Abstract
Aims: The aim of this study was to investigate the prognostic value of fractional flow reserve (FFR) and a novel index (the D-index) of residual diffuse disease after intravascular ultrasound (IVUS)-guided second-generation drug-eluting stent (DES) implantation.
Methods and results: We evaluated 201 patients (201 lesions) who underwent IVUS-guided second-generation DES implantation in the left anterior descending artery with pre- and post-intervention physiological evaluations. Post-intervention hyperaemic pullback pressure recording was used to quantify residual diffuse disease using the novel D-index, defined as the difference between the distal stent and the far distal FFR values divided by distance. Clinical outcomes were assessed by vessel-oriented composite endpoints (VOCE) and major adverse cardiac events (MACE). The incremental discriminant and reclassification abilities of far distal FFR or D-index for VOCE and MACE were compared. Post intervention, far distal FFR and D-indices were significantly lower in vessels with VOCE. The optimal far distal FFR and D-index cut-off values for VOCE and MACE were 0.86 and 0.017 cm, respectively. Although both indices remained significant predictors of VOCE, only the D-index proved to be a significant predictor of MACE and significantly improved the incremental reclassification ability for MACE.
Conclusions: Residual diffuse disease assessed by the D-index after IVUS-guided second-generation DES implantation can help to predict both VOCE and MACE, while far distal FFR can help to predict VOCE specifically.
Introduction
Fractional flow reserve (FFR) has become the standard method to document ischaemia and guide revascularisation in the catheterisation laboratory for angiographically intermediate lesions. Furthermore, recent studies have reported an inverse and proportional relationship between post-intervention FFR values and the risk of subsequent adverse events, suggesting the potential of FFR to predict the residual risk not only of suboptimal stenting, but also of residual diffuse coronary artery disease after successful percutaneous coronary intervention (PCI) for epicardial lesions1,2,3.
The residual pressure gradient between the far distal coronary artery and the ostium of the target vessel after angiographically successful PCI may be related to suboptimal stenting and residual diffuse disease, which is not adequately detected by angiography4,5,6. Intravascular imaging has been reported to impact on optimal stenting and clinical outcomes after stenting7,8. However, studies on the prognostic influence of post-PCI FFR values after second-generation drug-eluting stent (DES) implantation with intravascular ultrasound (IVUS) assistance are rare. Even after stent optimisation by IVUS or optical coherence tomography (OCT) guidance, post-PCI FFR values remain <1.0, often attributable to invisible diffuse disease1,2,9. No studies have attempted to quantify residual diffuse disease after second-generation DES implantation with IVUS assistance or evaluate its prognostic value for subsequent events. Post-PCI pullback pressure recording under maximal hyperaemia may be used to quantify post-PCI residual diffuse disease.
Thus, the aim of this study was to investigate the prognostic value of post-PCI FFR and our novel D-index after IVUS-guided second-generation DES implantation. This index quantifies residual diffuse disease obtained by post-PCI hyperaemic pullback pressure recording and is based on post-PCI FFR.
Methods
PATIENT POPULATION
The prospective Tsuchiura Kyodo General Hospital registry database of cardiac catheterisation was retrospectively searched. We identified patients treated with elective and successful PCI with IVUS assistance who underwent pre- and post-PCI FFR with pullback pressure recording during maximal hyperaemia, coronary flow reserve (CFR), and index of microcirculatory resistance (IMR) measurements before and after PCI between June 2012 and June 2017. Patients were eligible if they satisfied the following criteria: physiological assessment by a pressure temperature sensor-tipped wire for a de novo single coronary lesion at the proximal or mid segment exhibiting intermediate stenosis (estimated as 30-80% diameter stenosis on angiogram by visual estimation) in the left anterior descending artery (LAD). The exclusion criteria are detailed in Supplementary Appendix 1. The final data set included 201 lesions from 201 patients (Figure 1).The study was conducted in accordance with the Declaration of Helsinki. The institutional ethics committee approved the study protocol and all patients provided written informed consent for enrolment in the institutional database for potential future investigations.
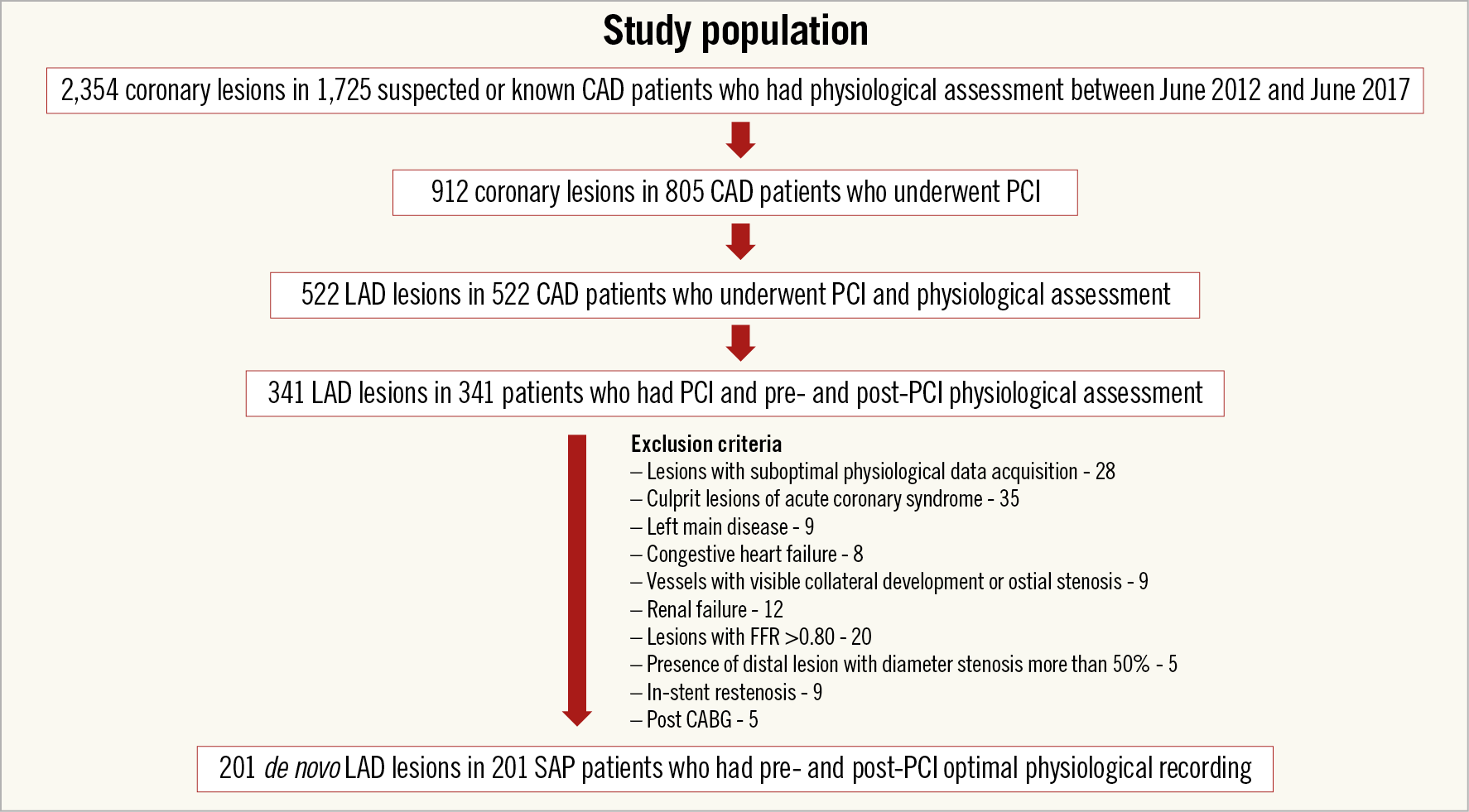
Figure 1. Study population. CABG: coronary artery bypass grafting surgery; CAD: coronary artery disease; FFR: fractional flow reserve; LAD: left anterior descending artery; PCI: percutaneous coronary intervention; SAP: stable angina pectoris
CATHETERISATION AND PCI PROCEDURE WITH IVUS GUIDANCE
All patients underwent second-generation coronary stent implantation with predilatation. When the operator confirmed acceptable results on the basis of angiographic and IVUS findings, post-PCI FFR measurement was performed and, in the presence of persistently ischaemic or suboptimal FFR results, a subsequent intervention was performed which included additional high-pressure post-dilation using a non-compliant balloon, additional stenting (in some cases of major edge dissection), or both at the operator’s discretion. The final decision for additional intervention was made by the operator, and some lesions with major dissection were left untreated. In about 22.4% of vessels, further intervention was performed in lesions which were not angiographically detected and was guided by pullback FFR analysis and IVUS observation after stenting. Although a total of 21 patients had multivessel disease at the time of the index PCI, they underwent complete revascularisation within three months from the index PCI and there were no patients who had residual functionally significant coronary stenosis.
The IVUS criterion for stent underexpansion was a post-procedural final minimum stent area of 5.0 mm²10,11. The MUSIC study criteria were also applied for optimal IVUS-guided stent implantation12.
INTRACORONARY PHYSIOLOGICAL INDICES
The FFR, mean hyperaemic transit time (Tmn), CFR, and IMR values were determined using the RadiAnalyzer™ Xpress instrument with the coronary PressureWire™ Certus™ (both St. Jude Medical, St. Paul, MN, USA), as described previously13,14,15. Hyperaemia was induced by an intravenous infusion of adenosine 5’-triphosphate (160 μg/kg/min). The distance from the ostium of the artery to the sensor position was determined by fastening a torque device to the advanced wire at the hub of the Y-connector. Then, the length of wire pulled back along the vessel was measured to position the sensor at each of the measuring positions from far distal to distal stent, proximal stent, and the ostium of the vessel, documenting pressures and FFR values at each position during hyperaemic manual pullback pressure recording at the speed of approximately 1 cm/sec. Pressure drift (PD) was determined when the pressure sensor reached the tip of the guiding catheter during hyperaemia. When mean Pd-Pa PD equal to or more than 4 mmHg at the tip of the guiding catheter during hyperaemia was confirmed, we reassessed physiologic data16.
Waveform tracings with phase adjustments meeting the following criteria were excluded from the analysis: 1) loss of pressure signal at any point during the measurement phase (apart from saline flush injection), 2) significant arrhythmia, including atrial fibrillation that might preclude appropriate waveform analysis, 3) inappropriate waveform quality, and 4) PD more than 4 mmHg.
NOVEL INDEX REPRESENTING RESIDUAL DIFFUSE DISEASE AFTER SUCCESSFUL PCI
The novel index for quantifying diffuse disease (the D-index) after stenting was defined as the delta FFR between the far distal and distal stent edge divided by the distance (far distal FFR minus stent distal FFR/distance/cm). By using hyperaemic pullback pressure recording, a sudden change in FFR value suggesting the presence of segmental stenosis was arbitrarily defined as equal to or more than 0.04/cm (defined as a D-index ≥0.04/cm). Lesions with a D-index ≥0.04/cm were excluded from the analysis. Representative angiographic findings, the corresponding post-PCI hyperaemic pullback pressure recordings and calculation of the D-index are shown in Figure 2.
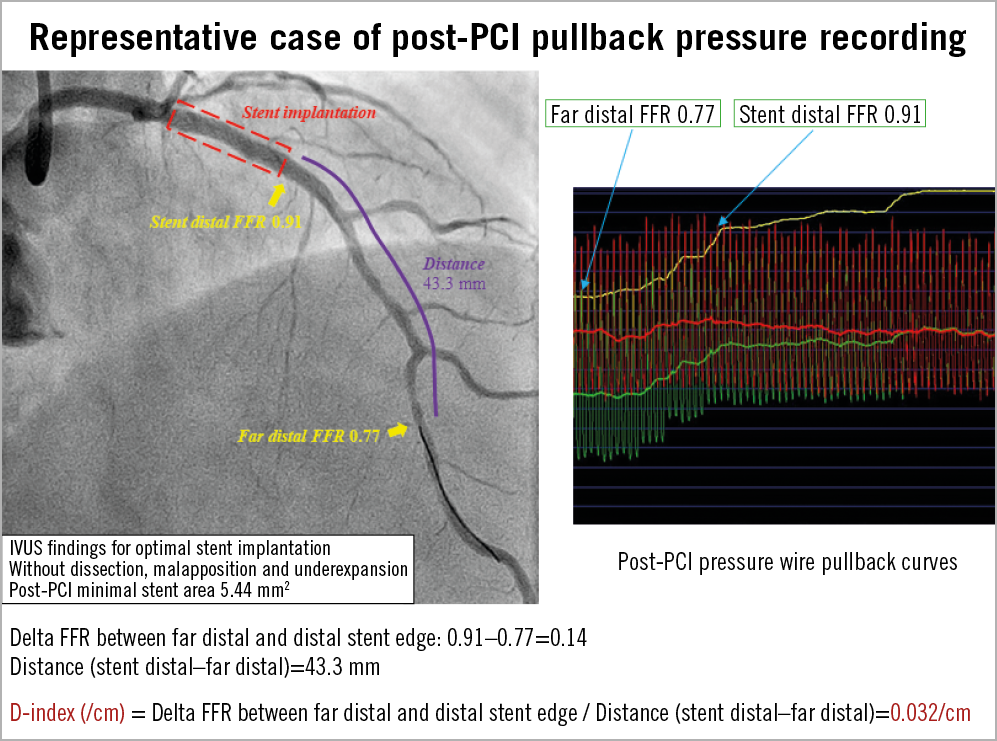
Figure 2. Representative post-PCI pullback pressure recordings and development of cardiac event. Representative case with stable angina pectoris after PCI. Hyperaemic pullback pressure recording documents gradual FFR improvement after IVUS-guided PCI. The D-index after stenting is calculated as delta FFR between the far distal and distal stent edge divided by the distance (/cm). FFR: fractional flow reserve; IVUS: intravascular ultrasound; PCI: percutaneous coronary intervention
The P-index was defined as a measure of difference in FFR values between guiding catheter tip and proximal stent edge divided by its distance. The S-index was defined as a measure of difference in FFR values between proximal and distal stent edges.
CLINICAL FOLLOW-UP
Vessel-oriented composite endpoints (VOCE) included cardiovascular death, vessel-related spontaneous myocardial infarction, and ischaemia-driven LAD revascularisation. In the study, VOCE were the cardiac events which occurred only in LAD lesions. Non-target VOCE included non-target vessel-related spontaneous myocardial infarction, and ischaemia-driven non-target vessel revascularisation. Although 21 patients had multivessel disease at the time of enrolment, they underwent complete revascularisation and no patients had residual significant coronary stenosis. One patient underwent revascularisation of in-stent restenosis of a non-target vessel and this was counted as non-target VOCE. The remaining 14 non-target VOCE were considered to be progression of native coronary lesions. In this study, non-target VOCE were nine in right coronary artery lesions, and six in left circumflex artery lesions. Major adverse cardiac events (MACE) were a composite of VOCE and non-target VOCE.
STATISTICAL ANALYSIS
Data were analysed on a per-lesion basis (one LAD lesion per patient). The statistical analysis was performed using SPSS, Version 23.0 (IBM Corp., Armonk, NY, USA). Categorical data were expressed as numbers and percentages and compared by χ2 or Fisher’s exact tests as appropriate. Continuous biochemical or physiological data were expressed as median (interquartile range [IQR]) and analysed using the Mann-Whitney test and analysis of variance for variables with non-normal distribution and normal distribution, respectively. Correlations between the two parameters were evaluated using a linear regression analysis. Receiver operating curves were analysed to assess the best cut-off values of post-PCI physiological indices and clinical characteristics to predict the occurrence of VOCE, non-target VOCE, and MACE. The optimal cut-off was calculated using the Youden index. Event rates over time were estimated using the Kaplan-Meier method, and linear trends were tested with log-rank tests. Since two subjects experienced both VOCE and non-target VOCE, the first event that occurred was counted in the survival analysis using Kaplan-Meier estimates for MACE in 27 patients. A Cox proportional hazards regression model was used to identify independent predictors of VOCE and MACE. The covariates used in multivariate analysis were selected using the criterion of p<0.10 in the univariate analysis. A collinearity index was used for checking linear combinations among covariates, and the Akaike information criterion for avoiding overfitting. A two-sided p<0.05 was considered statistically significant. Three prediction models were constructed to determine the incremental discriminatory and reclassification performance of the far distal FFR and the D-index for VOCE and MACE. As a baseline, clinical model 1 was derived from age, sex, hypertension, diabetes mellitus, hyperlipidaemia, the use of statins, and chronic kidney disease. Clinical model 2 was derived from clinical model 1 + far distal FFR <0.86. As the last model (clinical model 3) including the novel index representing residual diffuse disease, clinical model 1 + the D-index ≥0.017/cm was used. The discrimination and reclassification ability of model 3 was compared using relative integrated discrimination improvement (IDI) and net reclassification index (NRI).
Results
BASELINE PATIENT CHARACTERISTICS AND PROCEDURAL FINDINGS
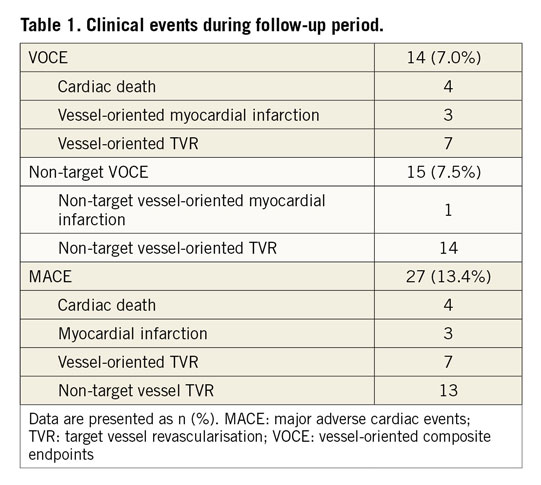
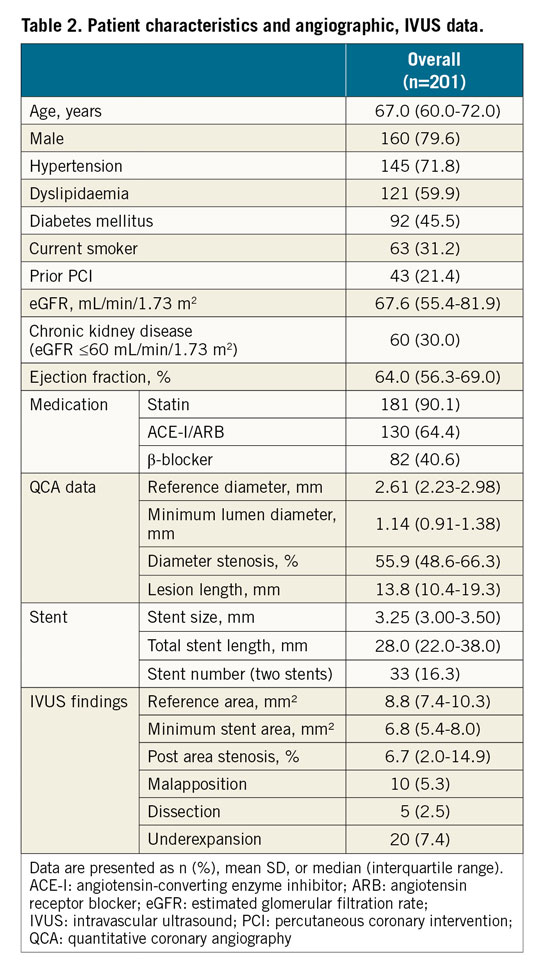
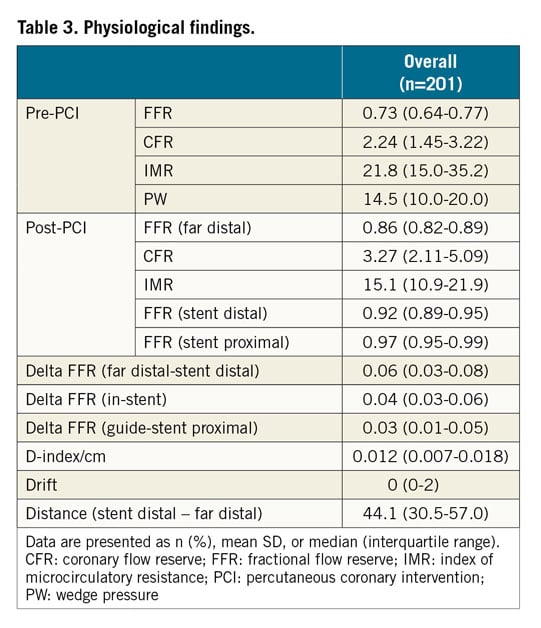
During a median follow-up of 24 months (14-48), VOCE occurred in 14 (7.0%) patients and non-target VOCE was observed in 15 (7.5%) territories in 15 patients. Clinical outcomes are summarised in Table 1. Demographics, angiographic and procedural characteristics are shown in Table 2. There was no statistically significant difference in IVUS findings in the two groups with or without VOCE (Supplementary Table 1). The median value of pre-PCI FFR measurements was 0.73 (0.64-0.77), and the post-PCI median value of FFR measurements was 0.86 (0.82-0.89) at the far distal position (Table 3). Post-PCI far distal FFR values were significantly lower in territories with VOCE than in those without, while there was no significant difference in FFR values in the proximal stent and distal stent positions in the two groups. The distance between post-PCI distal stent and far distal FFR measurement positions was 44.1 mm (30.5-57.0). The prevalence of adequate expansion according to the MUSIC criteria was also not significantly different between patients with and without VOCE (Supplementary Table 1). D-indices were widely distributed (median, 0.012; range, 0.007-0.018) and significantly greater in vessels with VOCE than in those without, and in vessels with MACE than in those without (Supplementary Table 2).
PREDICTIVE VALUES OF FFR AND THE D-INDEX FOR CLINICAL OUTCOMES
Receiver operating characteristic (ROC) curve analysis revealed that the best far distal FFR cut-off value for predicting VOCE and MACE was 0.86 for both. At a median follow-up of 24 months (14-48 months), VOCE-free survival was significantly worse in patients with far distal FFR values <0.86 (log-rank p=0.002) (Figure 3A), whereas far distal FFR <0.86 provided no significant prognostic information for MACE (log-rank p=0.084) (Figure 3B). ROC curve analysis also showed that the optimal D-index cut-off value for predicting VOCE and MACE was 0.017/cm. A D-index of ≥0.017/cm effectively discriminated VOCE (log-rank p=0.008) (Figure 4A). The best D-index cut-off value for predicting MACE (VOCE and non-target VOCE) was similar at 0.017/cm (log-rank p<0.001) (Figure 4B). This value remained as a significant predictor of non-target VOCE (log-rank p=0.046) (Figure 5A). On the other hand, far distal FFR provided no significant prognostic information for non-target VOCE (log-rank p=0.50) (Figure 5B). A Cox proportional hazards analysis revealed that a D-index of ≥0.017/cm was a significant predictor of VOCE (Supplementary Table 3). The P-index and S-index were both not significantly different between patients with and without VOCE or MACE (Supplementary Table 2). Multivariable Cox proportional hazards analyses revealed that chronic kidney disease and a D-index of ≥0.017/cm were independent predictors of MACE (Table 4).
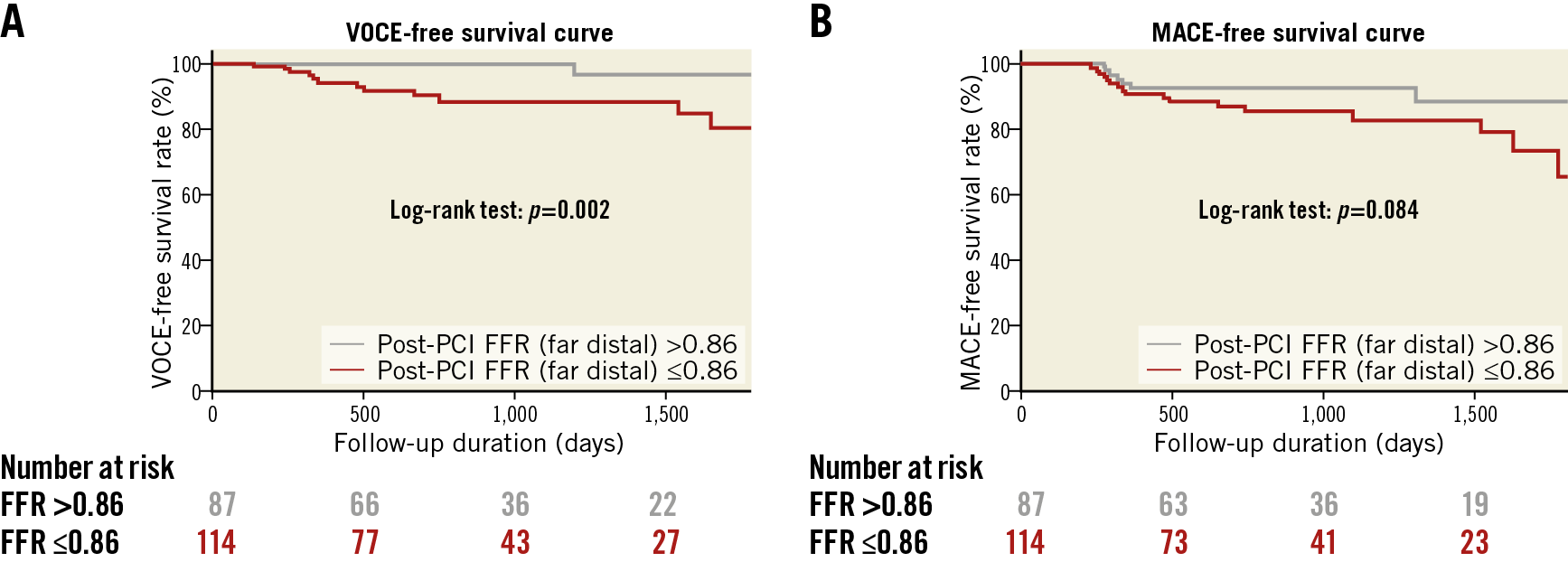
Figure 3. Freedom from VOCE and MACE according to post-PCI far distal FFR. Kaplan-Meier curve showing significantly higher survival free from VOCE (A) and MACE (B) in the patients with far distal FFR of ≥0.86 compared to the far distal FFR <0.86 group. FFR: fractional flow reserve; MACE: major adverse cardiac events; PCI: percutaneous coronary intervention; VOCE: vessel-oriented composite endpoints
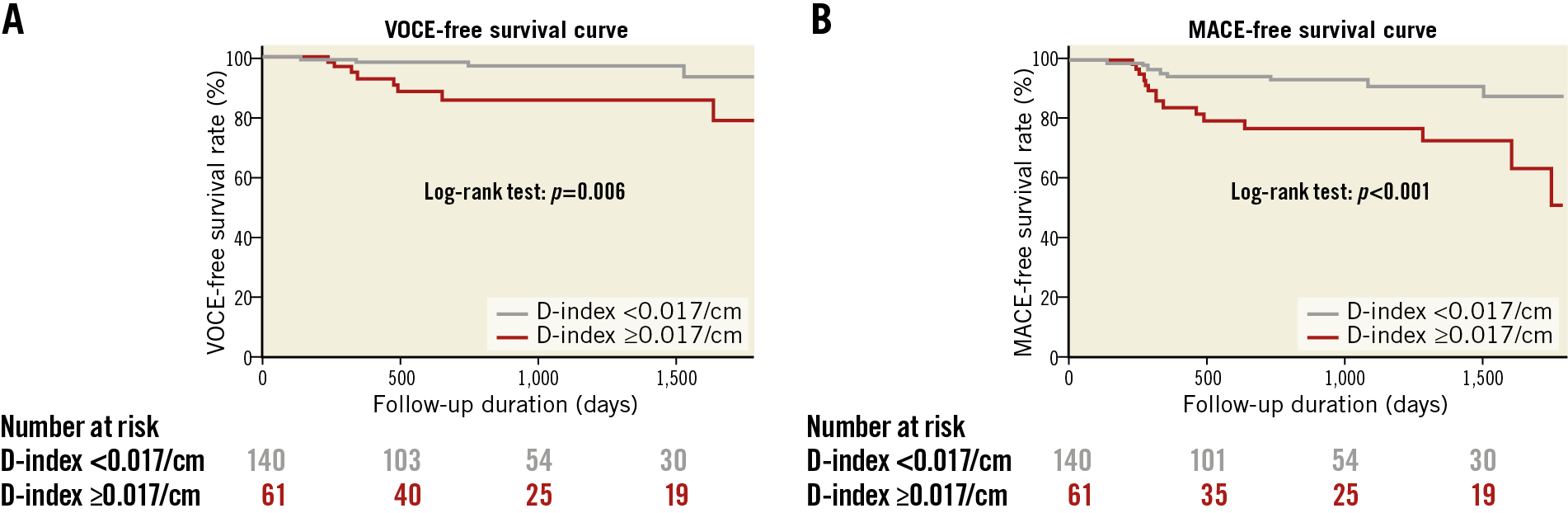
Figure 4. Freedom from VOCE and MACE according to the D-index. Kaplan-Meier curve showing significantly higher survival free from VOCE (A) and MACE (B) in patients with a D-index <0.017/cm compared to patients with a D-index ≥0.017/cm. MACE: major adverse cardiac events; VOCE: vessel-oriented composite endpoints
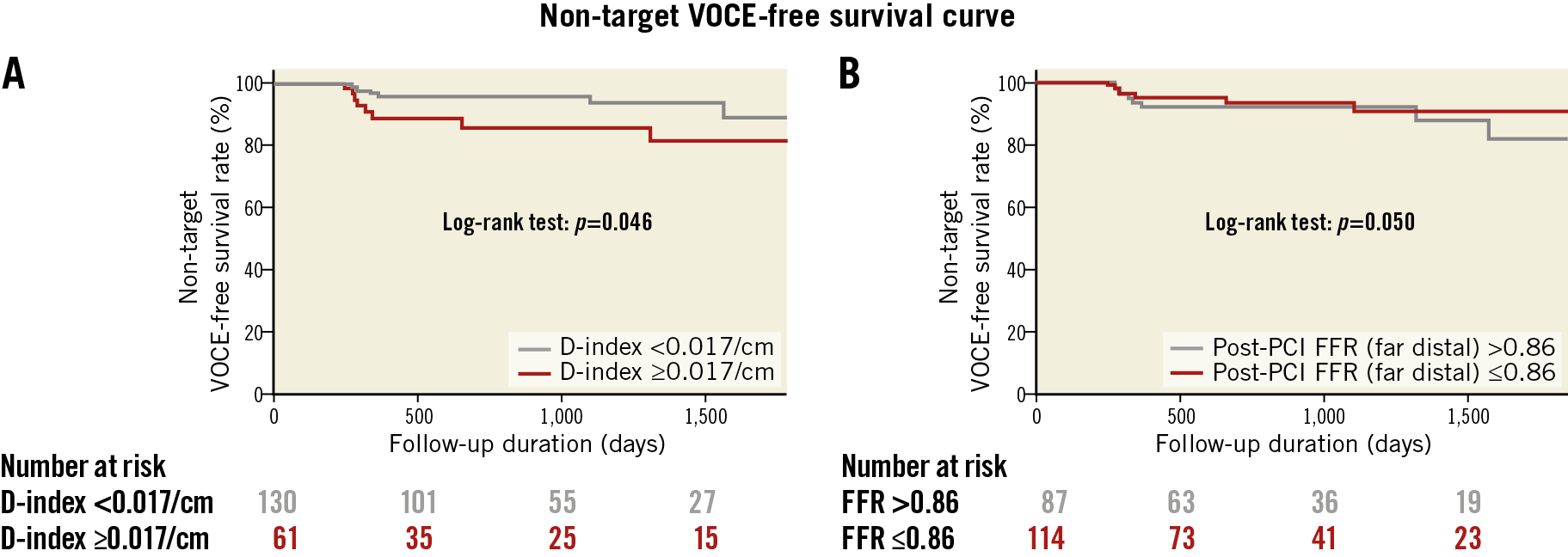
Figure 5. Freedom from non-target VOCE. A) Kaplan-Meier curve showing significantly higher VOCE-free survival in the patients with a D-index <0.017/cm compared to patients with a D-index ≥0.017/cm. B) Kaplan-Meier curve showing no difference in the patients with a post-PCI FFR ≥0.86 compared to patients with a post-PCI FFR <0.86. FFR: fractional flow reserve; PCI: percutaneous coronary intervention; VOCE: vessel-oriented composite endpoints
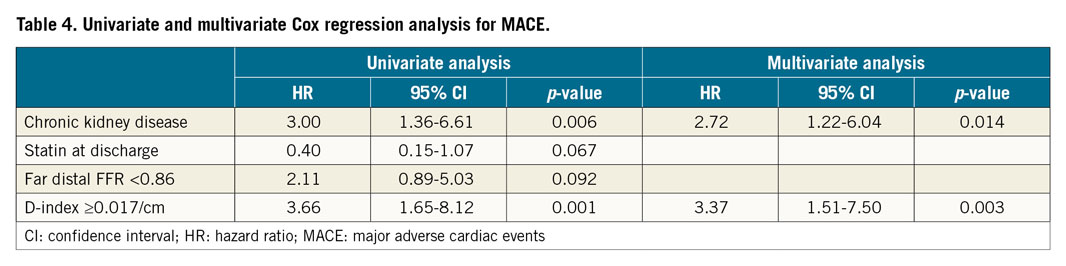
Figure 6 presents the NRI and IDI values for the three models. Furthermore, model 3 showed significant incremental reclassification ability for VOCE (NRI: 0.730, p=0.006; IDI: 0.067, p=0.029) and MACE (NRI: 0.502, p=0.014; IDI: 0.045, p=0.030) compared with model 1, whereas model 2 showed incremental reclassification ability only for VOCE.
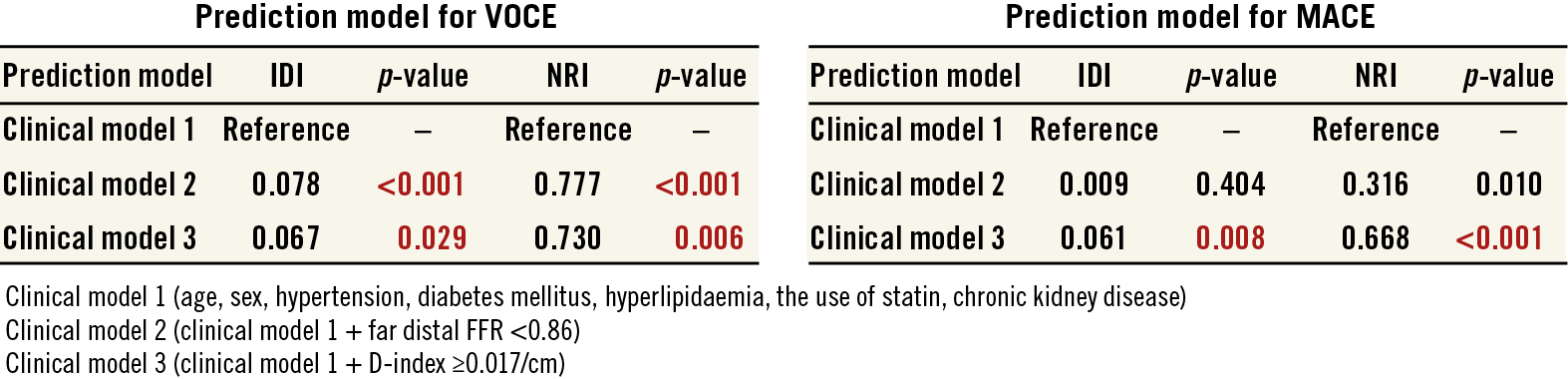
Figure 6. Comparison of discriminant and reclassification ability of predictive models to determine incremental discriminatory and reclassification capacities of far distal FFR and D-index for cardiac events. FFR: fractional flow reserve; IDI: relative integrated discrimination improvement; MACE: major adverse cardiac events; NRI: net reclassification index; VOCE: vessel-oriented composite endpoints
In comparison with the pressure wire location of 44 mm (median) from the distal stent edge, post-PCI IVUS imaging was performed from 15 mm (median) of the distal stent edge to 7 mm (median) of the proximal stent edge. The results from these limited IVUS data showed no significant difference between vessels with VOCE and those without VOCE (Supplementary Table 4).
Discussion
This is the first study demonstrating significant prognostic value of post-PCI far distal FFR values and the novel physio-logical index quantifying residual diffuse disease for patients after successful second-generation DES implantation with IVUS guidance. The present study provides the following important findings: 1) a novel index (the D-index) quantifying residual diffuse disease was introduced and calculated as the difference in FFR values divided by the distance between distal stent edge and far distal FFR measurement position, 2) the D-index was widely distributed and demonstrated a significant association not only with VOCE, but also with non-target vessel VOCE, whereas far distal FFR showed no prognostic value for non-target VOCE, 3) a D-index of more than 0.017/cm was significantly associated with MACE, including VOCE and non-target VOCE (log-rank p<0.001), 4) the integration of residual diffuse disease assessment after PCI (D-index) improved risk stratification and had incremental prognostic value on coronary risk factors for VOCE and MACE (Figure 6).
A residual pressure gradient or low FFR after angiographically successful coronary stenting can be caused by several mechanisms, including the presence of an unmasked lesion other than an initially stented lesion, pressure sensor drift, residual diffuse disease, and suboptimal stenting17. Intracoronary imaging, such as IVUS and OCT, may help to identify suboptimal stenting and improve prognosis, particularly when the stented segment is the primary cause of low post-PCI FFR values4,5,18. A pullback pressure recording under maximal hyperaemia may help to identify the primary mechanism3,9. Currently, final PCI results are mostly evaluated by angiography; however, residual disease caused by diffusely distributed atherosclerotic burden may not be adequately revealed with angiography. Diffuse disease is commonly associated with epicardial focal stenosis in patients with coronary heart disease, and these have been reported to be significant risk factors for subsequent cardiac events2,19. PCI can modify and reduce epicardial focal stenosis, but residual diffuse disease may not be cured by PCI. Our results suggest that residual severe diffuse disease after PCI may limit or override the benefit of revascularisation and influence outcomes, since the D-index independently provided significant prognostic information for non-target vessel VOCE, while far distal FFR did not.
THE ASSOCIATION BETWEEN THE D-INDEX AND THE POST-PCI MEASUREMENT POSITION OF FFR
In our study, post-PCI far distal FFR values demonstrated prognostic efficacy: the best cut-off FFR value to predict VOCE was 0.86, which was similar to or lower than previously reported cut-off values3,4,20,21. This is probably due to the differences in study population, drugs and administering methods for inducing hyperaemia, subtended cardiac mass and the location of the pressure wire. In particular, the location of the FFR measurement position is important since a far distally located wire gives lower FFR values. In the present study, the starting position of post-PCI pullback pressure recordings was 44.1 mm (30.1-57.0) from the distal stent edge. This distance might have contributed to the clinical significance not only of far distal FFR values, but also of D-indices for quantifying residual diffuse disease, and helps to demonstrate the prognostic information of this index not only for VOCE but also for MACE, potentially by representing systemic severe atherosclerotic burden after PCI.
POTENTIAL CLINICAL IMPLICATION
Pre-PCI FFR values or hyperaemic pullback pressure documentation may not accurately discriminate focal stenosis and co-existing diffuse disease. The relative severity of the epicardial lesion and residual diffuse disease are not easily discriminated, particularly when severe focal lesion and diffuse disease co-exist. PCI would reduce anatomical focal stenosis and potentially increase coronary flow, resulting in an enhanced pressure gradient caused by residual diffuse disease between the stent distal and far distal positions. PCI for the epicardial focal lesion may not help to reduce adverse events in the presence of severe diffuse coronary artery disease. The impact of microvascular dysfunction on diffuse disease is detailed in Supplementary Appendix 2.
Study limitations
The results of the present study should be interpreted bearing in mind several important limitations. First, this study included a relatively small number of subjects from a single centre, which may not allow extensive subgroup analysis or more reliable multivariable analyses. Second, rigorous exclusion criteria limited the number of study patients and the analysis included only LAD lesions. This may have resulted in some level of selection bias, while the present analysis might have excluded the physiological difference dependent on lesion location. Third, decision making and subsequent interventions during PCI were based on the operator’s discretion without a prospectively defined procedure algorithm.
Conclusions
The post-PCI far distal FFR value was associated with VOCE after second-generation DES stenting with IVUS guidance, independent of the presence or absence of suboptimal stenting. The severity of residual diffuse disease after successful PCI as measured by the novel D-index was associated with poor prognoses, including VOCE and non-target VOCE. The integration of D-index assessment may improve the identification of MACE.
|
Impact on daily practice Post-PCI far distal FFR values were associated with VOCE after second-generation DES stenting with IVUS guidance. A novel D-index representing the severity of residual diffuse disease after PCI may help to identify high-risk patients for subsequent adverse cardiac events, not only for VOCE, but also for MACE. |
Conflict of interest statement
The authors have no conflicts of interest to declare.