Introduction
Coronary angiography is the most common diagnostic tool to assess in-stent restenosis (ISR) severity, both in clinical practice and in trials1. However, given its poor ability to depict the relevance of functional stenosis, fractional flow reserve (FFR) has been proposed as the reference standard to ascertain functional ISR severity2. More recently, quantitative flow ratio (QFR) has been validated in de novo lesions as an angiography-based approach to functional stenosis characterisation that does not require intracoronary instrumentation3. We investigated the diagnostic performance of QFR in ISR lesions, using FFR as the reference standard.
Methods
This was a multicentre, international, retrospective, blinded study, enrolling patients from three hospitals in three countries (Hospital Clínico San Carlos, Spain; Toda Chuo General Hospital, Japan; and Sejong General Hospital, Republic of Korea). The study population consisted of a group of ISR patients in whom FFR was used to guide coronary revascularisation. Patients with ISR defined as ≥50% diameter stenosis (DS) within the stent, or within 5 mm from the stent edges, luminal narrowing as judged visually were considered for the study. Details regarding data collection and analysis are available in Supplementary Appendix 1.
Results
QFR analysis was performed in 78 vessels (73 patients) with ISR, all investigated with FFR (Figure 1). Supplementary Appendix 2 and Supplementary Table 1 show details of patient demographics and clinical characteristics. Angiographic and physiological variables are shown in Table 1. Stenosis severity was intermediate both in terms of angiography (mean %DS: 51±9%) and FFR (mean value: 0.79±0.09).
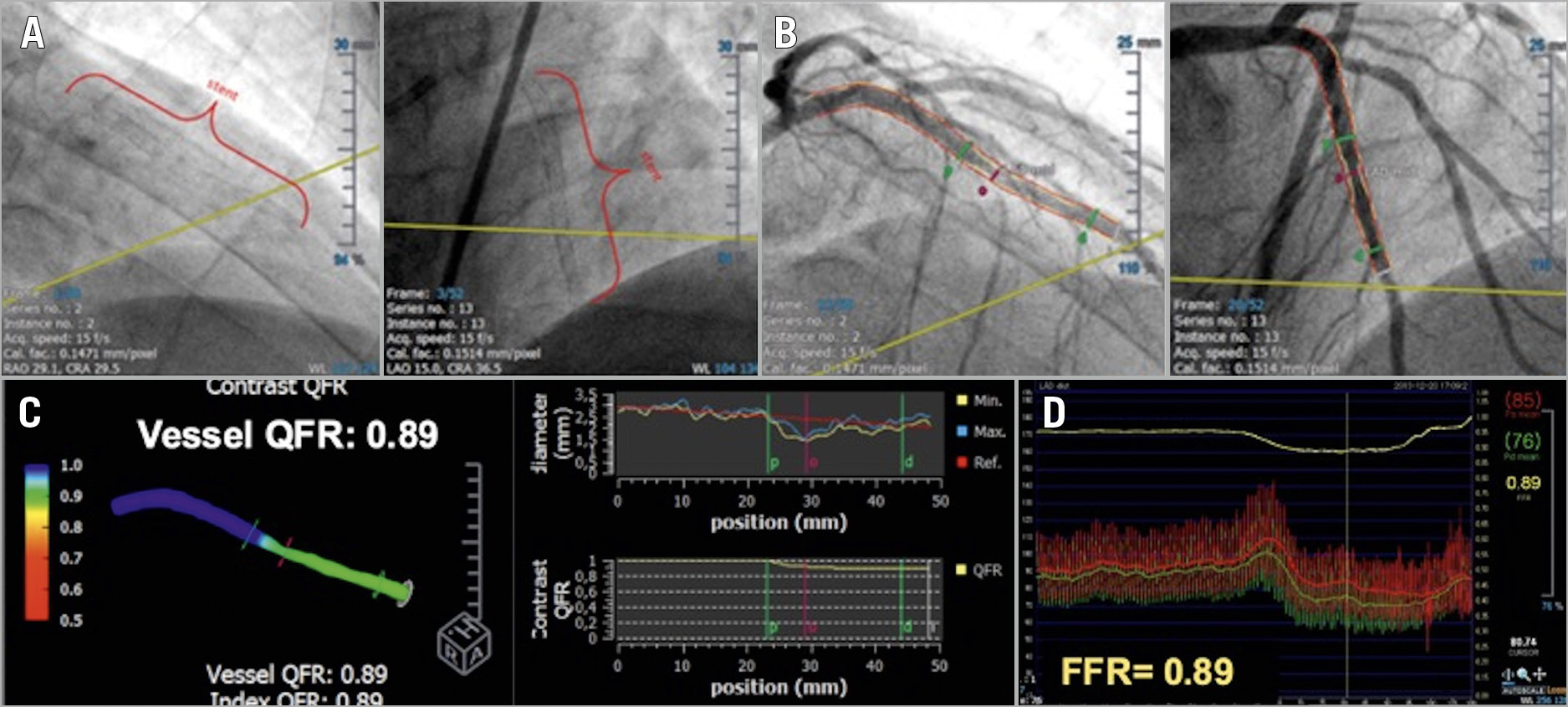
Figure 1. Case example of QFR analysis of intermediate ISR in left anterior descending artery (LAD). A) Long LAD stented segment analysed. B) Two angiographic projections >25° apart allow three-dimensional vessel reconstruction. C) QFR computed based on 3D-QCA and TIMI frame count, resulting in a QFR value of 0.89 (non-significant). Green lines represent the proximal and distal borders of the segment with the most significant lesion and the red line represents the most severe stenosis level. D) FFR value was 0.89.
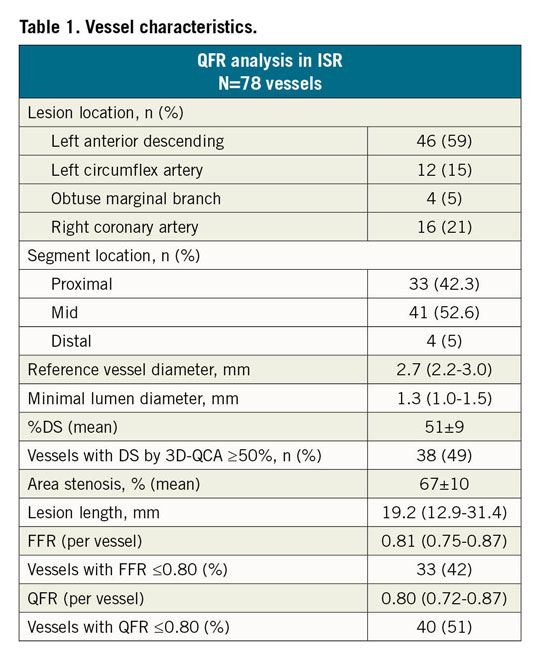
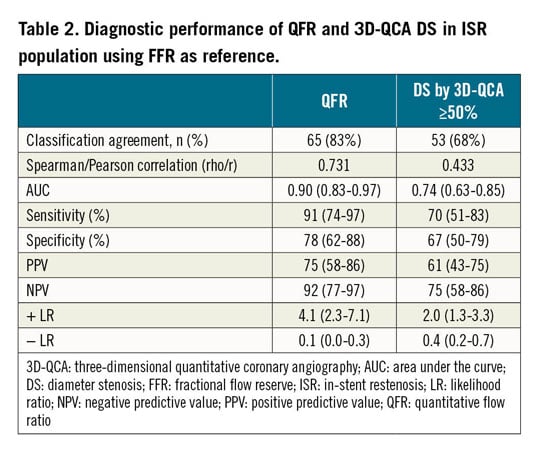
The mean difference between FFR and QFR was only 0.01±0.09 (Supplementary Figure 1). Classification agreement between FFR and QFR (in terms of dichotomous functional significance) was high, i.e., 83%. Functional assessment of ISR lesions with QFR was comparable to that reported in de novo lesions in previous studies (Supplementary Table 2). Additionally, the area under the receiver operating characteristic (ROC) curve (AUC) demonstrated high diagnostic performance of QFR regarding its ability to establish ISR relevance, taking FFR as reference (AUC: 0.90 [0.83-0.97]) (Figure 2). Although there was a difference in classification agreement between vessels, this was not of statistical significance (Supplementary Table 3). The study also confirmed the low diagnostic yield of angiography in ISR: in terms of functional severity a 50% DS criterion correctly classified only 68% of ISR cases (Table 2). QFR analysis of ISR cases correctly reclassified (as judged by FFR) 45% of ISR lesions as functionally non-significant.
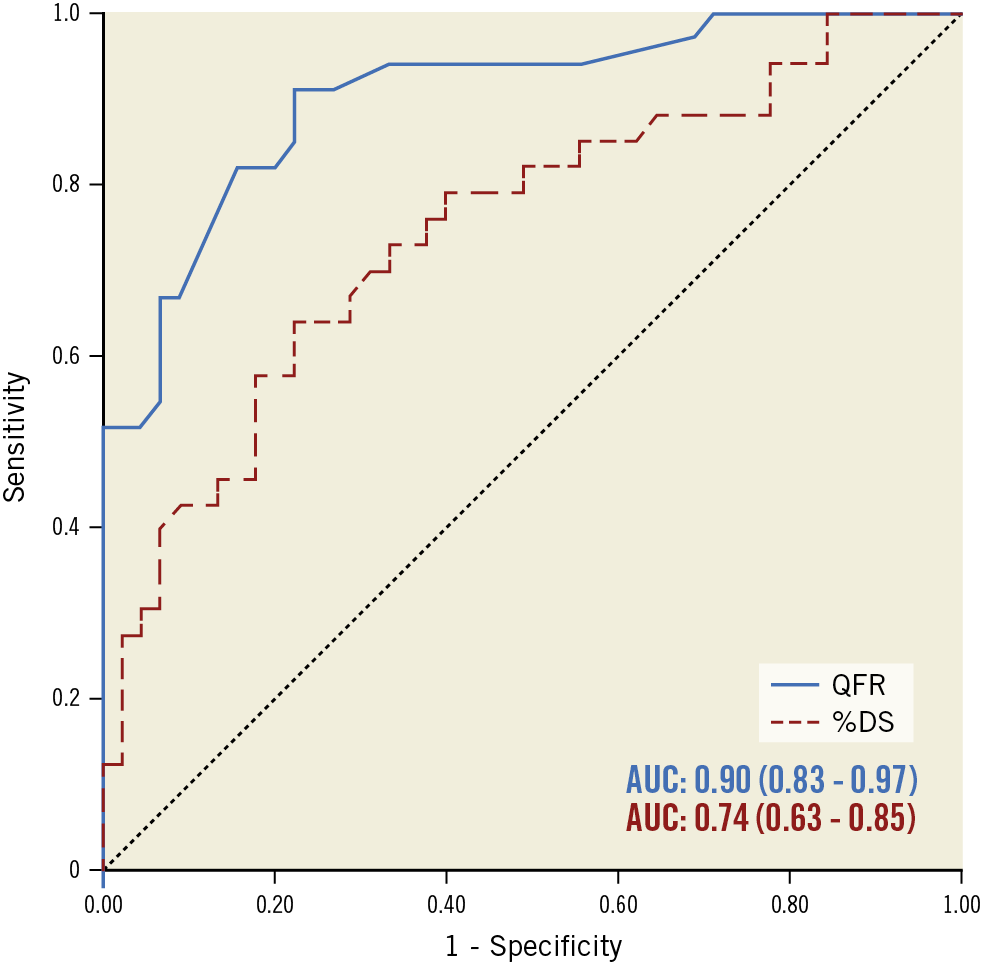
Figure 2. Significant difference in diagnostic performance of QFR and %DS in identifying significant lesions in the ISR population. The area under the curve using FFR as reference standard shows high diagnostic accuracy of QFR but low diagnostic accuracy of %DS for ISR lesions.
Discussion
Our findings support the use of QFR to outline the functional relevance of ISR, with similar diagnostic efficiency to that reported for QFR in major studies in de novo lesions. Compared with available series, the classification agreement of QFR and FFR in ISR lesions was similar to that of two major pivotal studies of QFR-FFR in de novo lesions4,5. Importantly, 45% of the ISR cases deemed significant by angiographic criteria were judged as functionally non-significant both by QFR and by FFR, showing that, due to its high negative predictive value, QFR can lead to safe deferral of revascularisation in a significant proportion of ISR lesions. Furthermore, QFR can be useful as a research tool in assessing the long-term results of stenting.
Limitations
The main limitation of our study was its retrospective character, with exclusion of cases with suboptimal angiography or vessel overlap, something which may have caused selection bias.
Conclusion
QFR has a high diagnostic performance in assessing ISR lesions, similar to that in de novo lesions. It may therefore facilitate adoption of functional assessment in these lesions.
|
Impact on daily practice By not requiring intracoronary instrumentation or drug administration, QFR may facilitate the adoption of functional assessment in ISR. Given its high negative predictive value, QFR will contribute to avoiding unnecessary interventions in patients with ISR. |
Acknowledgements
We are grateful to Pilar Jiménez-Quevedo, MD, PhD, Luis Nombela-Franco, MD, PhD, Carlos Macaya, MD, PhD, and Antonio Fernández-Ortiz, MD, PhD, for their contribution to data acquisition.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.