Abstract
Aims: Transcatheter aortic valve replacement (TAVR) is a promising therapeutic option for patients with severe aortic stenosis (AS) considered at too high risk for conventional aortic valve replacement. The balloon-expandable Edwards valve can be implanted using either the transfemoral or transapical routes, depending on arterial ilio-femoral suitability. The aim of the study was to evaluate the usefulness of ilio-femoral angiography as an initial screening tool for TAVR using the transfemoral approach with the Edwards SAPIEN valve.
Methods and results: Aortography with bilateral ilio-femoral run-off was assessed in the antero-posterior projection. Minimal arterial diameter, vessel tortuosity and calcification were assessed. Transfemoral implantation was appropriate when the minimal arterial diameter was >7 mm for a 23 mm trans-catheter heart valve (THV) and >8 mm for a 26 mm THV with limited calcifications and tortuosity. Included were 135 patients with severe aortic stenosis undergoing cardiac catheterisation before conventional aortic valve replacement or TAVR. Mean femoral artery diameter was 7.5±1.3 mm and mean iliac artery diameter was 9.3±2.3 mm. There was no or moderate tortuosity in 72% of them. Calcifications were absent or moderate in 83%. At first sight, the transfemoral route was considered potentially suitable in 71% of patients for a 23 mm THV and 39% of patients for a 26 mm TAVI.
Conclusions: In the course of haemodynamic and angiographic evaluation of patients with severe symptomatic aortic stenosis, angiography of the ilio-femoral access can be used as a first screening modality to determine potential candidacy for a transfemoral TAVR using a balloon expandable THV.
Introduction
Transcatheter Aortic Valve Replacement (TAVR) has become a therapeutic alternative for patients with severe symptomatic Aortic Stenosis (AS) who have an elevated risk of surgical mortality or have a contraindication to surgery. Cribier et al1, reported the first successful TAVR and since then, over 6,000 patients have been treated successfully utilising the Edwards SAPIEN balloon expandable prosthesis (Edwards Lifesciences, Irvine, CA, USA) or the CoreValve ReValving self expandable system (Medtronic, Minneapolis, MN, USA)2-8. Both valves can be placed through a retrograde (transfemoral) approach, however, only the SAPIEN valve can be implanted transapically.
The main limitation for transfemoral TAVR is the size of the ilio-femoral arterial diameter. The Edwards SAPIEN prosthesis is available in two sizes (23 and 26 mm) that are placed through a 22 Fr or 24 Fr arterial sheath, which require a minimal arterial diameter of >7 and 8 mm respectively. (Figure 1)

Figure 1. Various measurements of femoral and iliac diameters on angiographic AP view.
A minimal diameter of 6 mm is required for the insertion of the 18 Fr sheath utilised by the CoreValve ReValving system. Invasive angiography, intravascular ultrasound, CT or MRI imaging can be utilised for the evaluation of arterial luminal diameter, vascular calcification or tortuosity. The goals of this study were 1) to assess by angiography the ilio-femoral anatomical characteristics of patients with severe aortic stenosis; 2) to assess the potential value of this imaging technique as a preliminary screening test before TAVR using the Edwards SAPIEN valvular prosthesis and 3) to evaluate from this simple test the percentage of patients that might potentially be candidate (or be rejected) for transcatheter heart valve (THV) implantation using the transfemoral route.
Methods
Prospectively included in the study were 135 consecutive patients with severe symptomatic AS (aortic valve area <1 cm2, <0.6 cm2/m2) undergoing cardiac catheterisation before conventional aortic valve replacement or TAVR from May 2006 to August 2007. Patients gave informed consent for participation in the trial.
Angiography
All patients underwent distal aortogram with bilateral ilio-femoral run-off in the antero-posterior projection. Twenty to 30 ml of contrast (Iomeprol, Bracco, Imaging France) was injected by a power injector (Medrad Inc., Warrendale, PA, USA) at a rate of 15-18 ml/sec through a 6 Fr pigtail catheter placed above the iliac bifurcation. Images were evaluated for luminal diameter, vessel tortuosity and degree of calcification to assess potential suitability for TAVR.
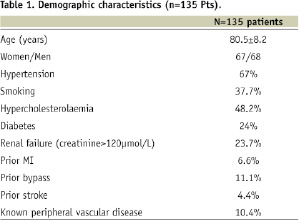
Mean diameter was measured for every segment between the distal aorta and bilateral common femoral arteries using the 6 Fr catheter as a reference. The smallest luminal diameter was noted. The recommended minimal arterial luminal diameters are greater than 7 and 8 mm for the 23 and 26 mm valve respectively in the absence of circumferential calcification. Measurements and qualitative assessment was performed by one blind operator (Figure 1). Vessel tortuosity was graded in the same AP view utilising the following scale: 0) no tortuosity; 1) mild tortuosity (30°-60°); 3) moderate tortuosity (60° to 90°), and 4) marked tortuosity (≥90°). (Figure 2)
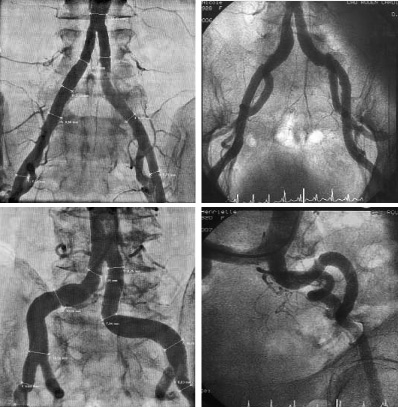
Figure 2. Assessment of ilio-femoral tortuosities (grade 0 to grade 3).
Vessel calcification was assessed by fluoroscopy prior to contrast administration and graded using the following scale: 0) no calcification, 1) mild discrete calcification, 2) moderate calcification, 3) severe calcification.
Patients were considered candidates for the transfemoral approach when the following criteria were met: 1) a minimal ilio-femoral diameter of ≥7 and ≥8 mm for the 23 and 26 mm valve respectively; tortuosity ≤2, and calcification ≤2.
Statistical analysis
Numerical data are expressed as mean and standard deviation. Continuous variables were analysed with the T-test, and qualitative variables with chi-square using the statistical package Statview 5.0. Statistical significance was defined a priori with a p value less than 0.05.
Results
There were 135 patients included in this study. Mean age was 80.5±8.2 years (51 - 95 years) and 50% were female. Hypertension was present in 67% of them and 24% were diabetics. Other characteristics are reported in Table 1.
Haemodynamic and angiographic characteristics are presented in Table 2.
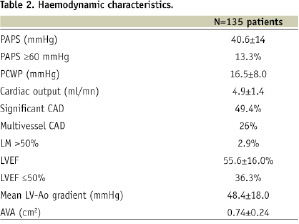
Coronary artery disease was present in 49% of the patients and multivessel disease was present in 29%. Aortic stenosis was severe in all with a mean valve area of 0.74±.24 cm2 and a mean transvalvular gradient of 55±16 mm Hg. Left ventricular ejection fraction was 55±16%.
The distal aorta, right and left iliac and femoral, arteries were assessed (270 arteries in 135 patients) (Table 3).
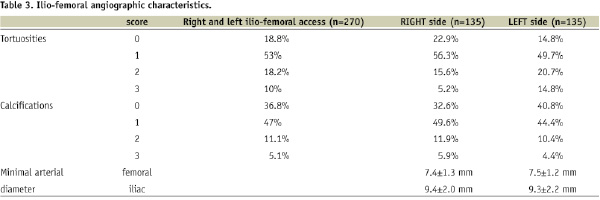
Mean femoral artery diameters were similar on both sides: respectively 7.4±1.3 mm and 7.5±1.2 mm (p=0.15). Mean iliac artery diameters were respectively 9.4±2.0 and 9.3±2.2 mm, p=0.57. Calcifications were absent or minimal (Grade 0 or 1) in 83.8% of cases, grade 2 in 11.1% and grade 3 in only 5.1%. Distribution of calcifications was similar on the right and left sides (p=0.6). Vessel tortuosity was graded as 0 to 1 in the majority of patients (71.8%), grade 2 in 18.2% and grade 3 in 10%.
Using the combination of the three parameters, the femoral approach appeared suitable in 71% of patients for the 23 mm TAVR and 39% of patients for the 26 mm TAVR. In other words, 29% and 61% of patients would have been declined for a 23 mm and 26 mm THV implantation respectively after this simple angiographic test in a single antero-posterior view. Of note that 90% of patients had a minimal artery diameter >6 mm without excessive calcifications or tortuosity.
Discussion
Degenerative aortic stenosis is the most frequent valvular disease in developed countries and aortic valve replacement is the treatment of choice for a majority of symptomatic patients with severe AS. However, mortality and morbidity increase with age and associated comorbidities; transcatheter aortic valve replacement (TAVR) was developed as an alternative therapeutic option for high risk or non-surgical patients. Since the first case performed in 2002 by Cribier et al1, and with technological improvements, more than 3,000 patients have been implanted worldwide with the balloon expandable THV using either the transfemoral2-8 or transapical approaches9. Implantation success rate is high, >95%, and one-month mortality is around 10%.
With the currently used Edwards SAPIEN bioprosthesis, the ilio-femoral access is critical for appropriate selection of the implantation route. Prosthetic valve sizing is based on the aortic annulus diameter: a 23 mm valve is placed when the aortic annulus measures 18-21 mm, and a 26 mm valve is used in an annulus of 21-25 mm. The 23 mm valve requires a 22 Fr sheath, which has an internal diameter of 7.62 mm and an outer diameter of 8.38 mm; while the 24 Fr sheath, required for the 26 mm valve, has an internal and external diameter of 8.38 and 9.4 mm respectively. In the absence of moderate calcification or tortuosity, a minimal lumen diameter of 7 and 8 mm is required for the 22 and 24 Fr sheath respectively. When the arteries do not fulfil these characteristics, transapical implantation is indicated in order to reduce vascular complications.
Angiography provides a gross assessment of lumen diameter and vessel tortuosity. It also presents information on the degree of vessel straightening after insertion of a guidewire or catheter. In addition to angiography, CT-scan is crucial and must be performed in all cases, since it allows a finer assessment of the vessel wall, lumen, and trajectory. Image post-processing allows the ability to create a three- dimensional reconstruction of the ilio-femoral arteries for procedural planning. Transverse (axial) slices of the vessel are obtained to evaluate the degree of vessel calcification, calcium extension into the lumen, and minimal luminal diameter. This information provides an effective vessel analysis and ensure appropriate patient selection to avoid vascular complications. However, CT angiography requires the addition of iodinated contrast and increases exposure to radiation. Intravascular ultrasonography of the iliac and femoral arteries provides detailed information of the vessel lumen and wall. However it is an invasive procedure, image quality is dependent on vessel tortuosities (when using a transducer with a mechanical array), and may also provide distorted diameters due to vessel tortuosity if the imaging catheter is not centred in the lumen.
An AP angiogram of the distal aorta with ilio femoral run off identified on first sight 71% and 39% of potential patients for transfemoral TAVR requiring a 23 mm and 26 mm valve respectively, these results needing to be confirmed by CT-Scan. On the other hand, the transapical approach could be considered the most appropriate solution in 29% and 61% of patients respectively. Ongoing technological developments (18 Fr SAPIEN XT bioprosthesis) will decrease the required sheath size by 4 to 5 Fr, resulting in a 18 Fr sheath for a 23 mm THV and 20 Fr for a 26 mm valve. Based on the existing series, this change would allow transfemoral implantation in 80 to 90% of the patients. This should have an impact on vascular complications and on increased rate of implantations using transfemoral approach.
Limitations of the study
A more accurate assessment of the ilio-femoral access by angiography would have required multiple contrast injections in different views. In this study, angiography was intentionally limited to a single antero-posterior view in a population of patients who were undergoing diagnostic cardiac catheterisation for aortic stenosis. At least two views (antero-posterior and left anterior oblique) are generally required for a pre-THV screening procedure and CT-Scan is crucial to detail the arterial internal diameter, tortuosity, and calcium distribution. Also, the straightening effect of the pigtail catheter might have lead to under appreciation of the degree of tortuosity on the catheterisation side.
Conclusions
In the course of haemodynamic and angiographic evaluation of patients with severe symptomatic aortic stenosis, angiography of the ilio-femoral access can be used as a first screening modality to determine potential candidacy for a transfemoral TAVR using a balloon expandable THV. In our study, the current catheter sizes constitute a limitation to this approach in 29% and 61% of potential candidates for a 23 or 26 mm THV respectively. The upcoming decrease in sheath size by 4 to 5 Fr will considerably increase the suitability of the transfemoral approach in the near future.

