
Introduction
Contained ruptures of the aortic annulus (CR) have been diagnosed as an incidental finding on computed tomography angiography (CTA) performed after TAVI with an incidence of up to 5%1. Information on outcomes in patients with CR is limited2-6. Therefore, the aim of the present study was to evaluate long-term outcomes in patients with CR from a large European multicentre cohort with systematic post-TAVI CTA.
Methods
We report on 12 patients (out of a total of 1,030) who underwent post-TAVI CTA between July 2009 and July 2015 at three centres in Denmark and Germany. Data collection was performed via case report forms, and a final interview (by phone or via mail) was conducted in all patients between May and November 2016.
Results
The median interval from TAVI to diagnosis was 16±15 days. Patient characteristics are summarised in Table 1. All patients had received a balloon-expandable valve (SAPIEN XT or SAPIEN 3; Edwards Lifesciences, Irvine, CA, USA). Mean degree of oversizing was 26.7±10.5%. In three of the 12 patients, periprocedural transoesophageal echocardiography (TEE) revealed findings suggestive of aortic dissection, an aortic intramural haematoma, and/or a pericardial effusion. In the remaining nine patients, periprocedural echocardiographic monitoring, including TEE in seven patients, was unremarkable and the rupture was detected incidentally on post-TAVI CTA. In nine cases (75%), the contained rupture was found adjacent to the left coronary cusp, whereas the bulk of calcification was found next to the non-coronary cusp (Table 1). At the time of diagnosis, none of the patients was symptomatic, and no specific treatment related to the CR was initiated. During a median follow-up of 2.5±1.5 years, none of the patients developed symptoms or died from CR-related causes. In five patients, follow-up-CTA was performed after 287±218 days, three with stable findings and two with no longer detectable ruptures (Figure 1).
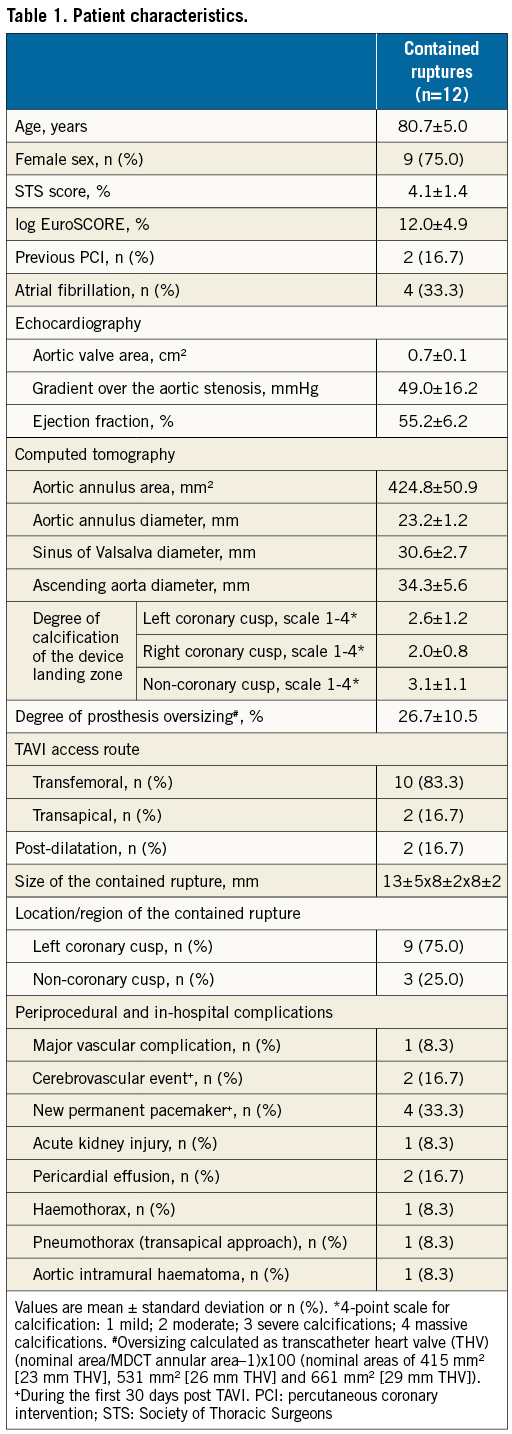
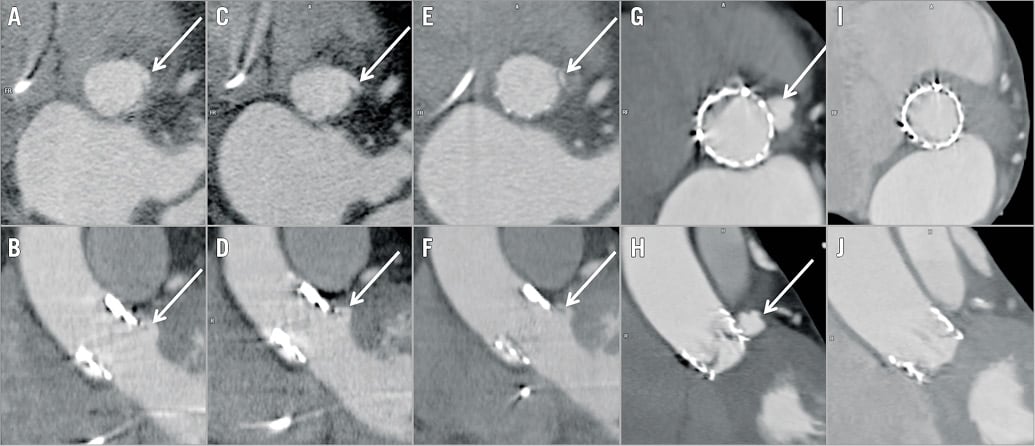
Figure 1. Typical CTA findings of contained ruptures of the aortic annulus post TAVI (arrow in A-H). The first case represents an 80-year-old female with a contained rupture diagnosed eight days post TAVI (A & B). Findings on CTA are unchanged after one (C & D) and three years (E & F). The second case demonstrates a contained rupture in a 77-year-old female diagnosed 15 days post TAVI (G & H) with complete remission in a follow-up CTA performed eight months later (I & J).
Discussion
To the best of our knowledge, this is the first study to investigate the long-term follow-up of patients with contained rupture of the aortic annulus after TAVI, documenting a benign course over a mean follow-up period of 2.5±1.5 years. In none of our patients was a specific treatment necessary, and all remained asymptomatic during the follow-up period. This is in line with prior short-term follow-up studies, which demonstrated unchanged follow-up CTA and favourable outcomes up to six months1-4.
Limitations
Due to the clinical characteristics of our patient cohort, we achieved a post-TAVI CTA rate of 69%. Therefore, a number of contained ruptures may have been missed and a higher incidence of this condition cannot be excluded. Although our observations are based on a large cohort undergoing TAVI, the number of patients with contained ruptures is limited as is the duration of follow-up.
Conclusions
The data presented suggest that previously reported favourable short-term outcomes1-4 in patients with CR extend to long-term follow-up, supporting a conservative approach in these patients.
| Impact on daily practice A contained rupture after TAVI represents a rare, predominantly incidental finding on post-TAVI CTA. No adverse events related to the contained rupture were reported during long-term follow-up, supporting a watch-and-wait strategy in these patients. |
Conflict of interest statement
F-J. Neumann reports receiving grants and non-financial support from Edwards Lifesciences. G. Pache is a consultant for Edwards Lifesiences. P. Blanke provides core laboratory services for Edwards Lifesciences. Medtronic, Neovasc, Tedyne and Aegis, for which he does not receive direct financial compensation. He is a consultant to Edwards Lifesciences, Neovasc, Tendyne, Circle Cardiovascuar Imaging. The other authors have no conflicts of interest to declare.

