In 2012, the residual SYNTAX score emerged as an efficient method to evaluate the contribution of non-culprit coronary lesions – based on their anatomic features – to the remaining cardiovascular risk of patients with multivessel disease treated with primary percutaneous coronary intervention (PCI)1. The residual SYNTAX score has been well validated across different clinical presentations including the most complex such as myocardial infarction (MI) with cardiogenic shock2. Then, landmark trials demonstrated that non-ischaemia-guided PCI of non-culprit lesions was superior to medical treatment only in patients with ST-elevation myocardial infarction (STEMI), but with inconsistent reductions in hard endpoints such as recurrent MI and death3,4. Going a step further, the DANAMI-3—PRIMULTI trial demonstrated that complete revascularisation of patients with STEMI guided by fractional flow reserve (FFR) reduced ischaemic events, mostly by reducing repeat revascularisation with no effect on death and recurrent MI5. The FLOWER-MI trial, also evaluating FFR to guide the treatment of non-culprit lesions in patients with STEMI, was presented at ACC 20216. There are currently no data concerning non-hyperaemic pressure ratios to assess coronary lesions during STEMI (Figure 1). As a result, the question remains regarding the appropriate evaluation of non-culprit stable lesions in patients with STEMI and multivessel disease, especially after the results of the ISCHEMIA trial in the treatment of stable coronary lesions7.
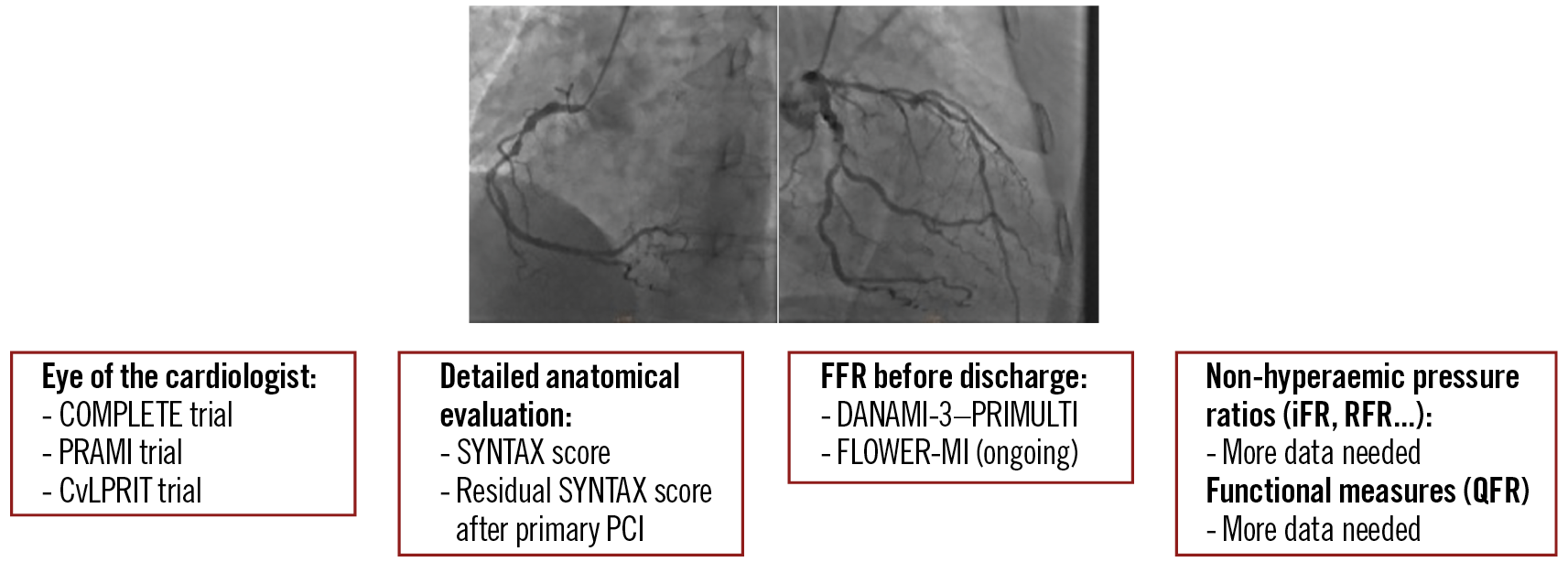
Figure 1. Management of non-culprit lesions in patients with STEMI.
In the study in the present issue of EuroIntervention, the hypothesis of Tang et al was that the residual SYNTAX score guided by coronary physiology would improve the risk stratification of patients admitted with STEMI and multivessel disease8.
Using quantitative flow ratio (QFR) – a physiologic measure using angiographic projections to evaluate stenosis, without hyperaemia or dedicated wire9 – the investigators reviewed the angiograms of 354 consecutive patients with STEMI: 57.6% were considered as having a complete revascularisation, and 42.4% were considered as having an incomplete revascularisation (residual SYNTAX score according to QFR ≥1). Importantly, QFR downgraded to a low-risk category 1 in 3 patients considered to have a high or intermediate residual SYNTAX score by the operators; no patients were upgraded to a higher risk. The investigators reported that patients with an incomplete revascularisation according to QFR were more likely to suffer from further ischaemic events, mostly new revascularisation. Eventually, the use of a QFR-based residual SYNTAX score improved the risk stratification of major adverse cardiac events at two years.
The observations described by Tang et al are important, as they remind us that myocardial ischaemia is not the only determinant of prognosis. Anatomic characteristics reflecting plaque vulnerability, atheroma volume or complex lesions (evaluated by coronary imaging) and flow limitations (measured by physiology tools such as QFR or FFR) can predict coronary risk. The combination of both anatomic and physiologic evaluations may help reconsideration of the severity of some lesions and avoid inappropriate revascularisation, or in contrast may avoid leaving patients with flow-limiting lesions at risk of further ischaemic events10.
These observations highlight the need for randomised trials evaluating innovative coronary physiologic methods for patients with complex coronary artery disease. We currently live in a disturbing period for the treatment of stable and often asymptomatic coronary lesions, with positive trials encouraging complete revascularisation of non-culprit lesions in STEMI, but negative trials for immediate complete revascularisation in cardiogenic shock and other negative trials for revascularisation of stable coronary artery disease even in the presence of ischaemia. The time may have come for shifting gear towards an approach combining anatomic and physiologic evaluations for our decisions of revascularisation of stable coronary lesions.
Conflict of interest statement
G. Montalescot reports research funds or honorarium fees from Abbott, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Bristol-Myers Squibb, CellProthera, CSL Behring, Europa, Idorsia, SERVIER IRIS, Medtronic, MSD, Novartis, Pfizer, Quantum Genomics, and Sanofi-Aventis. M. Zeitouni reports research grants from Fédération Française de Cardiologie, Institut Servier, BMS/Pfizer, and Bayer.
Supplementary data
To read the full content of this article, please download the PDF.