Abstract
Aims: Patients aged ≥80 years are often excluded or under-represented in trials assessing treatment modalities in STEMI. We assessed in-patient outcomes in elderly patients undergoing contemporary primary PCI (PPCI).
Methods and results: From Sept 2005 to July 2011 patients undergoing PPCI in our centre were identified. Demographic details, procedural data and in-patient outcomes were collated. Those aged ≥80 years were compared with those aged <80 years. In the study period 1,218 patients required PPCI, of which 224(18.4%) were ≥80 years. The elderly cohort were more likely to be female (44.3% vs. 20.3%; p<0.001), and have significant comorbidities. Times from first medical contact until TIMI 3 flow were similar between the two groups (medien 102 min vs. 109 min; p=0.19). There was no difference in rates of PCI success (97.3% vs. 98.3%; p=0.24), drug-eluting stent use (63.5% vs. 63.3%; p=1.00) and number of stents used. In-patient outcomes were worse in the elderly cohort with significantly higher rates of death (11.2% vs. 3.7%; p<0.001) and acute kidney injury (12.9% vs. 4.0%; p<0.001), with a trend towards more post-procedure cardiovascular accidents (CVA), access site complications and reinfarction. Length of stay was significantly longer in the elderly cohort (median days 5 vs. 3; p<0.001).
Conclusions: Important demographic differences exist in very elderly patients presenting with STEMI compared to younger patients though procedural data and PCI success rates are similar between the two groups. Those aged ≥80 years have significantly worse in-patient outcomes though death rates are not as high as historical data suggests.
Introduction
In developed countries, cardiovascular disease remains the most common cause of mortality in those aged >65 years1,2. Despite this, elderly patients are poorly represented in research studies related to cardiovascular disease with up to 50% of randomised controlled trials studying treatment strategies in the management of acute coronary syndromes explicitly excluding elderly patients from enrolment, and other studies without overt age exclusions enrolling very few patients aged 80 or older3.
Reperfusion therapy is now standard in the management of ST elevation myocardial infarction (STEMI) with several randomised trials and large meta-analyses demonstrating primary percutaneous coronary intervention (PPCI) to be superior than thrombolysis as the treatment of choice in these patients4,5. Yet many of the studies included in the meta-analyses excluded elderly patients from enrolment6-10. Trials assessing PPCI in the elderly have been performed and appear to suggest superiority over thrombolytic therapy but data has been considered inconclusive and the definition of what constitutes elderly has not been uniform11-13. Furthermore it is clear that in practice not all elderly patients with STEMI receive reperfusion therapy of any kind14.
This study sought to ascertain demographic details, procedural outcomes and in-hospital outcomes in consecutive patients aged ≥80 years undergoing contemporary PPCI. Comparison was made with those patients aged <80 years.
Methods
Royal North Shore Hospital, Sydney, Australia, serves as the centre of a regional STEMI system offering 24-hour PPCI covering a population of approximately one million people. When a patient with STEMI is identified in an emergency department, the interventional team is activated and the patient is transported directly to the PCI centre. In addition, since April 2004 the hospital has also pioneered a field triage system where patients with chest pain are assessed in the community by emergency response teams15. STEMI patients are identified in this manner and transported directly to the cardiac catheterisation laboratory.
The details of all patients undergoing emergent cardiac catheterisation and PCI through the above channels are prospectively collated on a computerised database. The database was initiated in mid 2005 and maintained by research nurses employed specifically for this purpose. Using this database, all patients with STEMI undergoing PPCI from September 2005 until July 2011 were identified. In order to standardise inclusion criteria only patients with ST elevation or new onset left bundle branch block (LBBB) on the electrocardiogram (ECG), undergoing PPCI were included. Patients with ST-segment elevation on the ECG subsequently seen to have non-obstructive coronary disease due to conditions such as myopericarditis or Tako-tsubo cardiomyopathy were excluded. Patients undergoing rescue PCI were excluded. In addition, patients who necessitated emergent PCI who did not have ST elevation on the ECG, or who had initially non-diagnostic electrocardiograms were excluded.
Using the patient cohort identified, demographic, procedural, detailed time to treatment data, laboratory data, coronary angiographic findings, and in-hospital morbidity and mortality data were assessed. All cause mortality was collated. PCI success was defined as TIMI 2/3 flow in the culprit artery at the end of the procedure. Acute kidney injury was defined as a rise in serum creatinine of ≥50% within the first seven days following PPCI. Comparison was made between those aged <80 years and those aged ≥80 years. Assessment for predictors of in-patient mortality was performed using stepwise multivariate regression.
Unless otherwise stated, continuous data were presented as mean±SD and skewed continuous data were presented as median and interquartile range (IQR). An independent t-test was used for comparison of means. A Fisher’s exact test was utilised for comparison of categorical variables. The value p<0.05 was considered as statistically significant.
Results
In the study period 2,088 patients within the primary PCI catchment area underwent emergent cardiac catheterisation. Of these 357 had ST-segment depression on the ECG, 77 had t-wave inversion and 112 had a normal ECG. There were 74 cases of presumed new onset bundle branch block with subsequent normal or non-obstructed coronary arteries. There were 191 patients who had ST-segment elevation on the ECG but did not undergo PPCI due to no culprit artery being identified, spontaneously recanalised coronary arteries and deferred revascularisation, or conditions such as Takotsubo cardiomyopathy, pericarditis or myopericarditis. A total of 1,277 patients were identified with STEMI requiring emergency revascularisation with 59 being referred for emergency coronary artery bypass grafting. The remaining 1,218 patients underwent PPCI.
AGE DISTRIBUTION OF PATIENTS
The age ranges of the remaining 1,218 patients are identified in Figure 1. With respect to the pre-defined categories, 994 (81.6%) were aged <80 years and 224 (18.4%) were aged ≥80 years.
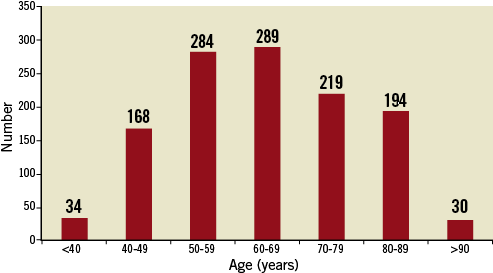
Figure 1. Age distribution of patients treated with PPCI in the study period.
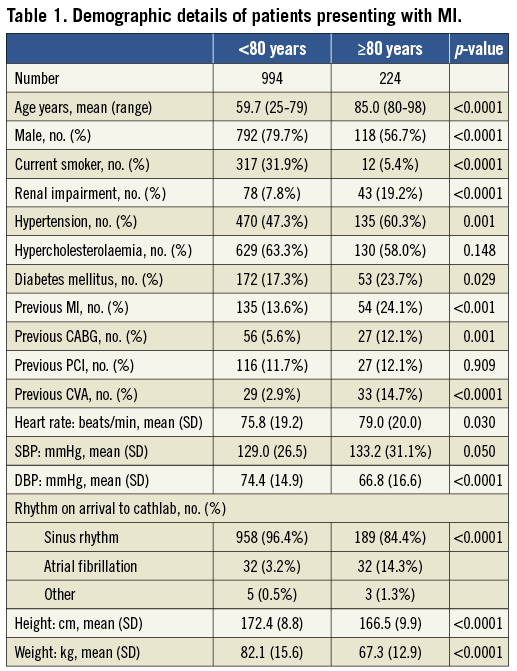
DEMOGRAPHIC DETAILS OF PATIENTS
Demographic details are identified in Table 1. Those aged ≥80 years were more likely to be female (43.3% vs. 20.3%; p< 0.0001) and have a history of hypertension. There were also significantly higher incidences of diabetes (23.7% vs. 17.3%), previous myocardial infarction (24.1% vs. 13.6%), previous renal impairment (19.2% vs. 7.8%), previous coronary artery bypass graft (CABG) (12.1% vs. 5.6%) and previous cardiovascular accident/transient ischaemic attack (CVA/TIA) (14.7% vs. 2.9%) in the elderly cohort. The elderly cohort had significantly lower weights and heights than those <80 years, related to the higher percentage of male patients in the younger cohort.
PROCEDURAL AND OUTCOME DATA
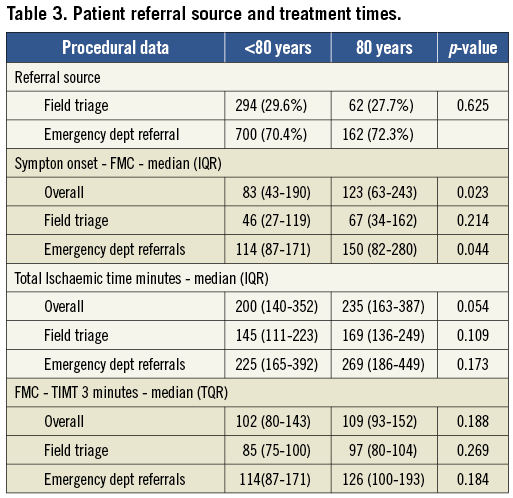
Procedural related data are detailed in Table 2. Referral sources were comparable between the two groups with approximately 70% derived from emergency departments and 30% from field triage directly to the cardiac catheterisation laboratory. The infarct-related artery was comparable between the groups, as was the median number of stents used (one in each group) and the stent type. The elderly cohort were less likely to have single vessel disease than those <80 years (43.3% vs. 52.4 %; p=0.015), but there was no difference between the requirement for intra-aortic balloon pump (IABP) (0.9% ≥80 years, 2.6% <80 years; p=0.143) or intubation (6.3% ≥80 years, 7.6% <80 years; p=0.572). Those aged ≥80 years were more likely than the younger cohort to be in cardiogenic shock on arrival at the cardiac catheterisation lab (13.4% vs. 7.6%; p=0.008).
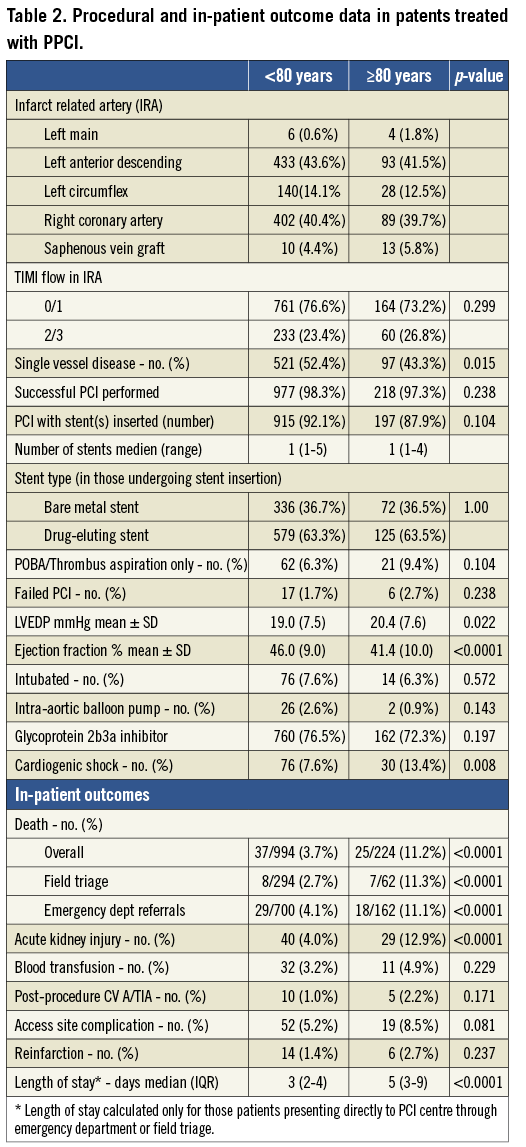
Symptom onset to FMC was significantly longer in the elderly cohort in the emergency department cohort and overall. However total ischaemic time (i.e., time from symptom onset to TIMI 3 flow in the culprit artery) and first medical contact to TIMI 3 flow (FMC-TIMI 3) were not statistically different between the groups, regardless of the mode of referral. In all parameters, however, there was a non-significant trend towards elderly patients having longer ischaemic times and FMC-TIMI 3 times. Field triaged patients in both cohorts had significantly shorter total ischaemic times and FMC-TIMI 3 than those presenting at emergency departments (Table 3).
Rates of PCI failure (i.e., TIMI flow <2 at end of procedure) were very low in both groups (≥80 years: 2.7%, <80 years: 1.7%; p=0.238). A larger percentage of the elderly cohort was managed with balloon angioplasty/thrombus aspiration without subsequent stent implantation (≥80 years: 9.4%, <80 years: 6.3%; p=0.104).
Despite the similarities in the procedural data, outcomes were significantly worse in those aged ≥80 years. The elderly group had lower ejection fractions when compared with those <80 years (41.4% vs. 46.0%; p<0.0001) though this may reflect the higher incidence of previous myocardial infarction. In-patient mortality rates in the elderly however were almost three times that of the younger cohort (11.2% vs. 3.7%; p<0.0001). There was also a significantly higher incidence of post-procedure acute kidney injury (defined as a >50% increase in serum creatinine) in the elderly cohort (12.9% vs. 4.0%; p<0.0001) and a non-significant trend towards more major and minor access site complications (8.5% vs. 5.2%; p=0.081) (Table 2, Figure 2).
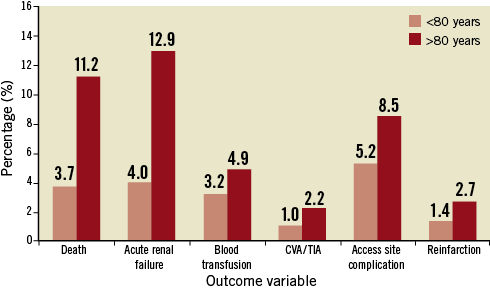
Figure 2. In-patient morbidity and mortality following PPCI for STEMI.
Comparing mortality rates between the groups, depending on referral source, revealed a lower mortality rate in those <80 years if they had been field triaged directly to the cardiac catheterisation laboratory (2.7%) as opposed to attending their local emergency department (4.1%). This reduced death rate associated with field triage was not seen in the elderly group with comparable mortality rates irrespective of the referral source (11.3% field triage vs. 11.1% emergency department).
The length of stay was assessed in those who presented directly at Royal North Shore Hospital, either through the emergency department or through the field triage system. Those aged ≥80 years had significantly longer lengths of stay when compared with the younger cohort of patients (median stay 5 vs. 3 days; p<0.0001).
PREDICTORS OF IN-PATIENT MORTALITY
Stepwise multivariate regression was performed to assess for independent predictors of in-patient mortality. Included in the model was gender, age ≥80 years, body mass index, hypertension, hypercholesterolaemia, smoking history, diabetes mellitus, previous myocardial infarction (MI), previous revascularisation, previous CVA, heart rate, initial blood pressure, total ischaemic times, multivessel disease, PCI failure, cardiogenic shock, reinfarction, periprocedural CVA and acute kidney injury.
Cardiogenic shock was the strongest predictor of in-patient mortality, though age ≥80 years, PCI failure, reinfarction and acute kidney injury were also identified as independent variables predicting death (Table 4).
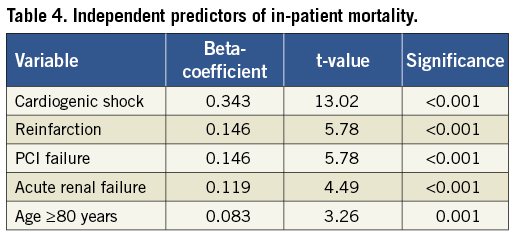
Patients aged ≥80 years presenting with cardiogenic shock had an in-patient mortality of 50.0%. Patients aged <80 years presenting without cardiogenic shock had an in-patient mortality of 1.6%.
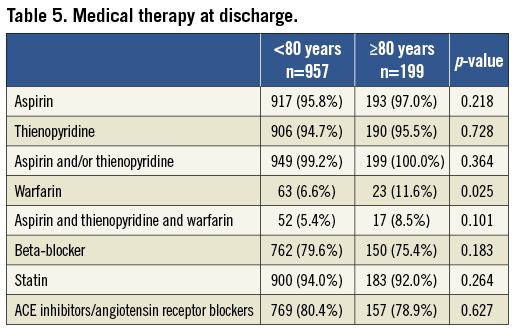
MEDICAL THERAPY AT DISCHARGE
Secondary prevention medications at discharge were comparable between the two groups (Table 5). All (100%) of the elderly cohort who survived to discharge (n=199), and 99.2% of the 957 patients <80 years who survived to discharge were on aspirin and/or a thienopyridine. Approximately 80% of each patient cohort were on an angiotensin converting enzyme (ACE) inhibitor/angiotensin receptor blocker and over 90% were on a statin. Use of beta-blockers were also comparable between the two groups (≥80 years: 75.4%, <80 years: 79.6%; p=0.183). A significantly larger percentage of elderly patients were on oral anticoagulation therapy at discharge compared with those <80 years (11.6% vs. 6.6%; p=0.025). In both cohorts a minority of patients were discharged on warfarin, aspirin and thienopyridine (triple therapy). In those <80 years, 5.4% of all patients were on triple therapy at discharge compared with 8.5% of those ≥80 years. Seventy-four percent of those ≥80 years discharged on warfarin were on triple therapy compared with 82% of the younger cohort.
Discussion
The ageing population will ensure that elderly patients presenting with STEMI will become increasingly common in the future. In our centre, 18% of all PPCI was performed on patients aged ≥80 years, a figure comparable to the total number of patients presenting aged younger than 50 years.
The most notable difference between the two cohorts was the in-hospital outcome between the two groups, with those aged ≥80 years having an in-patient mortality rate almost three times that of the younger cohort. Although mortality rates were higher in the elderly cohort, the rates of death compare favourably with previous studies performed in the late 1990s in assessing PPCI in the elderly in which 30-day mortality rates of 16-30% were recorded16,17. This improved outcome likely reflects modern PPCI practice and compliments more recent outcome data in elderly cohorts, with mortality rates in studies dating from 2007 and later ranging from 7.6-16% in those aged 75 years or older and 18.6% in those aged ≥85 years14,18,19. The improvement in mortality rates since the late 1990’s likely reflects contemporary practice at Royal North Shore Hospital with higher rates of use of thienopyridines, glycoprotein IIb IIIa inhibitors and routine thrombus aspiration along with a more streamlined STEMI service resulting in shorter ischaemic times20-22.
Important differences exist in the demographics of elderly patients presenting with STEMI compared with the younger cohort. Approximately half of the elderly patients in this study were female compared with 20% in those aged <80 years. They also had increased rates of significant pre-existing conditions such as diabetes, hypertension, previous myocardial infarction, previous revascularisation procedures, previous CVA and a history of renal impairment. The elderly cohort also had a higher incidence of cardiogenic shock on arrival to the catheterisation lab. This factor in particular, in addition to advanced age, was associated with worse in-patient outcomes observed in the elderly cohort.
It is interesting to note that field triage did not result in a reduced mortality rate in the elderly cohort as was demonstrated in those <80 years. In this cohort symptom onset - FMC was significantly longer when compared with those <80 years, though total ischaemic times were comparable. One explanation for the comparable death rates between ED and field triage could be that the assessment of pain onset is less precise in the elderly in general and may be even more subject to imprecision in field triage. Another possible reason for this finding however is the low number of mortality cases in the elderly field triage cohort (n=7), compromising the validity of statistical analysis. A third explanation is the mode of referral. Field triage is performed by a paramedical crew who electronically transmit the ECG to medical staff in the regional infarct centre. A decision whether to transfer directly to the cardiac catheterisation laboratory is made dependent on a doctor reviewing the ECG and no physician assessment of the patient is performed prior to arrival. This results in highly unselected patients with STEMI arriving for PPCI via the field triage system based largely on the ECG. This system contrasts with the emergency department referral process were an ECG forms part of an immediate assessment of the patient by an emergency physician. It is probable that certain elderly patients with STEMI are not referred for PPCI by emergency physicians based on significant comorbidities. This filtering system does not apply in the field triage system to the same degree and this may explain the lack of difference in mortality rates noted in our analysis. It has previously been shown that field triage reduces total ischaemic times, reduces infarct size and improves mortality rates15 and there is no reason to suggest that this improvement in mortality would not apply to the elderly population.
Our data demonstrates that PPCI in the elderly is technically feasible and rates of PCI failure are not more common in the elderly cohort. Furthermore, elderly patients do not require more stents than those aged <80 years though treatment with plain old balloon angioplasty (POBA)/thrombus aspiration alone is more common. The reasons why elderly patients had a higher incidence of balloon angioplasty/thrombus aspiration alone without stent implantation may be multifactorial. Embolic myocardial infarction is often due to atrial fibrillation (AF), with the prevalence of AF and thromboembolic risk associated with the arrhythmia increasing with advancing age. The elderly cohort was significantly more likely to be in atrial fibrillation on arrival at the cathlab. In addition, the elderly cohort also had higher rates of hypertension, diabetes and previous stroke. Consequently it is possible that elderly patients may have had a higher incidence of embolic MI without underlying obstructive coronary artery disease, therefore not requiring subsequent stent implantation. Another possible reason for higher rates of PCI without stent implantation in the elderly cohort may have been a more conservative percutaneous approach employed by the interventional cardiologists when dealing with those aged ≥80 years.
Although symptom onset –FMC was significantly longer in the elderly cohort, total ischaemic times, and time from first medical contact to TIMI 3 flow (FMC-TIMI 3) are comparable in the two groups. A total ischaemic time of approximately three to four hours and a FMC-TIMI 3 time of approximately one and a half to two hours were similar regardless of the age of the patients and suggest that PPCI activation within the Royal North Shore Hospital regional STEMI system of care is not influenced by the patient age. This finding compliments a recent study which showed only very minor increased transfer times and treatment times with increasing age, largely driven by elderly patients waiting longer with ischaemic symptoms14.
The high use of proven secondary prevention medications in the elderly cohort is a positive finding in this study, with early institution of beta-blockers and ACE inhibitors shown to improve outcomes in the elderly population post myocardial infarction21. The comparable rates of use of beta-blockers, ACE inhibitors and statins between the two groups demonstrate that it is possible to institute secondary prevention medications in those ≥80 years old. Drug intolerance due to bradycardia, hypotension or idiosyncratic reactions did not appear to be more common in the elderly cohort post myocardial infarction. No comments can be made on compliance and tolerance of secondary prevention medications in the patient groups following discharge; though it is known that long-term compliance with these prognostically important drugs are suboptimal in a wide variety of patients23,24. The high rates of antiplatelet medication at discharge reflect the high use of stents in this patient cohort, with dual antiplatelets being essential to avoid stent thrombosis. Triple therapy with dual antiplatelet medications along with warfarin was more common in the elderly population reflecting the higher rates of atrial fibrillation with associated hypertension and previous CVA in the elderly groups. Although triple therapy carries a higher risk of bleeding, recent guidelines validate its use in certain high-risk groups such as elderly patients with atrial fibrillation and recent stent implantation25,26.
It is also noteworthy that elderly patients had longer median in-hospital stays compared with the younger cohort. This likely reflects the increased morbidity rates of acute kidney injury, major and minor access site complications, etc., seen in the elderly. Although the majority of PPCI at Royal North Shore Hospital is now currently performed via the radial artery, most patients in this study will have had femoral arterial access during their procedure. Recent data suggests that a default radial artery access for STEMI may improve outcomes compared with the femoral artery and it is possible that this may represent a future area where morbidity and mortality rates may be improved, with associated shorter in-patient stays27. It is important to note that our study reports clinical outcomes in elderly patients undergoing pPCI, but we have not addressed the cost effectiveness of this procedure.
Limitations
There are limitations inherent in this study. The study is retrospective and it is arguable that prospectively collated data may be more dependable. However, although the study is retrospective the data entry into our database was performed prospectively and maintained by specially-appointed, trained staff. The data recorded is therefore robust and reliable.
Certain data was not recorded which may have influenced outcomes between the two groups. Pre-procedure anti-platelet therapy (i.e., aspirin/clopidogrel, etc.) was not recorded in our database and we cannot be sure the treatments were homogenous. In addition the exact incidence of thrombus aspiration and the arterial access site were not recorded prospectively and unrecognised heterogeneity in these factors may have influenced outcomes. Frailty index was not assessed in our cohort, and this may have identified a further independent predictor of mortality28.
Our study assessed only in-patient mortality. It is likely that the attrition rate in the elderly cohort at 30 days or one year continued to increase at a higher rate relative to the younger patient group, and our data will not have identified this pattern.
The question of selection bias is an important one. It is clear from other studies that not all elderly patients with acute STEMI either receive thrombolysis or are referred to specialist centres for percutaneous revascularisation14. It is highly probable that in the study period a cohort of patients aged ≥80 years attended emergency departments within the catchment area with acute STEMI, but were not referred for PPCI on the basis of significant comorbidities such as dementia or significant lung disease. Therefore the quoted periprocedural data, morbidity and mortality rates in this study may reflect relatively healthy older adults and may not be universally applicable to all patients ≥80 years old.
Another possible limitation is that the study comprises data from a single PCI centre and may not reflect outcome data from other infarct centres. However, the analysis involves over 1,200 patients and is novel in that it reports experience of STEMI patients ≥80 years treated within a regional STEMI system.
Conclusion
In the coming decades it is inevitable that patients aged ≥80 years presenting with STEMI will become increasingly common. This study demonstrates that PPCI is efficacious and safe in this high-risk subgroup, with procedural outcomes comparable to younger patients. Although in-patient mortality remains high compared with younger patients, contemporary PPCI practice, along with a streamlined STEMI network has resulted in lower mortality rates when compared with historical data. A wider use of field triage systems for identifying STEMI along with default radial artery access represent two areas where outcomes may be improved further. PPCI should now be routinely offered to all suitable patients presenting with STEMI, regardless of age.
Acknowledgements
The authors would like to acknowledge the work of Annie Loxton and Soon Yeng Soo Hoo, whose tireless commitment to the Royal North Shore Hospital STEMI database made this article possible.
Conflict of interest statement
The authors have no conflicts of interest to declare.

