Abstract
Aims: The aim of this study was to assess the performance of a self-expanding valve in bicuspid aortic valve (BAV) stenosis.
Methods and results: An international registry included a total of 712 patients with aortic stenosis treated with the ACURATE neo in bicuspid (n=54; 7.5%) or tricuspid (n=658; 92.4%) anatomy. The overall mean age was 81±5.6 years. At baseline, no significant differences were found between the two groups. BAV more frequently required both predilatation (94.4% vs. 78.1%, p=0.004) and post-dilation (57.4% vs. 38.7%, p=0.007). Moderate perivalvular regurgitation was more frequently found in patients with BAV (7.4% vs. 3.18%, p=0.0001). After propensity score matching (PSM), the rate of predilation and post-dilation was confirmed to be higher in the BAV group (94.4% vs. 66.6%, p=0.001, and 57.4% vs. 37.1%, p=0.034, respectively), while the incidence of moderate perivalvular regurgitation was similar between the two groups (BAV 3.1% vs. 5.5% in tricuspid anatomy, p=0.734). In unmatched cohorts, the 30-day outcome showed a higher rate of stroke in the BAV group (7.4% vs. 1.8%, p=0.001). After adjustment for PSM quintiles, the rate of stroke resulted in being similar (odds ratioadj 1.20, 95% confidence interval [CI]: 0.81-1.76, p=0.819). The other 30-day clinical endpoints were similar between the two populations.
Conclusions: This preliminary analysis shows that the use of the ACURATE neo in bicuspid aortic valves is feasible and has acceptable 30-day outcomes. Larger studies are needed to confirm our preliminary findings.
Abbreviations
AS: aortic stenosis
BAV: bicuspid aortic valve
CI: confidence interval
CT: computed tomography
OR: odds ratio
PSM: propensity score matching
STS: Society of Thoracic Surgeons
TAV: tricuspid aortic valve
TAVI: transcatheter aortic valve implantation
TF: transfemoral
VARC: Valve Academic Research Consortium
Introduction
Transcatheter aortic valve implantation (TAVI) represents a valid therapeutic alternative to surgical aortic valve replacement for intermediate- and high-risk patients with symptomatic severe aortic valve stenosis (AS)1,2. However, in all randomised clinical trials evaluating TAVI, congenital bicuspid aortic valves have been excluded. Therefore, because of the lack of clinical data in this patient subset, TAVI in bicuspid aortic valve (BAV) disease is currently off-label. However, data from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry showed that the use of a balloon-expandable valve might be a possible therapeutic option to treat BAV disease3. The aim of our study was to compare the procedural and 30-day outcome of the ACURATE neo™ (Boston Scientific, Marlborough, MA, USA) in BAV and in tricuspid aortic valve (TAV) anatomy.
Methods
The ACURATE neo implantation in bicuspid aortic valve registry is an international registry including all patients treated for AS in BAV and TAV anatomy using the ACURATE neo system in seven different European centres. BAV morphology was classified according to Sievers et al4 considering the number of cusps and the presence of raphes. All participating centres reviewed and subsequently confirmed the diagnosis and classification of BAV. Patients were not included in the BAV group if the diagnosis of bicuspid anatomy was not consistent or remained non-conclusive.
STUDY DEVICE
The ACURATE neo system used in our population consists of a self-expanding nitinol stent with an anatomic conformability to the native annular shape. Stabilisation arches are designed to pivot against the ascending aorta for self-alignment of the prosthesis. The upper crown allows supra-annular anchoring, stable positioning and tactile feedback. The ACURATE neo transapical (TA) valve is made of three non-coronary native porcine leaflets5, while the ACURATE neo transfemoral (TF) valve is made of porcine pericardial tissue with BioFix™ anticalcification treatment6. The ACURATE neo TF is a supra-annular valve whose delivery system is compatible with 15 Fr balloon-expandable and 18 Fr rigid sheaths7.
STUDY PROCEDURE
The decision to perform TAVI was based on the severity of symptoms, risk evaluation and contraindications to surgery. All patients were evaluated by a multidisciplinary Heart Team comprising a cardiologist, interventional cardiologist, cardiothoracic surgeon, and cardiac anaesthetist. Patient demographics, symptoms, and comorbidities were documented, and individual risk was assessed with the logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) and the Society of Thoracic Surgeons (STS) score. All patients with severe AS considered for an intervention underwent computed tomography (CT) to evaluate annular size, coronary arteries and peripheral access sites. The standard access route was the TF approach; the TA route was considered whenever the TF approach was found to be inappropriate by the Heart Team. The sizing of the valve and the implantation technique were left to the operator’s decision. However, in the presence of BAV, the authors suggested a higher implant of the valve with the upper crown positioned above the virtual basal ring because the supra-annular structure may serve a key role in anchoring the transcatheter valve. The clinical status of the patients, electrocardiogram (ECG) and echocardiogram as well as any new rehospitalisation or valve-related event were adjudicated by each centre and the data were recorded in a dedicated spreadsheet.
STUDY OBJECTIVES AND DEFINITIONS
The primary objective of the present study was device success. Secondary objectives were 30-day major clinical endpoints using the Valve Academic Research Consortium (VARC)-2 criteria8. Other endpoints included the need for permanent pacemaker implantation, procedure- and device-related complications and echocardiographic assessment of the valve and cardiac function at discharge. The severity of regurgitation was qualitatively assessed and graded using transthoracic echocardiography at each institution according to established guidelines9. Aortic valve calcifications were graded according to the criteria suggested by Tops et al10.
STATISTICAL ANALYSIS
Baseline categorical variables are presented as percentages and continuous variables as mean±standard deviation. Results are expressed as mean±standard deviation. The significance of variability among groups was determined by one-way or two-way ANOVA.
A propensity score matching (PSM) was performed using Stata, version 13.0 (StataCorp, College Station, TX, USA) to reduce imbalance in patient baseline characteristics and the effect of potential selection bias for comparing ACURATE valves in bicuspid and tricuspid anatomies. PSM was calculated for each patient to estimate the propensity towards belonging to a specific treatment group (tricuspid vs. bicuspid). This was carried out by means of a non-parsimonious multivariable logistic regression including the following covariates: age, sex, previous cardiac surgery, previous pacemaker or implantable cardioverter defibrillator, New York Heart Association (NYHA) functional Class III or IV, left ventricular ejection fraction (LVEF), Society of Thoracic Surgeons (STS) score, aortic valve calcifications. A one-to-one nearest neighbour matching algorithm without replacement was performed to identify propensity-matched pairs. The C-statistic was 0.72, indicating good discrimination for the PSM model.
Results
Between October 2012 and July 2017, a total of 54 patients with severe aortic stenosis of a bicuspid aortic valve were treated with ACURATE neo implantation in seven centres. During the same time period, a total of 658 TAVI procedures with the ACURATE neo were performed in three out of seven centres among patients with severe tricuspid aortic valve stenosis (Table 1). Our registry included a total of 712 patients with aortic stenosis treated with the ACURATE in the presence of either bicuspid (n=54%; 7.5%) or tricuspid (n=658; 92.4%) anatomy. The overall mean age was 81±5.6 years and 63.3% were female (n=453). The demographic features of the two populations are listed in Table 2. At baseline, no significant differences were found between the two groups. Similarly, echocardiographic and CT scan findings were similar between the tricuspid and bicuspid valve populations (Table 3). CT scans identified 49 patients (90.7%) with a type 1 bicuspid valve, two patients (3.7%) with a type 0 bicuspid valve and one case (1.8%) of a type 2 bicuspid valve (Table 3). A one-to-one PSM analysis resulted in a total of 54 matched pairs. As shown in Table 2 and Table 3, there was no significant difference in any baseline, CT scan or echocardiographic characteristics among the propensity score-matched groups, including the degrees of aortic valve calcification.
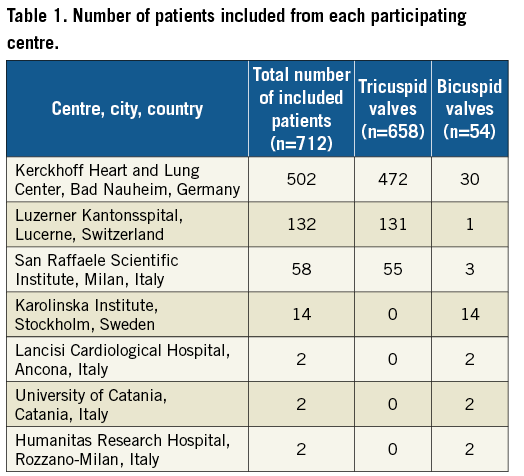
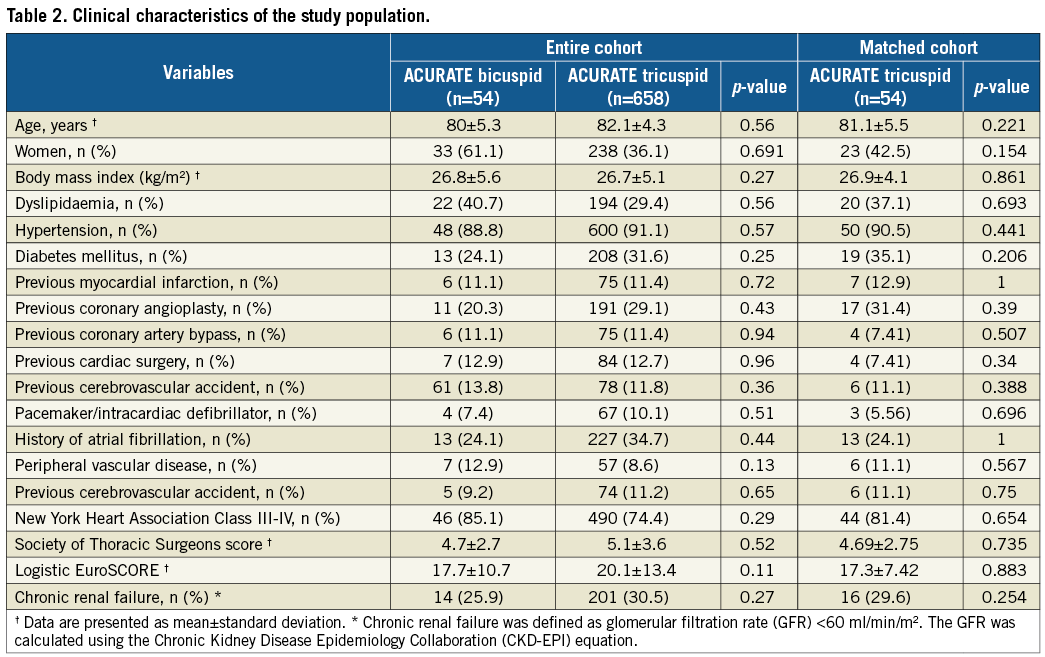
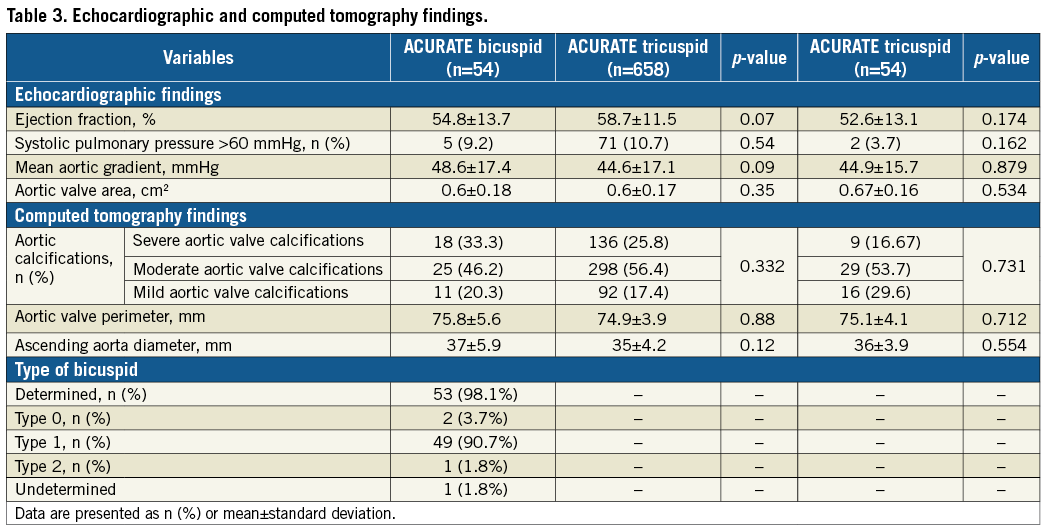
Table 4 summarises the procedural data. Bicuspid patients were less frequently implanted using the TF route (83.3% vs. 100%, p=0.001) and more frequently required both predilatation (94.4% vs. 78.1%, p=0.004) and post-dilation (57.4% vs. 38.7%, p=0.007) (Figure 1). Figure 2 shows the grade of perivalvular regurgitation in both the matched and unmatched populations. A moderate/more-than-moderate perivalvular regurgitation was more frequently found in patients with bicuspid valve anatomy (7.4% vs. 3.18%, p=0.0001). After PSM analysis, the rate of moderate perivalvular regurgitation was non-significant (7.4% BAV vs. 3.7% TAV, p=0.734) while the rate of predilation and post-dilation was confirmed as being higher in the bicuspid population (94.4% vs. 66.6%, p=0.001, and 57.4% vs. 37.1%, p=0.034, respectively) (Figure 1); the other variables were comparable between the two groups.
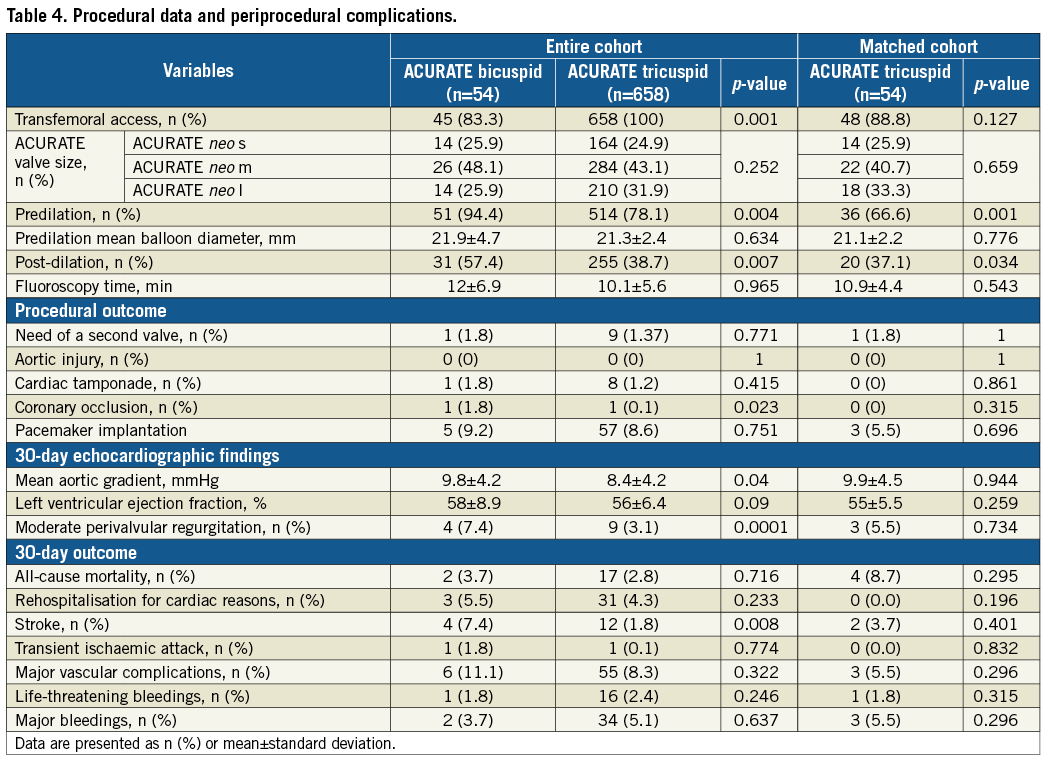
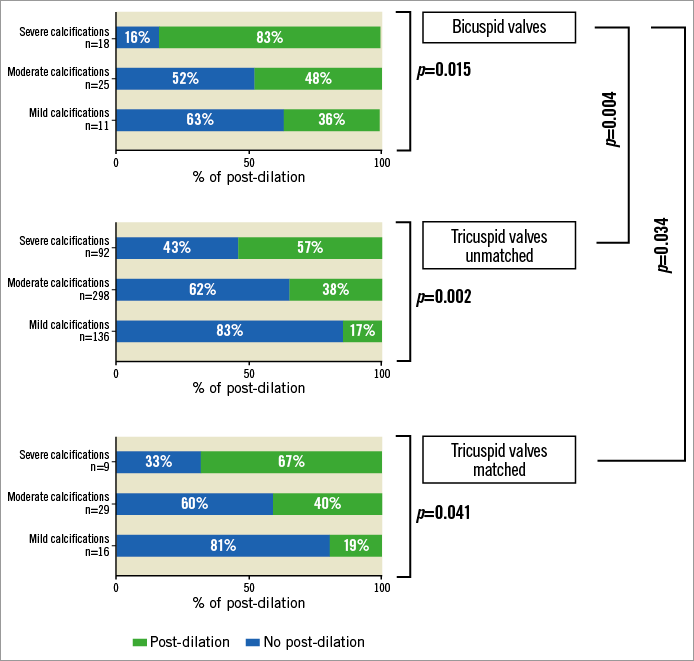
Figure 1. Post-dilatation according to the presence of mild, moderate or severe aortic calcifications.
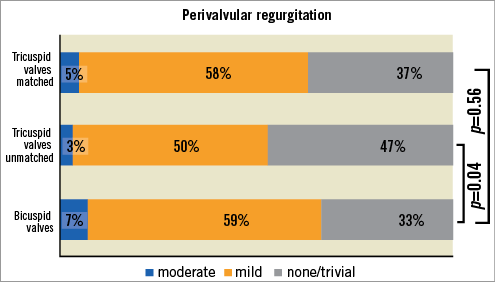
Figure 2. Perivalvular leak at 30-day follow-up.
At 30-day follow-up, a higher rate of stroke (7.4% vs. 1.82%, p=0.008) and higher gradients (9.8±4.2 vs. 8.4±4.2 mmHg, p=0.04) were observed in patients with bicuspid aortic valve anatomy. No differences were observed in the rate of pacemaker implantation (bicuspid 9.2% vs. tricuspid 8.6%, p=0.751). The rates of all-cause mortality, rehospitalisation for cardiovascular reasons, vascular complications and major bleedings were similar between the two populations.
After adjustment for PSM quintiles, the rates of stroke (odds ratio [OR]adj 1.20, 95% confidence interval [CI]: 0.81-1.76, p=0.819) and moderate perivalvular regurgitation (ORadj 0.92, 95% CI: 0.88-1.33, p=0.653) were similar between the two groups. The other outcome variables were similar at 30-day follow-up.
Discussion
The main findings of our multicentre experience are the following. 1) The implantation of the self-expanding ACURATE neo in BAV appears to be feasible; however, compared to TAV, BAV more frequently required predilation and post-dilation to achieve a satisfactory result. 2) The 30-day rate of moderate perivalvular leak was 7.4% in the BAV group, higher compared to the TAV group; however, the difference between the two groups became non-significant after PSM. 3) A higher rate of stroke was observed in the BAV cohort (7.4%) compared to TAV; even though this difference disappeared after PSM, further investigations are needed to address this finding.
The treatment of bicuspid valve disease still represents a challenge in the transcatheter treatment of AS due to its peculiar anatomical features: bicuspid AS is characterised by larger size, and an oval annular shape with two commissures that make the virtual basal ring identification more ambiguous. In 2014, Mylotte et al reported data from 139 bicuspid valve patients who underwent TAVI with first-generation devices. The study highlighted the complexity of performing TAVI in such patients, with high rates of malpositioning, use of multiple transcatheter heart valves and relatively high rates of moderate-to-severe residual aortic regurgitation11. Over the years, the implementation of transcatheter heart valve technology has allowed a progressive increase in procedural safety and efficacy. Data from Yoon et al showed the excellent safety and efficacy of the balloon-expandable valve (SAPIEN 3; Edwards Lifesciences, Irvine, CA, USA) and the LOTUS™ valve (Boston Scientific) in the presence of BAV disease. Among 91 patients treated with SAPIEN 3 and 11 patients using the LOTUS valve system, the authors reported a 0% rate of moderate perivalvular leaks at 30-day follow-up, and an overall rate of device success of 92.2% with a good safety profile in terms of annular rupture, which occurred in only one case12. More recent data have confirmed those findings, showing a good performance of both SAPIEN 3 and LOTUS in the treatment of BAV stenosis with similar outcome compared to those who received the same devices in tricuspid valves13.
Few data are available about the treatment of bicuspid AS with new-generation self-expanding valves. To date, and only recently, the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry has reported that the use of the CoreValve® Evolut™ (Medtronic, Minneapolis, MN, USA) is feasible and safe with 97.4% device success, 7.7% residual moderate perivalvular leak and 12.6% need for permanent pacemaker implantation at 30-day follow-up3.
To the best of our knowledge, no study has been published on the feasibility and safety of TAVI with ACURATE neo implantation in bicuspid AS. Our data show the feasibility and safety of the self-expanding ACURATE neo implant in this population, reporting a 7% rate of moderate perivalvular leak, and 9.2% rate of permanent pacemaker implantation. These data are in line with the use of ACURATE neo in the treatment of TAV7. However, in our cohort, the implantation of ACURATE neo in BAV seems to be more challenging compared to the tricuspid anatomy: we showed a higher rate of both predilation and post-dilation when this self-expanding valve needed to be implanted in bicuspid anatomy. We can speculate that the low radial force of the ACURATE neo requires a more meticulous preparation of the valve and that a final post-dilation is needed to achieve a good final result. Compared to the overall tricuspid cohort, the incidence of moderate final perivalvular regurgitation was higher among patients with bicuspid anatomy: even though the difference was not significant after PSM, this result needs to be confirmed in larger populations. Previous data described an increased risk of annular rupture in case of post-dilation in severely calcified bicuspid aortic valves14,15. However, in our experience no cases of annulus rupture and/or aortic dissection were reported except for one patient who had evidence of post-procedural ventricular septal defect which led to cardiac death during surgery due to extreme haemodynamic instability. The patient had mild valvular calcifications, underwent an aggressive predilation using a 22 mm balloon in an annulus of 22.4 mm and did not require post-dilatation.
Compared to other studies and to the unmatched TAV cohort, our experience reports a relatively high rate of stroke (n=4; 7.4%) among BAV16. Several different factors might have contributed to such a rate of cerebrovascular events. The neurological events occurred in a high-risk population (mean age 80 years with a prevalence of female patients, and 29.6% of patients with a previous history of atrial fibrillation). Both TIA and strokes occurred a few hours after the procedure, and therefore procedural factors such as high rates of predilation and post-dilation could have had an impact. Previous studies have reported that a high rate of manipulation during a TAVI procedure is associated with a higher rate of embolisation17. We cannot exclude that the high rate of predilation and post-dilation performed in our patients could have had a negative impact on the rate of neurological events observed. Furthermore, we cannot exclude that operator experience might have played an important role.
Limitations
The study was retrospective and non-randomised in design, making the results purely hypothesis-generating. In addition, the events were not adjudicated by a clinical events committee but by single centres, and the device and patient selection were left to the decision of the operator. Moreover, our study was limited by the lack of uniformity in the annular sizing; we cannot exclude that this limitation could have had an impact on the final results presented in this paper.
Conclusions
This multicentre experience reported that the use of the ACURATE neo in bicuspid anatomy has acceptable procedural and midterm results when compared with its use in TAV. Larger studies are needed to confirm our preliminary findings.
| Impact on daily practice This international experience increases the knowledge about the treatment of bicuspid valves with a self-expanding prosthesis, demonstrating the safety and feasibility of this transcatheter valve implantation. |
Conflict of interest statement
S. Toggweiler is a proctor and consultant for Boston Scientific and NVT GmbH and has received an institutional research grant from Boston Scientific. K. Won-Keun has received speaker fees from Symetis/Boston Scientific and Edwards, and is proctor for St. Jude Medical/Abbott and Boston Scientific. The other authors have no conflicts of interest to declare.