricular outflow tract (neo-LVOT) area estimated at 277 mm2, she developed acute LVOT obstruction (LVOTO) with haemodynamic collapse (Moving image 3). Emergent alcohol septal ablation (ASA) of the first septal branch with 1.5 cc of pure alcohol was performed with immediate improvement of haemodynamics (Moving image 4).
Postoperative transthoracic echocardiography (TTE) showed a decrease in the transmitral mean gradient from 16 to 3 mmHg, with complete resolution of both MS and mitral regurgitation (MR), as well as a mild remnant LVOT gradient of 20 mmHg that did not change with the Valsalva manoeuvre. The patient was discharged on warfarin with a target international normalised ratio (INR) of 2.5-3.5 and significant improvement of her New York Heart Association Functional Class from Class IV to Class II. A three-month TTE showed normal mitral valve gradients and the patient remained asymptomatic until nine months later when she started experiencing worsening dyspnoea on exertion. Transoesophageal echocardiography (TEE) revealed an increasing gradient across the SAPIEN 3 valve with severe MR (Moving image 5). Repeat cardiac computed tomography (CT) showed some basal leaflet thickening with no overt thrombosis. The patient was started on warfarin regardless with no MR improvement six weeks later. Due to her worsening condition, the Heart Team opted for a redo TS valve-in-valve (ViV) TMVR. This time, CT planning showed a neo-LVOT=217.7 mm2 (Figure 1D).
Through a TS approach, an Edwards SAPIEN 3 (26 mm + 1 cc) was positioned across the failed transcatheter valve. A 20 x 40 mm Z-Med II balloon (B. Braun Medical) was also positioned in the LVOT. Under rapid pacing through the Safari wire (Boston Scientific), both devices were simultaneously inflated in a kissing fashion to prevent LVOTO, with the successful deployment of the new SAPIEN 3 valve (Figure 1E, Figure 1F). Intraprocedural TEE confirmed no paravalvular leak, minimal transmitral gradient, and no LVOTO (Moving image 6). Finally, a 16 mm septal occluder was used to close the atrial septal defect due to a predominant right-to-left shunt with hypoxia (Moving image 7).
TTE at discharge revealed a mean transmitral gradient of 4 mmHg with no regurgitation noted, as well as a significant decrease in pulmonary artery systolic pressure from 92 to 52 mmHg. The patient was maintained on chronic anticoagulation with close follow-up by our anticoagulation clinic. Her three-month follow-up echocardiography revealed a mitral mean pressure gradient (MPG) of 3 mmHg with no regurgitation. Repeat CT scan showed a well-seated circular SAPIEN 3 valve with no leaflet thickening or thrombus formation (Figure 1G, Figure 1H).
To the best of our knowledge, ViV TMVR has never been previously reported. We aim to highlight its possibility as management for early failure of TMVR in MAC with good outcomes if the risk of LVOTO remains low. LVOTO can be prevented by pre-emptive ASA, or conceptually by the kissing balloon manoeuvre, which secures the patent neo-LVOT while orienting the TMVR away from the LVOT1. Alternatively, laceration of the anterior mitral leaflet to prevent outflow obstruction (the LAMPOON technique) can be attempted, with the antegrade approach being the currently favoured one. Tip-to-base LAMPOON is a simplified version applicable when the aortomitral curtain is protected by a surgical valve2. Longer follow-up will be necessary to determine if redo TMVR is durable.
Conflict of interest statement
F. Sawaya is a TAVR proctor for Edwards Lifesciences, Medtronic, Abbott Vascular, and Boston Scientific. G. Tang is a physician proctor and consultant for Medtronic, a consultant for Abbott Structural Heart and NeoChord, and a physician advisory board member for Abbott Structural Heart and JenaValve. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Severe MAC on A) 2D TEE, B) 2D TEE with colour Doppler, and C) 3D TEE.
Moving image 2. Good function of the first TMVR with no paravalvular leak. A) Fluoroscopic valve deployment, B) on 2D TEE, C) on 2D TEE with colour Doppler, and D) on 3D TEE.
Moving image 3. Severe turbulence at the LVOT on 2D TEE colour Doppler.
Moving image 4. A) Wire and OTW 1.5×8 mm balloon in the first septal, B) opacification of basal septum with pure alcohol on 2D TEE.
Moving image 5. Severe bioprosthesis central MR on A) 2D TEE, and on B) 3D TEE.
Moving image 6. TMVR ViV SAPIEN 3, 26 mm. A) Deployment simultaneously inflated in a kissing fashion with a 20×40 mm balloon parked in the LVOT on fluoroscopy, B) on 2D TEE, C) on 2D TEE colour Doppler, and D) on 3D TEE.
Moving image 7. ASD occluder across the septum on fluoroscopy.