Drug-coated balloon (DCB) angioplasty offers a novel strategy for the treatment of coronary artery disease. It yields non-inferior clinical outcomes compared with drug-eluting stent (DES) implantation in patients with in-stent restenosis and de novo small vessel disease1. When an acceptable angiographic result is achieved after lesion preparation in de novo lesions, DCB angioplasty allows delivery of the antiproliferative drug to the vessel wall while avoiding implantation of permanent metallic struts and their long-term consequences2. Evidence regarding DCB angioplasty in de novo lesions of large coronary vessels is scant.
The observational, retrospective DCB 3.0 cohort study included a total of 93 consecutive patients with coronary artery disease treated with DCB angioplasty for de novo lesions (n=100) on large coronary vessels at 2 centres in Italy (EMO-GVM Columbus and IRCCS Humanitas Research Hospital) between July 2020 and June 2022. The study was exempted from ethics committee approval, given its retrospective nature. Inclusion criteria were 1) presence of a de novo lesion in a vessel >3.0 mm in diameter and 2) performance of angioplasty with a DCB 3.0 mm or more in diameter, irrespective of concomitant DES implantation. After predilation, stenting was deferred in dissections classified as National Heart, Lung and Blood Institute (NHLBI) type A or B, provided there was Thrombolysis In Myocardial Infarction (TIMI) flow grade 3. In cases with evidence of flow-limiting dissection (TIMI flow grade <3) after either predilation or DCB angioplasty, percutaneous coronary intervention (PCI) with stent insertion was recommended. NHLBI dissections type C-E, if not flow-limiting, underwent functional evaluation according to the ratio of distal coronary pressure to aortic pressure (Pd/Pa)3.
The mean age of enrolled patients was 68±11 years old (89% male). One out of four patients were diabetic, the mean Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score was 22, and clinical indication for intervention was chronic coronary syndrome in 83% of cases. Out of 100 lesions, about half (48%) occurred on the left anterior descending artery and a quarter on the left circumflex artery. A single long lesion was treated and enrolled for the majority of patients (92.5%). Lesions were American College of Cardiology/American Heart Association class B2/C in 77% of cases, 1 out of 3 were bifurcations and 1/10 were severely calcified. The mean lesion length was 45±26 mm and treated vessels had a diameter of 3.2±0.3 mm. A DCB angioplasty alone intention-to-treat (ITT) strategy was implemented in 70% (n=70) of lesions, with 6% (n=6) of cases undergoing bailout DES implantation (Central illustration). A hybrid DCB+DES strategy was performed in the remaining lesions (30%), which tended to be longer (59.9±22.5 mm vs 38.1±25.8 mm; p<0.001). Lesion preparation included balloon predilation (diameter 3.1±0.4 mm, pressure 18±4 atm) in 90.0% of cases and cutting balloon inflation in 9.0%. Utilisation of intravascular lithotripsy (6.0%) and rotational atherectomy (4.0%) was rare. Intravascular imaging, most often intravascular ultrasound, was adopted in 40% of cases.
The majority of DCB employed were sirolimus-coated (77%, which comprised 52% MagicTouch [Concept Medical] and 25% SELUTION [Med Alliance]), while paclitaxel-coated balloons included IN.PACT Admiral/Prevail (Medtronic) in 18.0% of cases and RESTORE (Cardionovum) in 5.0%. The mean number of DCB per lesion was 1.4±0.8, and balloons adopted were 3.1±0.3 mm in diameter, 35±22 mm in length and inflated at 12±3 atm. The incidence of angiographically evident coronary artery dissection was 52% (n=52) (Central illustration), two being NHLBI type C-E. The number of balloons used was higher (1.6±0.9 vs 1.1±0.2; p<0.001) and they had an overall longer length (38.1±25.8 mm vs 28.1±12.1 mm; p=0.051) in the DCB alone ITT group versus the hybrid DCB+DES group. Among lesions treated with hybrid DCB+DES, 1.3±0.5 DES were implanted per lesion, with a diameter of 3.4 mm and a length of 26 mm. The overall median follow-up for the cohort was 350 (interquartile range 221-563) days. The Kaplan-Meier estimate for the incidence of target lesion failure at 12-month follow-up was 5.1% (Central illustration): 1.5% in the DCB alone ITT group versus 10.7% in the hybrid DCB+DES group (p=0.073). No cases of cardiac death or target vessel myocardial infarction occurred, while 4 (5.1%) cases of target lesion revascularisation were observed. Time-to-event analysis revealed an incidence of target vessel revascularisation of 6.6%, while no cases of definite/probable acute vessel occlusion were reported. One single patient died because of multiorgan failure, in absence of evident cardiac causes, and no cases of spontaneous myocardial infarction occurred.
The main findings of our study suggest DCB angioplasty alone or in combination with DES implantation in de novo long lesions of large coronary vessels is safe, effective, and allows a reduction in the number and overall length of DES implanted. While recognising the value of stenting, limiting its extent in de novo coronary lesions may have numerous advantages, including a simplified procedure (stent delivery is not always straightforward), a shorter course of dual antiplatelet therapy1, maintained vessel wall reactivity and positive remodelling and lower risk of neoatherosclerosis4. Our results, which are at least comparable to those reported among patients receiving short stents, are reassuring in terms of the incidence of target lesion failure at early follow-up.
Even though the dedicated approach hereby adopted had favourable outcomes3, questions remain about the strategy to pursue according to the result observed after lesion preparation.
Finally, results from prospective randomised controlled trials comparing a metal-limited PCI strategy with current standard of care (ClinicalTrials.gov: NCT04859985, NCT05550233, NCT04893291, NCT05209412) (Colombo A, et al. Drug-coated balloons as a first choice for patients with de novo lesions: pros and cons. EuroIntervention. 2023. In press.) are eagerly awaited.
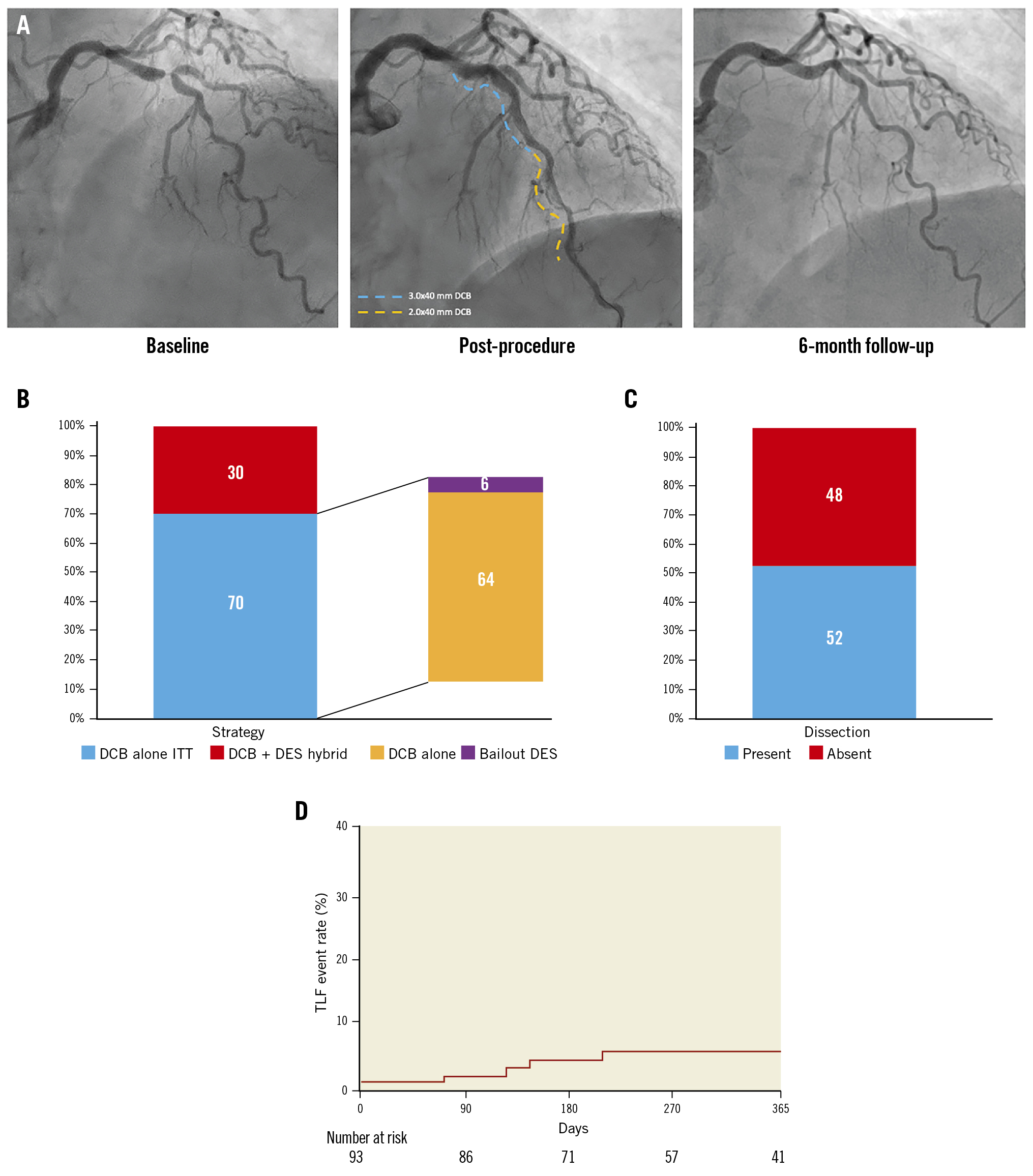
Central illustration. DCB angioplasty in de novo lesions on large coronary vessels. A) Critical calcific lesion of LAD-diagonal bifurcation and mid-LAD. Lesion preparation included cutting balloon inflation; drug delivery with 3.0x40 mm and 2.0x40 mm DCB followed (blue and orange dashed lines, respectively), and a good final angiographic result in absence of flow-limiting dissections was achieved. Six-month angiographic follow-up showed optimal results with satisfactory vessel healing. B) Proportion of patients treated according to each strategy. C) Incidence of intraprocedural angiographically visible coronary artery dissection. D) Time-to-event estimate of the composite endpoint TLF (including target lesion revascularisation, target vessel myocardial infarction or cardiac death) up to 12-month follow-up. DCB: drug-coated balloon; DES: drug-eluting stent; ITT: intention-to-treat; LAD: left anterior descending; TLF: target lesion failure
Conflict of interest statement
The authors have no conflicts of interest to declare.