Overview
Invasive cardiology was initiated in North Africa more than fifty years ago with the first catheterisation procedure performed in Tunis in 1968. In the same year, there was the first surgical valve replacement and the first surgical closure of an atrial septal defect (ASD). The first coronary angiogram was performed in 1983, the first pulmonary and mitral valvuloplasty in 1986, and the first coronary angioplasty in 1989.
Because of the high prevalence of rheumatic heart disease in North Africa at that time, interventional cardiology was focused initially (in the early 1980s) on the percutaneous therapy of mitral stenosis and some congenital heart disease such as ASD and patent ductus arteriosus (PDA) closures.
However, beginning in the early 1990s, there was a dramatic decline in rheumatic heart disease that was progressively replaced by an epidemic of coronary heart disease, resulting in a pressing need for coronary revascularisation procedures, including percutaneous coronary interventions (PCI). As shown in Figure 1, the current decade has witnessed an exponential growth in the number of coronary angiograms, PCI and stents used.
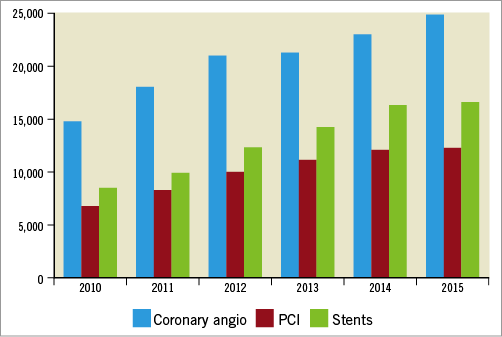
Figure 1. Annual number of coronary angios, PCI and stents used in Tunisia.
Since its emergence as a new subspecialty, interventional cardiology has evolved quite rapidly in North Africa compared to the other African countries apart from South Africa. The proximity of these African countries to Europe and particularly to France has helped that progression, as trainees have relatively easy access to French centres for subspeciality training.
Initially, patients in need of percutaneous cardiac intervention, particularly balloon mitral valvuloplasty or coronary interventions, were sent to France. However, the high cost of that approach has prompted the decision to send young cardiologists for training in preference to sending patients for care.
The purpose of this manuscript is to analyse the challenges of the current practice of interventional cardiology in North Africa, specifically in Tunisia, Algeria, Morocco and Egypt, and the opportunities offered for further development of this subspecialty in that part of the continent to make it a platform for education, training and healthcare for the other African countries.
Challenges
1. As in the majority of countries, North Africa has a two-tiered health system, a public system which is chronically underfunded but covers the majority of the population, and a private health system that is rapidly expanding thanks to the increasingly wider coverage by national insurance. This is particularly true in Tunisia where the national insurance covers more than 80% of the population; the remaining 20% are covered by the government. The private sector, where salaries are much higher, is increasingly attracting not only cardiologists but also nurses and cath lab technicians, resulting in the worsening of the current situation of a reduction in available personnel.
2. Education of cardiologists in North Africa is very good, with five years at medical school and, in addition, one to two years of internship and four years of training in general cardiology. There is no dedicated fellowship track for interventional cardiology; however, the majority of fellows have the opportunity, although this has become more difficult lately, of spending one or two years abroad for training, particularly in France. The majority of the trainees are attracted to the disciplines of interventional cardiology and electrophysiology. Many of those fellows do not return to their home countries and prefer to remain in Europe where salaries are much higher and life is more comfortable; this substantial brain drain has also been noted in many of the sub-Saharan African countries. Moreover, the majority of those who do return opt to work in the private sector over the public sector for the same reasons.
3. The quality of the reimbursement system is variable across North African countries. It is excellent in Tunisia, particularly for interventional cardiology procedures. However, having an excellent reimbursement system is a double-edged sword as this is good for the patient but tends to encourage abuse by performing unnecessary procedures.
4. Management of STEMI patients in North Africa has its limitations but the level of access and standards of care are very acceptable compared to most other African countries. The adhesion of Egypt and Tunisia to the Stent for Life initiative1 will probably have a positive impact on the improvement of STEMI care. Thrombolysis is widely available, initially with streptokinase though this is being replaced rapidly by tenecteplase.
Primary PCI is also increasing quite rapidly with the proliferation of cath labs, more in the private sector than in the public. The problem is the lack of adequate geographic distribution of cath labs across the country. The majority of cath labs are concentrated in big cities and along the coast. Thus, patients in remote and rural areas have limited access to emergency medical services (EMS) and to primary PCI. Also, there is the issue of the management of patients presenting at night. In a resources-constrained environment in which the availability of a cath lab and an interventionalist on a 24/7 basis is seriously limited, many of those patients will receive lytics and then be taken to the cath lab one or two days later, thus increasing the financial burden of STEMI care in those patients.
Opportunities
North Africa has an excellent educational system that has produced a number of high-quality cardiologists with a respectable number in relation to the size of the population. There are currently around 500 cardiologists in Tunisia for 11 million inhabitants whereas there are only 170 cardiologists in South Africa for a population of 55 million. At least two hundred are interventional cardiologists, very well trained, although without an official certification as there is no dedicated track for interventional cardiology in North African countries. Such a number of cardiologists will be able to cover not only the needs of the local patients but also those coming from the surrounding countries and even beyond. There is also the possibility for those cardiologists to travel to sub-Saharan African countries for proctoring, contributing to capacity building and teaching.
The expansion of cardiovascular interventions in North Africa has been accompanied by several high-quality clinical research publications mainly on balloon mitral valvuloplasty1-12. Some of these have had a considerable impact on the literature3-5. This indicates that the North African cardiology community has the potential and talent to expand its high-quality research profile. What is needed, and needs to be encouraged further, is the involvement in multicentre multinational registries and clinical trials, and collaboration with investigators in other countries in Africa, Europe and elsewhere.
The proximity to Europe is a great opportunity, allowing interaction, collaboration for proctoring, research and training.
Recommendations
The disparity in the quality of care between university hospitals and regional/rural institutions is striking11 and should be examined carefully not only in order to organise the transfer of patients from those hospitals to tertiary centres but also to establish cardiology units able to ensure an appropriate diagnosis and the minimal urgent care of patients with acute presentations. Initiatives such as Stent for Life and the most recent WHO Emergency System Framework will most likely overcome this geographic disparity in the quality of care. There must be attractive incentives to young cardiologists to work in institutions usually located in remote areas far from the larger and more attractive cities.
There is also a huge disparity in earnings between interventional cardiologists working in public institutions and those in the private sector which is attracting the majority of young interventional cardiologists, resulting in a lack of interest among the younger generation in an academic career which used to be considered very prestigious. This situation has also resulted in a lack of interest among fellows who are sent to Europe for training to come back to the country. If governments do not intervene to preserve the public sector and particularly the university sector, the whole education system may fall apart and the achievements mentioned above will be lost.
Because of the frustration felt by the elite in academic institutions, there is not much interest in research. The only category of cardiologists interested in some clinical research are those who will be applying for consultant or academic positions in the near future. Once in an established position, this potential and intellectual talent needs additional incentives to boost research.
Because of a reimbursement issue and a lack of interest in complex structural and congenital heart disease interventions, these latter procedures have not evolved to the extent that they should. To overcome this limitation, it would be relevant to built centres of excellence at a national but also at a regional level. This will allow expertise and force the system to accept reimbursement.
Conclusions
North Africa has a great potential for educational and cardiovascular care with quite a large number of very well trained cardiologists who can benefit not only the North African system but also the other African countries that are far behind. However, there are serious challenges that threaten the system, mainly related to a huge disparity in earnings between the public and private sector, and the brain drain. In addition, the lack of recognised centres of excellence has resulted in a slow progression of new complex interventional procedures such as transcatheter aortic valve replacement (TAVR) and rotablation, and the use of valuable tools such as intravascular ultrasound (IVUS), optical coherence tomography (OCT) and fractional flow reserve (FFR)/ instantaneous wave-free ratio (iFR).
Conflict of interest statement
The author has no conflicts of interest to declare.