Introduction
The Heart Team (HT) is essential when deciding upon the intervention in patients with valvular heart disease (VHD). There is evidence that patients express clear preferences for being involved in medical decision making. Unfortunately, the information patients can provide is overall underutilised1.
HT recommendations should be discussed with the patient, who can then make an informed decision taking into account his/her values and expectations in order to optimise patient-centred outcomes2.
Transcatheter aortic valve implantation (TAVI) will be used as an illustration in this editorial, because of the large clinical experience in this technique throughout the spectrum of surgical risk.
GENERAL PRINCIPLES
Patient-centred care requires that both the patient and the HT share information and work towards a consensus on decision making.
The choice between TAVI and surgical aortic valve replacement (SAVR) or medical therapy involves knowledge of the disease, making trade-offs between invasiveness of the procedure, immediate risks and benefits, and the balance between estimated life expectancy and prosthetic valve durability. This may be challenging given the remaining uncertainties in current data.
The validity of the patients’ preferences assumes the absence of significant cognitive impairment and the voluntary participation of the patient, because the patients’ wishes may differ from those estimated by their families or physicians. The former condition may justify the expertise of a geriatrician.
Finally, the burden of comorbidity is important. Patients should be made aware that symptoms that are not due to VHD will not improve after TAVI.
Besides patients and family, the “global network of care” must be involved in the process, including the HT members, the attending cardiologist, the general practitioner (GP) and, importantly, the nurses who deal closely with the patients.
Key factors are communication, the provider-patient relationship and trust, in which patients are empowered to question therapeutic options.
The assessment of patients’ preferences is a long and difficult process which requires time and patience.
PATIENTS’ PREFERENCES
Patients’ preferences for their involvement in decision making can be divided into a preference for information about the disease and treatment, and the desire to participate in the decision-making process. Information preferences are reported to be high in most patients, while there is variability regarding participation preferences (Figure 1).
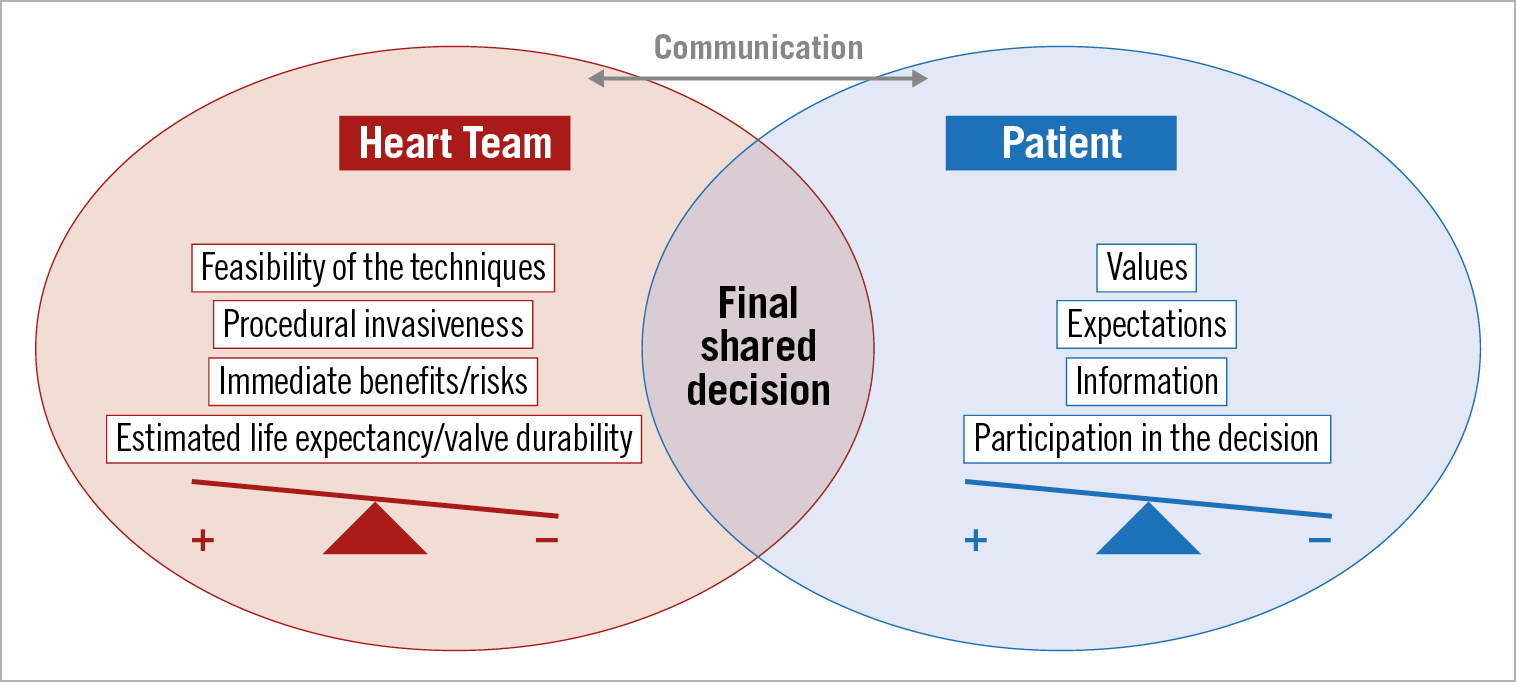
Figure 1. Integrating patient preference into the Heart Team decision.
INFORMATION PREFERENCES
A normative “one size fits all” approach is not the best recipe to meet patients’ preferences, which are very heterogeneous. This heterogeneity is due to differences in: i) education, which is “culturally sensitive” between specific regions, ii) awareness about VHD and its treatment in the general population, iii) the influence of the physician, since “paternalistic physicians” tend to expect a more passive role from the patients, and iv) socio-economic factors. Appropriate stewardship of economic resources is an important responsibility of the HT. Another difference is v) clinical conditions; even in “high-income countries” the most deprived patients receive less care. Age is a key factor today in the TAVI field. Elderly patients prefer symptomatic benefit over increased survival. Severity of heart failure symptoms influences patients’ willingness to accept risks.
PARTICIPATION IN THE DECISION
A few studies have shown that patients’ preferences may lead the decision-making process in as many as 40% of cases3.
Within the elderly population currently referred for TAVI, a large proportion of patients prefers TAVI over SAVR because they place great value on the benefits of TAVI and are willing to tolerate uncertainties about durability4.
The agreement between the proposal from the HT and patients’ preferences may be easy in younger patients at low risk for surgery who accept surgery, elderly patients who are good candidates for TAVI and prefer TAVI and, finally, those for whom TAVI is obviously futile.
In other cases, reaching a consensus may be difficult or even impossible. The decision is most challenging in patients for whom there are uncertainties about evidence, but this is also the situation when patients’ engagement is needed the most. This scenario may happen in two sets of patients. It may occur in younger patients at low risk for surgery, without adverse conditions for TAVI, who do not want to be operated, accepting the risk of reintervention and the more frequent need for pacemaker implantation, given the lower initial risks and a more rapid return to full activity. This scenario is likely to be increasingly frequent and requires in-depth discussion during which several members of the HT share information with the patient5. It may also occur in patients at high/prohibitive risk where there is no firm line drawn between those who should or should not receive the treatment. Ascertaining benefit versus futility in individual patients is a difficult and multifaceted problem requiring collective judgement6.
The divergence of opinions might be bidirectional.
1) Physicians report patients’ preference as the most common reason to select medical management, despite the opinion of the HT. In up to 40% of cases, the HT recommends an intervention which is refused by the patient3,7. Interestingly, it has been shown that patients receiving medical treatment may complain afterwards about receiving insufficient information concerning intervention or surgery – less engagement by their physicians in the decision – and are more prone to believe that the final decision was not the best one. For these patients, the consensus in favour of intervention should be eagerly sought by the HT if TAVI is estimated at an acceptable risk level and an important benefit is expected.
2) Less frequently, patients may want an intervention which is refused by the HT. In this case, a cautious and comprehensive discussion concerning the patient and family expectations would be needed. Many of these patients will benefit from palliative care consultation.
In such patients, the evaluation of futility could be a dynamic process. There are ongoing trials investigating the effect of prehabilitation strategies (TAVR frailty; TAVR prehab).
In both scenarios, the lack of consensus raises an ethical question about the right of the HT to refuse a treatment modality, if a patient is adequately informed about treatment options and outcomes.
FUTURE PERSPECTIVES
Patient awareness of valvular heart disease is far from being satisfactory and is only slowly improving over time8. Awareness campaigns on VHD, such as European Heart Valve Disease Awareness initiatives ([email protected]; https://heartvalvecouncil.org) or the Valve for Life initiative by the EAPCI9, are helpful to raise awareness of aortic stenosis.
HT members must understand better the importance of patient-centred outcomes and improve their knowledge and skills in shared decision making. Communication skills are an important aspect (including empathy, language, use of educational videos) during in-hospital and after discharge consultations. Tools have been developed to enhance active participation in informed shared decision making (https://valveadvice.org/about-us; https://www.cardiosmart.org/TAVR DecisonAids)10.
Further research is needed to identify and weigh the importance of patient preference and to evaluate the effects of educational interventions.
Conclusion
“Incorporating patients’ preferences into the HT equation” is important in the TAVI era. This aspect significantly complements the individualised evaluation of the clinical, anatomical, and procedural aspects. Such a patient-centred approach is likely to enhance the active participation of patients in decisions concerning their health and improve the outcomes.
Conflict of interest statement
A. Vahanian is a consultant for CardioValve. M. Urena has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.