Abstract
Background: When a balloon-expandable transcatheter heart valve (THV) is chosen to treat a failed balloon-expandable THV, there is a risk of underexpansion with a potential impact on performance.
Aims: We aimed to assess the impact of pre- and post-dilatation on the expansion of balloon-expandable THVs after redo-transcatheter aortic valve implantation (TAVI).
Methods: Redo-TAVI was performed on the bench with a 23 mm SAPIEN 3 (S3) implanted within a 23 mm SAPIEN XT (SXT) or a 23 mm S3, both of which served as the “failed” THVs. Pre- and/or post-dilatation was performed using a 23 mm non-compliant TRUE balloon. Expansion of the index and redo-THVs were assessed before and after pre-/post-dilatation using microcomputed tomography (micro-CT), and THV hydrodynamic testing was conducted.
Results: Without pre- or post-dilatation, the S3 was underexpanded, for all combinations, particularly in the mid-portion of the THV (18.6 mm and 19.7 mm representing 81% and 86% of the nominal diameter inside the SXT and S3, respectively). Pre- and post-dilatation had an additive effect on diameter expansion of the redo-THV, which remained constrained in most combinations. The only combination to achieve nominal expansion was the S3 in S3 when both pre- and post-dilatation were performed. The S3 remained underexpanded inside the SXT despite pre- and post-dilatation (93% in the mid-portion). Improved redo-THV expansion was accompanied by 2.7 mm (12%) overexpansion of the index THV. While all samples had acceptable hydrodynamic performance, the underexpanded samples had worse leaflet pinwheeling.
Conclusions: When performing redo-TAVI with a 23 mm S3 inside a 23 mm SXT or S3, only the S3 in S3 with the use of pre- and post-dilatation reached full expansion. This underlines the importance of CT assessment of THV expansion and the role of pre-/post-dilatation.
Introduction
Patients with a transcatheter heart valve (THV) may develop structural valve degeneration, which may require reintervention. Redo-transcatheter aortic valve implantation (TAVI) is a treatment option for patients with failed THVs1. Early experience with redo-TAVI has shown favourable outcomes in selected patients2.
Overall, clinical experience is limited with redo-TAVI, and the optimal THV choice and positioning remain unknown. Some paired configurations of THVs in redo-TAVI may lead to suboptimal expansion or function which may impact THV performance and durability. For example, in the case of a failed short-frame balloon-expandable THV, the index failed valve may be underexpanded as previously reported3, and this might subsequently impact the expansion of the redo-THV following redo-TAVI. Use of a tall-frame valve with supra-annular leaflets may be associated with lower gradients, but this must be balanced against a high neoskirt which may potentially prevent future coronary access. If another short-frame valve is used for redo-TAVI, the redo-THV may be underexpanded and lead to elevated residual gradients4. Additionally, recent data have shown that underexpansion of the SAPIEN 3 (S3; Edwards Lifesciences) THV is associated with increased hypoattenuated leaflet thickening (HALT) and possibly an increased risk of mortality3. Post-dilatation of the THV following redo-TAVI, with or without predilatation of the failed THV, can be considered to optimise expansion. The feasibility and efficacy of balloon dilatation to optimise THV expansion following redo-TAVI is, however, unknown. The presence of 2 layers of THV frame may limit the effectiveness of post-dilatation or may require higher pressure and risk damaging the THV leaflets.
The present bench study reports the impact of pre- and/or post-dilatation on THV function and expansion when performing redo-TAVI in SAPIEN XT (SXT; Edwards Lifesciences) and S3 THVs.
Methods
Testing was performed at the Cardiovascular Translational Laboratory (Centre for Heart Lung Innovation, Vancouver, BC, Canada). The present work is a bench study in which no human or animal subjects were included and, thus, did not require ethical approval.
VALVES
SAPIEN XT and S3 THVs were considered the “failed” or “index” THVs in this analysis, and an S3 was always used as the new redo-THV. For all combinations, 23 mm THVs were used. One of the relevant differences between the SXT and the S3 is the frame height when deployed; when nominally deployed, the 23 mm SXT has a height of approximately 14 mm while the height of the 23 mm S3 is 18 mm5. Further THV design and features have been previously described in detail6.
REDO-TAVI BENCH PROCEDURE
For implantation of an S3 into an SXT, the S3 was positioned with the outflow approximately 20% above the outflow of the SXT, to maximise the effective orifice area (EOA) and reduce the residual transvalvular gradient7. Since the S3 is about 20% taller than the SXT, this positioning resulted in an alignment of the inflow of both THVs after deployment. For implantation of an S3 into an S3, the THV was positioned with the 2 outflows aligned.
PRE- AND POST-DILATATION PROCEDURE
Pre- and/or post-dilatation was performed using a 23 mm non-compliant TRUE dilatation balloon valvuloplasty catheter (Bard Peripheral Vascular, Inc.)8. Balloons were inflated using a large syringe, indeflator and high-pressure stopcock. The balloon was filled by hand injection with the syringe first, and then, the stopcock was opened to the indeflator to pressurise the balloon. The balloon was pressurised to 6 atmospheres, corresponding to the rated burst pressure of the balloon. The TRUE balloon was selected since it has been previously shown that a reliable overexpansion of the SXT can be achieved at 6 atmospheres with this type of non-compliant balloon but not with a semi-compliant balloon9.
In total, 8 configurations were tested and measured once:
1) S3 in SXT without predilatation, without post-dilatation.
2) S3 in SXT without predilatation, with post-dilatation.
3) S3 in SXT with predilatation, without post-dilatation.
4) S3 in SXT with predilatation, with post-dilatation.
5) S3 in S3 without predilatation, without post-dilatation.
6) S3 in S3 without predilatation, with post-dilatation.
7) S3 in S3 with predilatation, without post-dilatation.
8) S3 in S3 with predilatation, with post-dilatation.
Predilatation was performed on the index THV, before deploying the redo-THV, while post-dilatation was performed with the second THV in place (Central illustration).
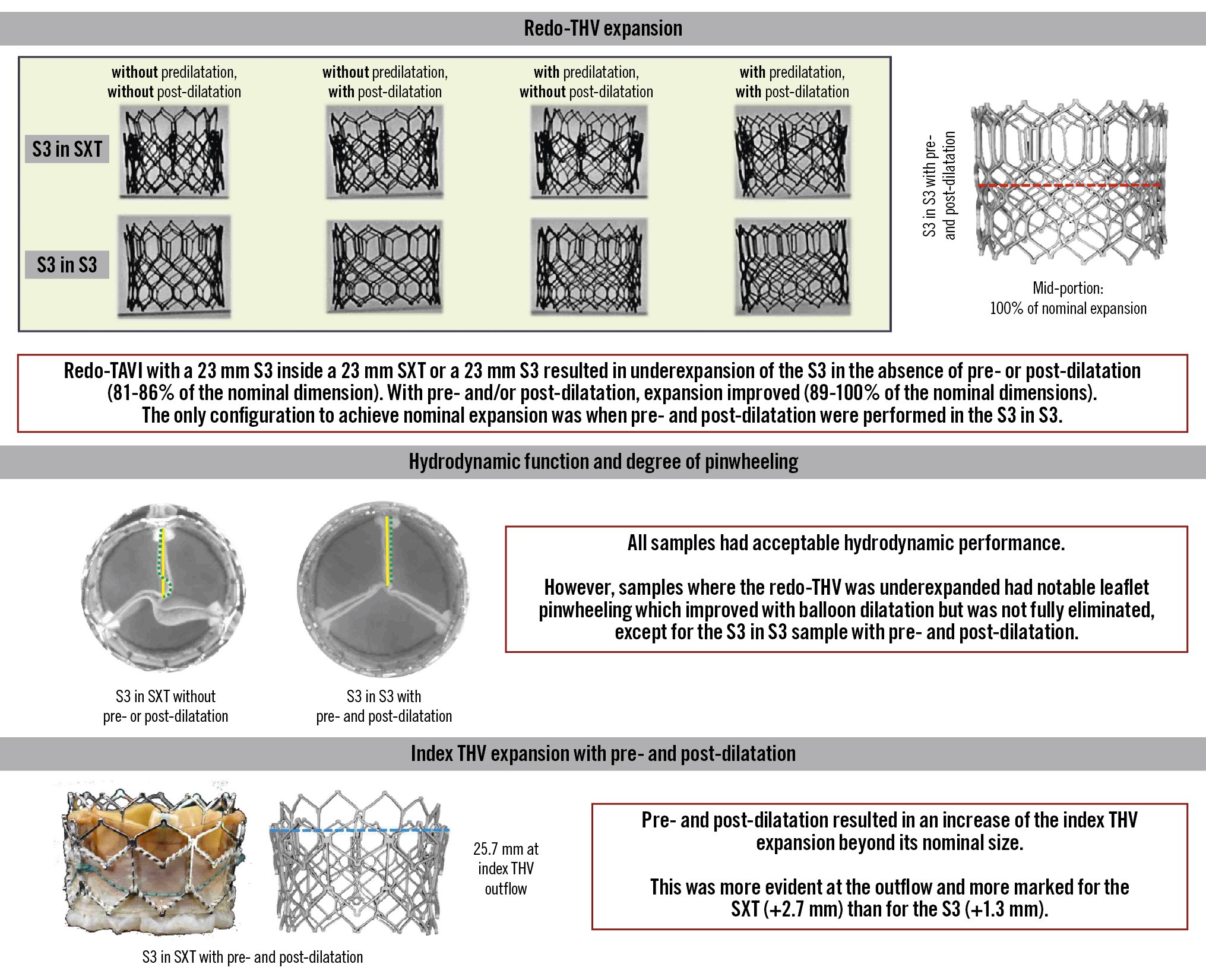
Central illustration. Redo-TAVI with a 23 mm SAPIEN 3 in a 23 mm SAPIEN XT or SAPIEN 3: impact of pre- and post-dilatation using a TRUE dilatation balloon on final THV expansion and performance. S3: SAPIEN 3; SXT: SAPIEN XT; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve
IMAGING
Multimodality imaging was performed with photography, high-speed video, fluoroscopy and microcomputed tomography (micro-CT); high resolution photography and video were performed at the same magnification and fixed camera height. Photos and high-speed video were taken following redo-TAVI and after post-dilatation. Micro-CT was performed for each sample at baseline and after post-dilatation. All images were taken using the Nikon XT H 225 ST microfocus X-ray tomography system (Nikon Metrology). A three-dimensional reconstruction of the micro-CT images was obtained using VGSTUDIO MAX software (version 3.5; Volume Graphics GmbH). Fluoroscopy of each sample was performed at baseline and after post-dilatation. Fluoroscopic images were acquired at a standard adult cardiac catheterisation laboratory (GE HealthCare, Chicago, IL, USA).
MICRO-CT MEASUREMENTS
Measurements were taken at the inflow, outflow, and mid-portion of the failed THV as well as at the inflow, outflow and mid-portion of the redo-THV. The area at each level was measured using Fiji imaging software (version 1.51f53; ImageJ) and compared to the labelled nominal size (23 mm). Measurements were taken at the mid-strut level as previously reported for surgical and transcatheter heart valves1011. This avoids under- or overestimation of the diameter due to blooming artefact when measuring the outer or inner diameter. Each measurement was repeated 3 times, and the mean value is reported. Of note, no standard deviation is reported for the purposes of simplicity, as the standard deviation was <1% for all samples.
PINWHEELING
Pinwheeling refers to the twisting of the leaflet-free edges, which results from excessive leaflet redundancy12. Pinwheeling can be quantified using the pinwheeling index but can also be assessed visually as none, mild, moderate, or severe13. Here, pinwheeling was visually assessed in the 8 configurations tested using high-speed videos.
HYDRODYNAMIC ASSESSMENT
Hydrodynamic testing was performed before and after post-dilatation, using a commercially available pulse duplicator (ViVitro Labs). Valves were tested in accordance with ISO 5840-3:2021 guidelines12. THVs were sealed in a holder fabricated from silicone with a Shore A durometer hardness of 40±5. The test fluid used was 0.9±0.2% sodium chloride test solution maintained at 37±2°C containing 1 drop/L of Cosmocil (Arxada), a bactericide. Valves were tested on the aortic side of the pulse duplicator with a spring-loaded disc valve (ViVitro Labs) on the mitral side of the pulse duplicator. Measurements were based on average results taken from 10 consecutive cycles. Pulsatile forward flow performance was tested at a nominal beat rate of 70±1 beats per minute, systolic duration of 35±5%, mean aortic pressure of 100±2 mmHg, and simulated cardiac outputs of 5.0±0.1 L/min. The mean gradient (MG) and EOA were assessed.
STATISTICS
Hydrodynamic variables are reported as mean±standard deviation (SD).
Results
Figure 1 shows photography and fluoroscopy of the different redo-TAVI combinations according to the pre-/post-dilatation strategy.
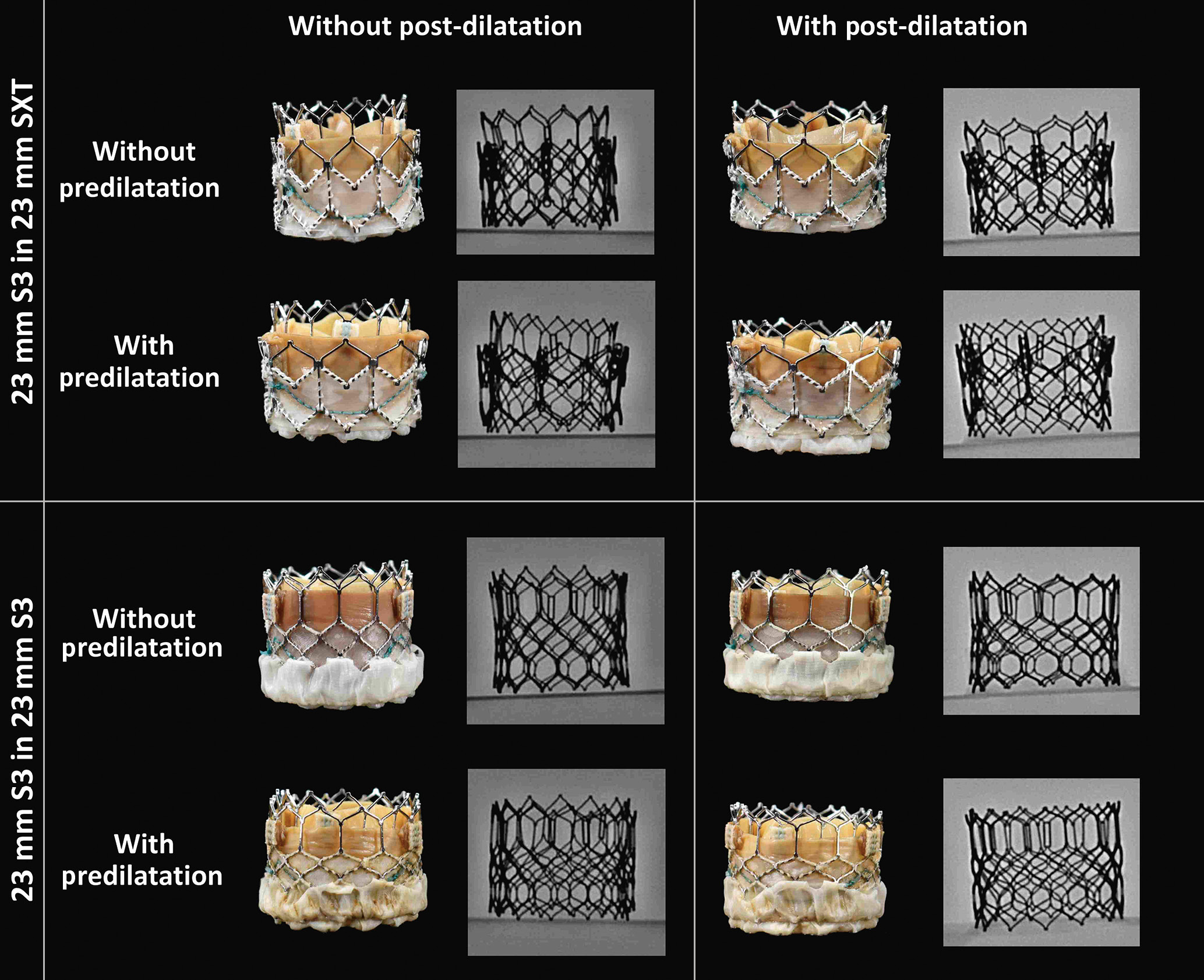
Figure 1. High-resolution photos and fluoroscopy of the different SAPIEN redo-TAVI combinations. S3: SAPIEN 3; SXT: SAPIEN XT; TAVI: transcatheter aortic valve implantation
THV EXPANSION BY MICRO-CT
Detailed dimensions at each level (inflow, outflow, and mid-portion) of the redo and index THVs for the 8 configurations tested can be found in Table 1 and Table 2, respectively. Figure 2 outlines the relative increase in diameter according to the pre-/post-dilatation strategy in the mid-portion of the valve, which was the most constrained THV segment.
Table 1. Micro-CT dimensions of the redo-THV.
| Redo-TAVI configuration | Mean diameter (mm) | ||||||
| Inflow | Mid-portion | Outflow | |||||
| Without post-dilatation | With post-dilatation | Without post-dilatation | With post-dilatation | Without post-dilatation | With post-dilatation | ||
| S3 in SXT | Without predilatation | 20.4 | 22.1 | 18.6 | 21.2 | 20.7 | 23.8 |
| With predilatation | 21.4 | 23.0 | 20.1 | 21.5 | 21.3 | 23.3 | |
| S3 in S3 | Without predilatation | 21.0 | 22.7 | 19.7 | 21.6 | 21.6 | 23.3 |
| With predilatation | 21.7 | 22.8 | 20.3 | 23.0 | 21.5 | 23.2 | |
| CT: computed tomography; S3: SAPIEN 3; SXT: SAPIEN XT; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve | |||||||
Table 2. Micro-CT dimensions of the index THV.
| Redo-TAVI configuration | Mean diameter (mm) | ||||||
| Inflow | Mid-portion | Outflow | |||||
| Without post-dilatation | With post-dilatation | Without post-dilatation | With post-dilatation | Without post-dilatation | With post-dilatation | ||
| S3 in SXT | Without predilatation | 22.5 | 23.4 | 22.5 | 23.8 | 22.8 | 25.0 |
| With predilatation | 23.4 | 23.4 | 24.2 | 24.3 | 25.2 | 25.7 | |
| S3 in S3 | Without predilatation | 22.6 | 24.1 | 21.5 | 23.3 | 22.7 | 24.3 |
| With predilatation | 23.6 | 23.8 | 23.4 | 23.6 | 23.4 | 24.1 | |
| CT: computed tomography; S3: SAPIEN 3; SXT: SAPIEN XT; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve | |||||||
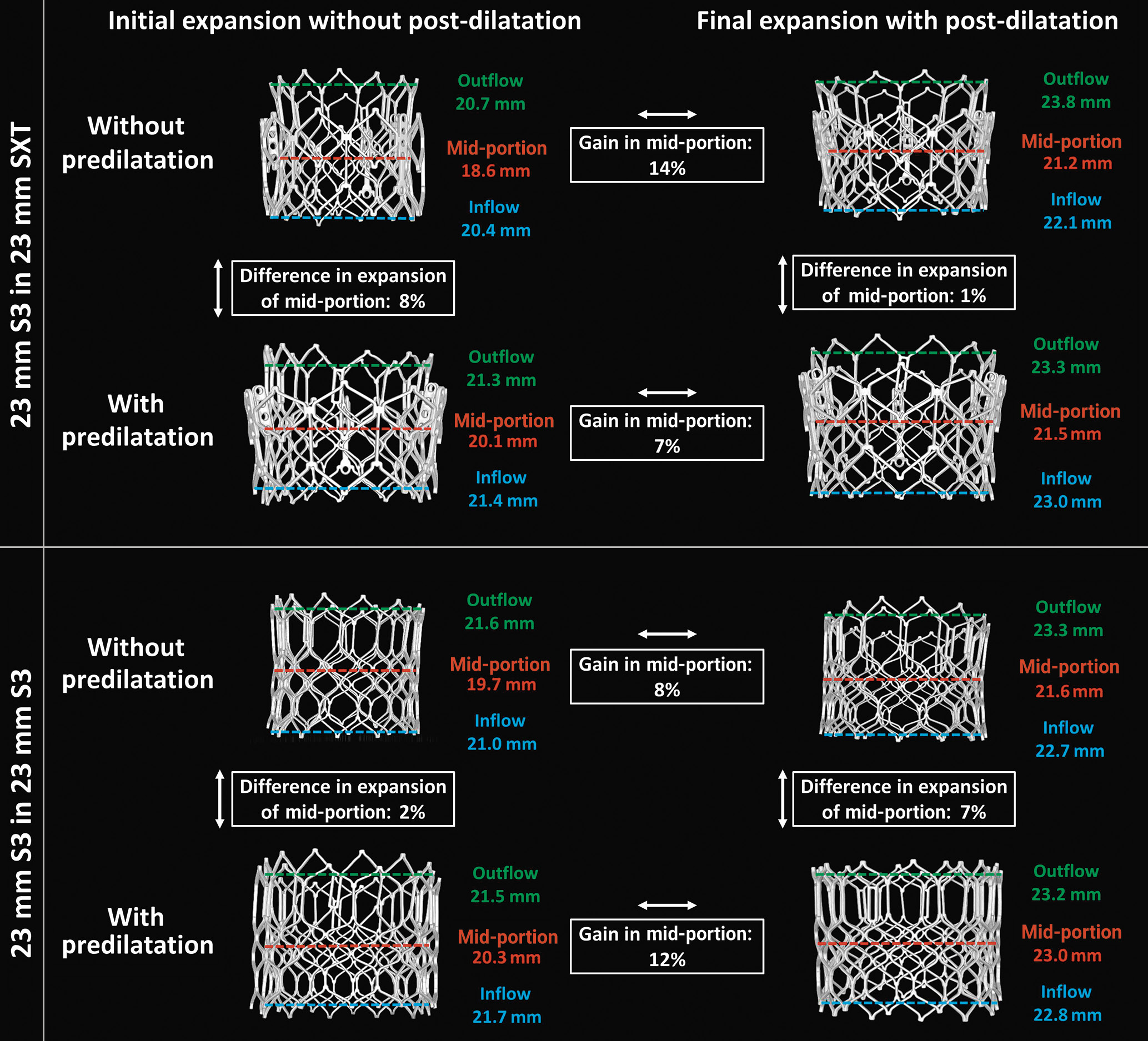
Figure 2. Micro-CT measurements of redo-THV expansion at the inflow, mid-portion and outflow according to procedural scenario. micro-CT: microcomputed tomography; S3: SAPIEN 3; SXT: SAPIEN XT; THV: transcatheter heart valve
DIMENSIONS OF THE REDO-THV
Redo-TAVI with a 23 mm S3 in a 23 mm SXT
Overall, in the SXT, in the absence of pre- or post-dilatation, the S3 was severely underexpanded in its mid-portion (18.6 mm, 81% of nominal diameter). Predilatation allowed for an improved S3 frame expansion, and the use of post-dilatation increased expansion only when predilatation was not performed.
In the absence of predilatation, the mean diameters at the inflow, mid-portion and outflow of the S3 were 20.4 mm, 18.6 mm (81% of nominal diameter) and 20.7 mm, respectively. Following post-dilatation, these dimensions increased to 22.1 mm, 21.2 mm (92% of nominal diameter), and 23.8 mm, respectively.
When predilatation was performed, the mean diameters at the inflow, mid-portion and outflow of the S3 were 21.4 mm, 20.1 mm (87% of nominal diameter) and 21.3 mm, respectively. This represents an 8% difference in expansion of the mid-portion compared to the strategy without predilatation. Following post-dilatation, these dimensions increased to 23.0 mm, 21.5 mm (94% of nominal diameter) and 23.3 mm, respectively. Compared to post-dilatation only, the combination of pre- and post-dilatation resulted in a 1% difference in the final expansion.
Irrespective of the pre-/post-dilatation strategy, the midpoint of the S3 remained underexpanded when performing redo-TAVI in the SXT, despite improved expansion at the inflow and outflow.
Redo-TAVI with a 23 mm S3 in a 23 mm S3
Similarly to what was observed in the SXT, redo-TAVI in the S3 without pre- or post-dilatation led to underexpansion of the redo-THV (19.7 mm, 86% of nominal diameter). Unlike in the SXT, pre- and post-dilatation had an additive effect on expansion of the redo-THV. In the absence of predilatation, the mean diameter at the inflow, mid-portion and outflow of the S3 were 21.0 mm, 19.7 mm (86% of nominal diameter) and 21.6 mm, respectively. Following post-dilatation these dimensions increased to 22.7 mm, 21.6 mm (94% of nominal diameter), and 23.3 mm, respectively.
When predilatation only was performed, the mean diameters at the inflow, mid-portion and outflow of the S3 were 21.7 mm, 20.3 mm (88% of nominal diameter) and 21.5 mm, respectively. This represents a 2% difference in expansion of the mid-portion compared to the strategy without predilatation. When post-dilatation was added to predilatation, these dimensions increased to 22.8 mm, 23.0 mm (100% of nominal diameter) and 23.2 mm, respectively.
Only the combination of performing both pre- and post-dilatation resulted in full nominal expansion of the mid-portion of the S3.
DIMENSIONS OF THE INDEX THV
The dimensions of the index THV increased beyond nominal values when pre- and/or post-dilatation were performed. This phenomenon was more marked with the SXT than the S3, likely reflecting the increased thickness at the commissural post due to the different frame designs. In consequence, the increase in expansion was more marked at the outflow than at the inflow. Thus, following post-dilatation, the index SXT outflow was overexpanded by almost 3 mm, while the index S3 outflow was overexpanded by only 1 mm. At the level of the inflow and mid-portion, this increase was about 1 mm for with the SXT and less than 0.5 mm with the S3 (Table 2).
Redo-TAVI with a 23 mm S3 in a 23 mm SXT
In the absence of predilatation and post-dilatation, the mean diameters at the inflow, mid-portion and outflow of the index SXT were 22.5 mm, 22.5 mm and 22.8 mm, respectively. When both pre- and post-dilatation were performed, these dimensions increased beyond the nominal size to 23.4 mm, 24.3 mm and 25.7 mm, respectively.
Redo-TAVI with a 23 mm S3 in a 23 mm S3
A similar trend was observed when the index THV was the S3. In the absence of pre- and post-dilatation, the index THV was also underexpanded with a mean diameter at the inflow, mid-portion and outflow of 22.6 mm, 21.5 mm and 22.7 mm, respectively. When pre- and post-dilatation where performed, these dimensions increased beyond the nominal size to 23.8 mm, 23.6 mm and 24.1 mm, respectively.
PINWHEELING
In the absence of predilatation, severe pinwheeling was observed in both samples, which was reduced using pre- and post-dilatation. Pinwheeling was improved for the S3 in S3 sample when predilatation was performed, and the only sample where no pinwheeling was observed was the 23 mm S3 in 23 mm S3 when both pre- and post-dilatation were performed (Figure 3).
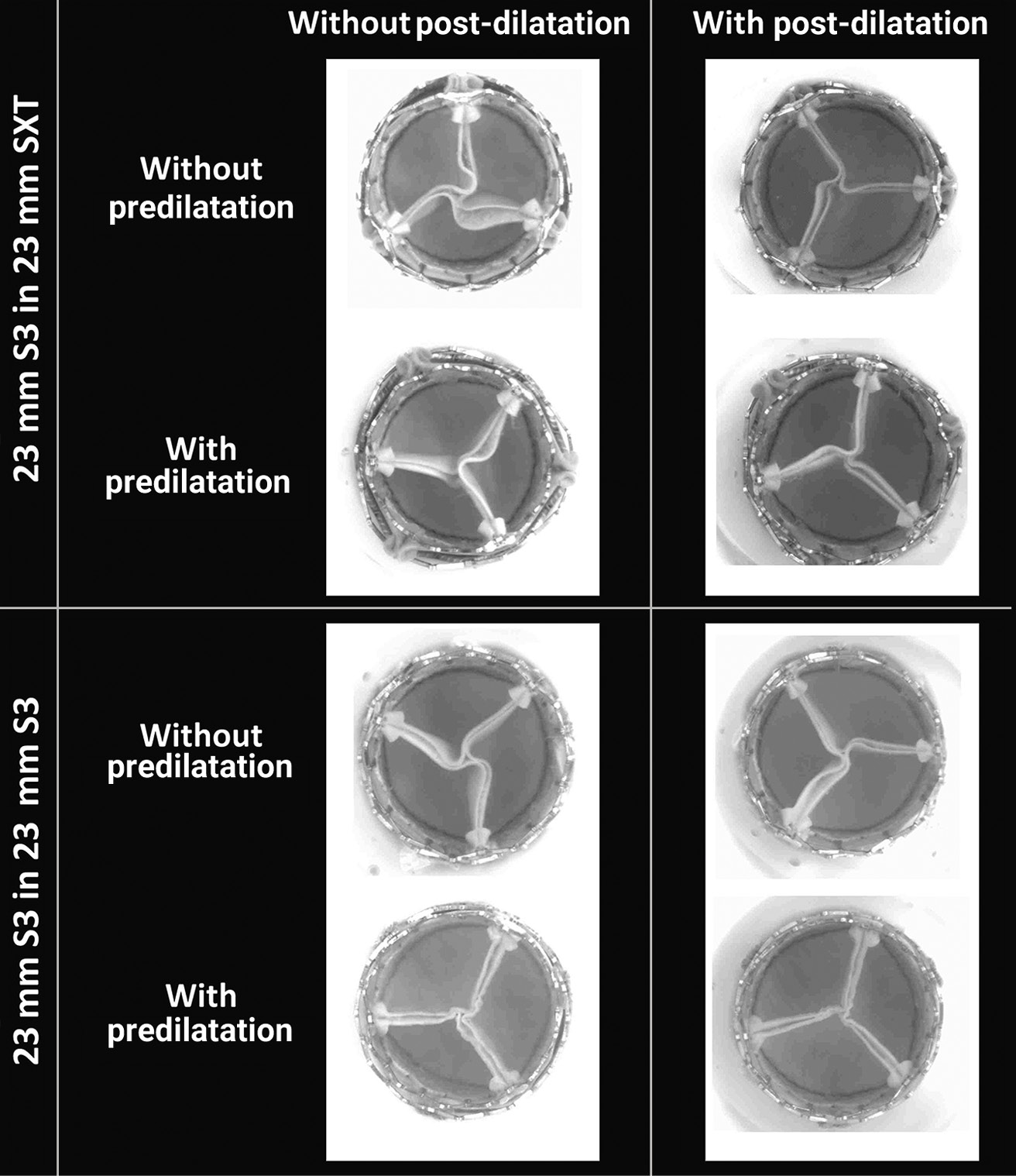
Figure 3. Images from the high-speed video showing the degree of pinwheeling of the SAPIEN XT (SXT) and SAPIEN 3 (S3) according to procedural scenario.
HYDRODYNAMIC PERFORMANCE
Results of the hydrodynamic testing, in terms of the MG and EOA, for the 8 samples are reported in Table 3. At baseline, all combinations resulted in an acceptable performance as per ISO standards.
Table 3. Hydrodynamic performances of the THV before and after post-dilatation
| Redo-TAVI configuration | MG (mmHg) | EOA (cm2) | |||
| Without post-dilatation | With post-dilatation | Without post-dilatation | With post-dilatation | ||
| S3 in SXT | Without predilatation | 9.8 ± 0.1 | 7.2 ± 0.5 | 2.0 ± 0.0 | 2.1 ± 0.0 |
| With predilatation | 8.0 ± 0.1 | 7.3 ± 0.1 | 2.1 ± 0.0 | 2.1 ± 0.1 | |
| S3 in S3 | Without predilatation | 7.5 ± 0.1 | 6.6 ± 0.3 | 2.3 ± 0.0 | 2.2 ± 0.1 |
| With predilatation | 9.7 ± 0.1 | 7.0 ± 0.1 | 2.0 ± 0.0 | 2.2 ± 0.0 | |
| EOA: effective orofice area; MG: mean gradient; S3: SAPIEN 3; SXT: SAPIEN XT; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve | |||||
Redo-TAVI with a 23 mm S3 in a 23 mm SXT
In the absence of predilatation, the MG and EOA of the S3 were 9.8±0.11 mmHg and 1.96±0.01 cm2, respectively. Following post-dilatation, minimal changes were observed (MG 7.2±0.50 mmHg, EOA 2.1±0.0 cm2).
When predilatation was performed before redo-TAVI, the MG and EOA of the S3 were 8.0±0.06 mmHg and 2.1±0.01 cm2, respectively, with almost no changes following post-dilatation (MG 7.3±0.10 mmHg, EOA 2.1±0.10 cm2).
Redo-TAVI with a 23 mm S3 in a 23 mm S3
In the absence of predilatation, the MG and EOA of the S3 were 7.5±0.09 mmHg and 2.3±0.01 cm2, respectively, with almost no difference following post-dilatation (MG 6.6±0.30 mmHg, EOA 2.2±0.1 cm2). When predilatation was performed before redo-TAVI, the MG and EOA of the S3 were 9.7±0.13 mmHg and 1.96±0.02 cm2, respectively. In this configuration, post-dilatation had the largest impact, since the MG decreased to 7.0±0.10 mmHg and the EOA increased to 2.2±0.0 cm2.
Discussion
We demonstrate the following when performing a SAPIEN in SAPIEN redo-TAVI: 1) In the absence of pre- and/or post-dilatation, the redo-THV is significantly underexpanded, and even with post-dilatation, the mid-portion of the THV remains constrained in most scenarios; 2) only the S3 in S3 redo-TAVI combination achieved uniform expansion when both pre- and post-dilatation were performed; and 3) the use of post-dilatation increases the dimensions of the index THV beyond its nominal size, which may impact procedural planning and risk prediction for annular injury.
In almost all scenarios (except for the S3 in S3 with pre- and post-dilatation), we observed some degree of underexpansion of the redo-THV mid-portion with some flaring at the inflow and outflow. The degree of diameter underexpansion was significant, with an expansion as low as 81% at the mid-portion. This underexpansion resulted in significant pinwheeling of the leaflets. This would likely be even worse in the case of a degenerated THV where the leaflets may be thickened and calcified. Non-uniform expansion can lead to impaired leaflet kinematics and increased pinwheeling which may impact long-term durability14. While long-term clinical data are currently lacking, it has been shown that asymmetric expansion is associated with HALT and increased 1-year mortality315. Moreover, some limited data have suggested a possible association between HALT and symptomatic valve deterioration16. These findings have implications for procedural planning and device selection. Procedural strategies that allow optimised expansion may aid both acute- and long-term valve performance. Hence, a self-expanding THV design with supra-annular leaflets where valve function and leaflet kinematics are less dependent on valve expansion may be considered in the case of a failed SAPIEN THV.
EFFECT OF PRE- AND/OR POST-DILATATION ON EXPANSION
Overall, pre- and/or post-dilatation improved expansion and reduced pinwheeling. It appears that the combination of both pre- and post-dilatation had an additive effect on the final expansion but that the magnitude of the effect varied depending on the THV combination. The S3 in S3 combination using pre- and post-dilatation was the only scenario which led to a full expansion of the S3 at the inflow, mid-portion and outflow. All the other scenarios led to residual underexpansion of the redo-THV. These results suggest that, even without considering patient specificity, each THV combination has unique features and that no class effect can be assumed in terms of procedural strategy. Of note, for the S3 in SXT combination, the overexpansion at the outflow of the S3 is likely related to the fact that this area did not have 2 layers of THV stent, since the S3 is taller than the SXT.
DIMENSIONS OF THE INDEX THV
The present work also offers valuable insights in the understanding of the index THV metamorphism in redo-TAVI. While the use of pre- and/or post-dilatation allows for optimised redo-THV expansion, it also expands the index THV beyond its nominal size. The magnitude of this effect was almost 3 mm at the outflow when the index THV was the SXT, while it was around 1 mm when the index THV was the S3. This difference is likely related to the thickness of the sutures at the level of the commissural post, which is more important for the SXT than for the S3. At the level of the inflow, likely to be situated closer to the annulus, this phenomenon was less marked, not exceeding 1 mm with either index THV. This element should be taken into consideration when planning redo-TAVI given the potential risk for annular damage depending on the extent of calcification and annular dimensions. Additionally, the overexpansion at the outflow might have an unpredictable impact on risk of coronary obstruction, decreasing the valve-to-coronary distance in patients with small sinuses of Valsalva and coronary ostia arising along the THV stent frame. Similarly to the magnitude of underexpansion of the redo-THV, the degree of overexpansion of the index THV is likely to be more important in the presence of leaflet thickening and/or the presence of pannus. Thus, the decision to pre- and/or postdilate the THV should be based on the patient’s annulus size/adverse root features. In cases where anatomical dimensions are borderline, it may be reasonable to avoid dilatation of the valve or to use a smaller balloon to mitigate the risk of the overexpansion of the index THV and damage to the anatomy. Alternatively, redo-TAVI with a self-expanding THV with a supra-annular leaflet position can be considered.
Limitations
The present work has some limitations inherent to bench testing. Indeed, bench testing may not entirely reflect how a THV will expand within a degenerated THV, as many factors such as leaflet calcification and native root anatomy are not represented in this study. Thus, it is likely that more underexpansion of the redo-THV would be observed and that, in the presence of thickened leaflets, the dimensions of the index THV could even increase beyond what was observed in the present study. Nevertheless, the present work suggests that pre- and post-dilatation can have an additive effect in some situations depending on the THV combination. Only one size of THV was tested and one sample was used for each combination. Furthermore, as would be done clinically, commissural alignment was random in the present study, and whether overlap of commissural tabs would increase the degree of underexpansion remains unknown. Finally, given the degree of underexpansion observed, a strategy where the second THV is downsized compared to the index THV warrants further study.
Conclusions
When performing redo-TAVI with an S3 inside an SXT or S3, only the S3 in S3 with the use of pre- and post-dilatation reached full redo-THV expansion. This underlines the importance of assessment of THV expansion with CT and the importance of considering pre- and/or post-dilatation at the time of redo-TAVI.
Further analyses of clinical series are needed to better understand procedural techniques that can lead to optimised expansion and improved long-term performance of THVs in the context of redo-TAVI.
Impact on daily practice
When performing redo-TAVI, there is a risk of underexpansion and a high residual gradient for the redo-THV. The impact of pre- and/or post-dilatation on expansion is unclear. In the present study, redo-TAVI with a SAPIEN 3 implanted within a SAPIEN XT or another SAPIEN 3 almost always resulted in underexpansion of the redo-THV despite the use of pre- and/or post-dilatation. Improved redo-THV expansion was accompanied by an expansion of the index THV beyond its nominal size. This underlines the importance of CT assessment of THV expansion and the role of pre-/post-dilatation. The long-term implications of THV underexpansion following redo-TAVI on performance and durability need to be determined.
Funding
D. Meier is supported by the Swiss National Science Foundation (grant P2LAP3_199561, Bern, Switzerland) and the SICPA foundation (Lausanne, Switzerland). G. Tzimas is supported by the Fondation Vaudoise de Cardiologie (Lausanne, Switzerland) and the SICPA foundation (Lausanne, Switzerland).
Conflict of interest statement
L. Sondergaard is the Chief Medical Officer and Divisional VP for Medical Affairs at Abbott Structural Heart; and has received consultant fees and/or institutional research grants from Abbott, Boston Scientific, Medtronic, and SMT. G. Lutter is a consultant to Edwards Lifesciences, Medtronic, and Abbott. T. Puehler is a consultant to Abbott. P. Blanke provides institutional CT core laboratory services to Edwards Lifesciences, Medtronic, Boston Scientific, Abbott Laboratories, PiCardia, and Neovasc, without direct personal reimbursements; and is a consultant to Edwards Lifesciences. J.G. Webb is a consultant to and has received research funding from Edwards Lifesciences, Abbott, and ViVitro Labs. J. Sathananthan is a consultant to Edwards Lifesciences, Medtronic, and Boston Scientific; and has received research funding from Edwards Lifesciences and Medtronic. D.A. Wood is a consultant to and has received research funding from Edwards Lifesciences and Abbott. S.L. Sellers is a consultant for Edwards Lifesciences and Medtronic. The other authors have no conflicts of interest to declare.