Introduction
The Carillon® Mitral Contour System® (Cardiac Dimensions, Kirkland, WA, USA) for coronary sinus (CS)-based percutaneous mitral valve repair has demonstrated a reduction in functional mitral valve regurgitation (FMR) in heart failure patients1,2. However, an acute reduction in FMR determined by echocardiography cannot be achieved in all patients: the AMADEUS trial reported that there was no acute effect on FMR in 18.6% of the patients2. However, three-dimensional (3D) imaging modalities for percutaneous valve interventions have been implemented in clinical routine. For example, multislice computed tomography (MSCT) is pivotal for procedural planning of transcatheter aortic valve implantation (TAVI). This valuable technique may offer unique 3D CS/great cardiac vein (GCV) and mitral annulus reconstructions to analyse their anatomical relation using the latest technology. Based on the results of CT-based 3D CS/GCV and mitral annulus reconstructions, we aimed to analyse the rate of patients with a sustained reduction of FMR three months after Carillon device implantation using echocardiographic assessment.
Methods
The study comprises 11 consecutive patients undergoing Carillon device implantation at our institution with prior MSCT and baseline, post-procedure and three-month transthoracic echocardiography. Patients with symptomatic (>Class II New York Heart Association [NYHA]) dilated ischaemic or non-ischaemic cardiomyopathy (left ventricular ejection fraction [LVEF] <40%) on stable heart failure medication (medication prior to implantation: beta-blocker, n=11, 100%; ACE inhibitor/AT2 antagonists, n=11, 100%; spironolactone/eplerenone, n=6, 54.5%; diuretics, n=11, 100%) suffering from at least moderate FMR were eligible for percutaneous annuloplasty3. Responders were defined as having echocardiographic improvement of the vena contracta, proximal isovelocity surface area (PISA), effective regurgitant orifice area (EROA) and regurgitant volume at three-month follow-up. We defined non-responders as having at least three parameters which remained unchanged at follow-up. The 3mensio Structural Heart software (Pie Medical Imaging BV, Maastricht, the Netherlands) enables mitral valve annulus and CS reconstruction. The distance and angle of the mitral valve annulus (MVA) plane and a CS/GCV plane were calculated (Figure 1).
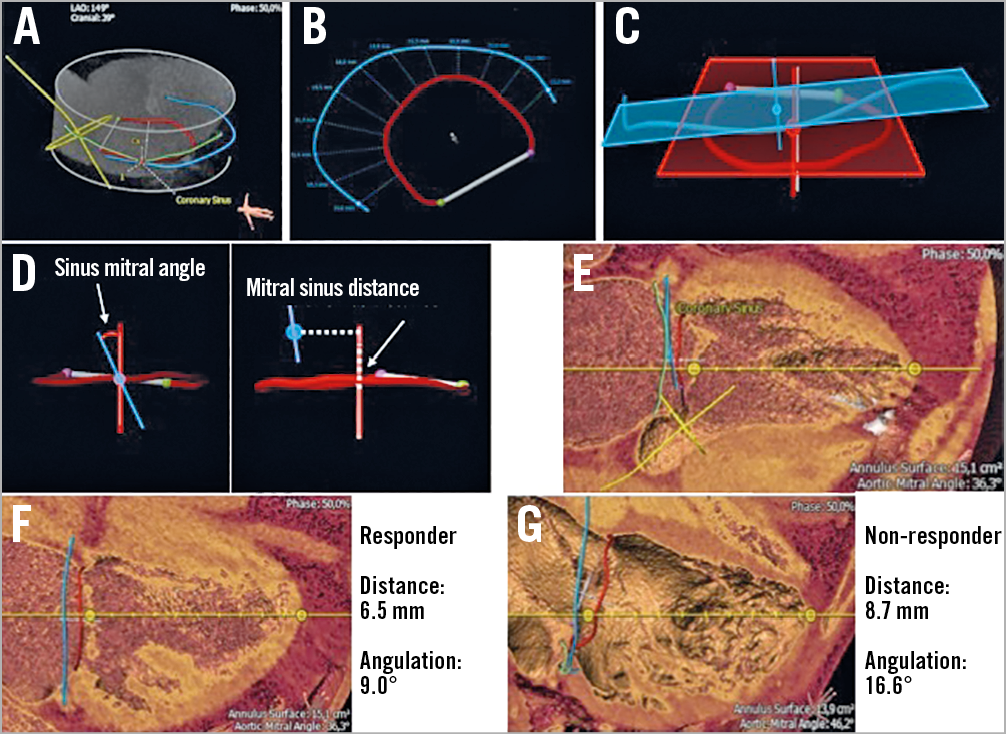
Figure 1. Usage of CT angiography reconstruction to determine coronary sinus anatomy and relation to the mitral valve annulus. A) Blue line: coronary sinus. Green line: left circumflex artery. Red line: mitral annulus (D-shaped). Yellow line: aortic valve. B) Variable distances of CS to MVA. C) MVA and CS plane as a 3D model. D) Calculation of angulation and distance of MVA and CS planes. One plane for the MVA and one plane for the CS were calculated. To determine the distance a measurement from centroid to centroid of the 3D planes is carried out. Therefore, a perpendicular line is projected from the CS centroid towards the normal line of the mitral annulus. A straight distance is measured from the annulus centroid over the normal line of the mitral annulus towards the transection point of the projected CS line. For the angulation measurement centroids and normal (direction) are overlaid and an angle measurement between the CS and normal line of the annulus is derived. E) CS (blue), MVA (red), left circumflex artery (green) and aortic valve (yellow). F) Responder. G) Non-responder.
Results
A total of 11 patients with implantation of a Carillon device, prior CT angiography (CTA) and three-month follow-up transthoracic echocardiography were enrolled in this retrospective study. Figure 1 shows original reconstruction imaging from the 3mensio Structural Heart software prototype and Table 1 shows angulations and distances in responders and non-responders.
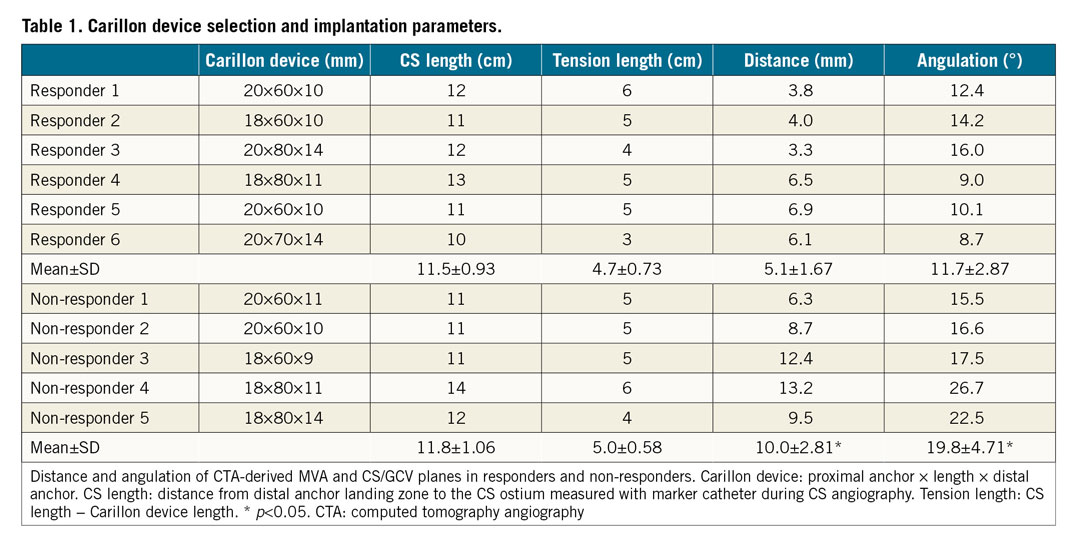
Figure 2 shows significant improvement of the vena contracta, PISA, EROA and regurgitant volume in responders but not in non-responders over a period of three months. Comparison of the distance and angulation of the CS plane and the MVA plane showed a shorter distance and lower angulation in responders (distance: responders 5.1±1.7 mm versus non-responders 10.0±2.8 mm; angulation: responders 11.7±2.9° versus non-responders 19.8±4.7°). Our results suggest that a CS plane and MVA plane with a distance of <6.9 mm (sensitivity 100%, specificity 80%, area under the curve [AUC] = 0.933) and an angulation of <14.2° (sensitivity 83.3%, specificity 100%, AUC = 0.967) could be considered for predicting a reduction in FMR after mitral annuloplasty using the Carillon device.
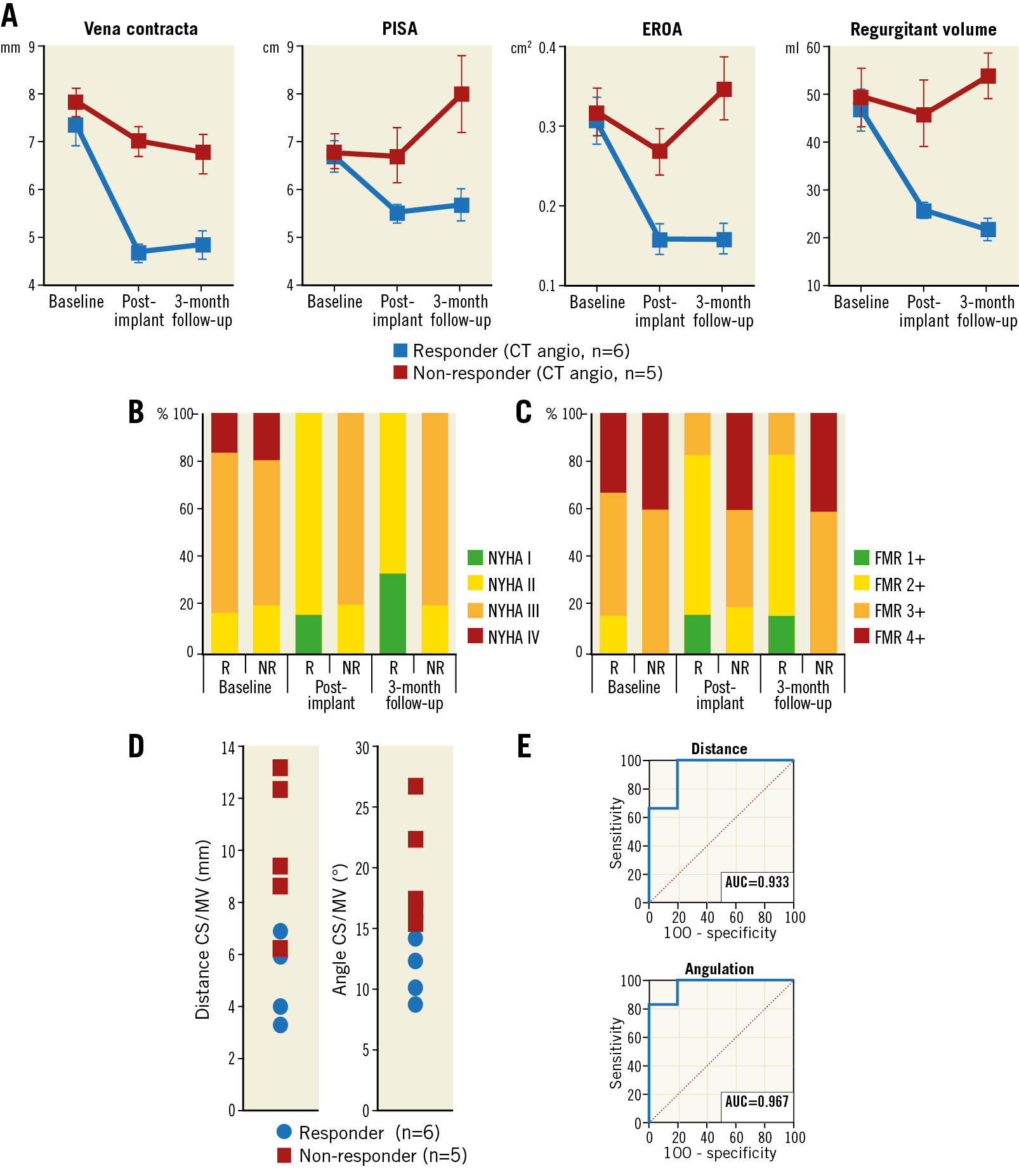
Figure 2. Relationship of the coronary sinus and mitral annulus in responders and non-responders following percutaneous coronary sinus-based mitral valve repair. A) Vena contracta, PISA, EROA and regurgitant volume at baseline, post implantation and three-month follow-up (FU). B) NYHA classification at baseline and during follow-up. C) FMR classification at baseline and during follow-up. D) Dot plots of distance and angulation of coronary sinus and mitral annulus. E) ROC curve analysis of distance and angulation of coronary sinus plane and mitral annulus plane. NR: non-responder; R: responder
Discussion
Clinical data for the Carillon Mitral Contour System showed a good safety profile. Furthermore, clinical trials documented a reduction of echocardiographic FMR parameters and improved heart failure symptoms1,2. However, in an AMADEUS trial sub-analysis, no difference of the CS/GCV position relative to the MVA was found in patients with or without acute reduction of FMR based on MSCT4. However, linear distances from the edge of the MVA to the centre of the vein lumen were exclusively measured in long-axis views. To determine the distance more precisely, we used 3D reconstructions generating an MVA and CS/GCV plane.
Our results suggest that shorter distance and lower angulation of the CS plane to the MVA plane might have an impact on procedure success up to three-month follow-up. However, coronary sinus anatomy is highly variable and other parameters might influence the clinical success of CS-based mitral annuloplasty. Therefore, further studies are needed to prove a potential benefit of CT angiographic screening to predict the acute and long-term response of FMR after Carillon device implantation.
Study limitations
This is a retrospective, non-validated, single-centre study and it enrolled a small number of patients. Therefore, the results should be regarded as hypothesis-generating and need to be verified by randomised, multicentre trials.
Conclusion
The distance and angulation of MVA and CS/GCV planes from 3D reconstructions of MSCT have the potential to predict the echocardiographic and clinical impact of percutaneous mitral valve repair using the Carillon Mitral Contour System; however, further clinical studies are needed.
|
Impact on daily practice Carillon device implantation into the CS is effective in reducing FMR. Using the 3D MSCT-derived distance and angulation of CS/GCV to MVA planes has the potential to predict echocardiographic and clinical non-responders after Carillon device implantation. |
Conflict of interest statement
H. Degen is a consultant for Biotronik and Cardiac Dimensions. M. Haude has received institutional grants/research support from Abbott and Biotronik, and honoraria or consultation fees from Biotronik, Cardiac Dimensions, OrbusNeich and Philips. M. Chatrou is an employee of Pie Medical Imaging. The other authors have no conflicts of interest to declare.