Abstract
Aims: Late stent thrombosis has been documented in on- and off-label populations. Stent thrombosis is more frequently in higher risk patients and there is still scarce data about the impact on late adverse cardiac events. The aim therefore is to determine the 3-year safety and effectiveness of Sirolimus-Eluting Stent (SES) (Cypher®) implantation in patients with multivessel disease and to compare outcomes with the historical results of the two arms of the Arterial Revascularisation Therapies Study (ARTS-I).
Methods and results: ARTS-II is a 45 centre, 607 patient single-arm study. Three years outcomes were compared to the outcome of the historical cohorts of ARTS-I using the same inclusion and exclusion criteria and major adverse cardiac and cerebrovascular events (MACCE) definitions. Patients were stratified by clinical site to ensure that at least 1/3 had 3-vessel disease to achieve a number of treated lesions per patient comparable to ARTS-I. Stent thrombosis was re-adjudicated using the ARC definitions. An angiographic coronary score to characterise lesion complexity was applied to allow the identification of patients who might benefit the most from multivessel stenting.
In ARTS-II, 46.6% of the patients underwent 3-vessel treatment as compared to 18.0% in ARTS-I percutaneous coronary intervention (PCI) (n=600) with bare metal stents (BMS). Diabetes was present in 26.2% in ARTS-II as compared to 17.3% in ARTS-I. In ARTS-II, patients received on average 3.7 stents resulting in a mean total stented length of 72.5 mm. The 3-year survival rate in ARTS-II was 97.0%, comparable to the 95.6% and 96.0% of the historical surgical (n=605) and PCI cohorts of ARTS-I. The death/cerebrovascular accident (CVA)/myocardial infarction (MI) event free survival rate in ARTS-II was 91.7%, versus 89.1% (p=0.1) and 87.2% (p=0.007) in ARTS-I coronary artery bypass graft (CABG) and PCI cohorts, respectively. Freedom from revascularisation in ARTS-II was 85.5%, lower than in ARTS-I CABG (93.4%; p<0.001) but higher than in ARTS-I PCI (73.7%; p<0.001) cohorts. MACCE free survival was 80.6% in ARTS-II, comparable to ARTS-I CABG (83.8%; p=0.21) but superior to ARTS-I PCI (66.0%; p<0.0001). The incidence of stent thrombosis (ARC any) in ART-II was 6.4% (39/607 patients).
Conclusions: Despite the higher clinical and angiographic risk profile, the overall MACCE rate at three years was lower in ARTS-II than in the ARTS-I PCI and comparable to ARTS-I CABG. However, the re-intervention rate in ARTS-I CABG remained significantly lower than in ARTS-II.
Introduction
In September 2001, the results of the pivotal randomised trial comparing bare metal stents (BMS) and sirolimus-eluting stents (SES) were presented at the scientific sessions of the European Society of Cardiology and subsequently published in 2002.1 Shortly after the commercialisation of this first drug-eluting stent (Cypher®) in Europe in April 2002, European investigators requested the manufacturer to sponsor a randomised comparison between bypass surgery and stenting with SES for multivessel disease, using a similar study design as in the Arterial Revascularisation Therapies Study ARTS-I.2-4 However, the project was considered to be premature, hazardous and expensive. As a surrogate, the ARTS-II registry was designed applying the same inclusion and exclusion criteria, the same protocol definitions and the same primary endpoint, in order to make the registry as comparable as possible to the randomised ARTS-I trial of coronary artery bypass surgery and BMS.5
Despite the non-randomized nature of the ARTS-II trial, the 3-year results can be interpreted today in the context of the current concerns raised about the long-term safety of SES, since the ARTS-II population is so far one of the most complex populations of patient treated with SES.
Since the first seminal observation of very late stent thrombosis, a large number of reports have raised concerns about the safety of the treatment, particularly in off-label use.6-10 ARTS-II clearly represents “off-label” use of SES with an average use of 3.7 stents per patients resulting for a mean total stented length of 72.5 mm per patient, a length of stenting unparalleled by any randomised trial or current registry reported thus far. In the meantime, the Academic Research Consortium (ARC), working with the FDA and major stent manufacturers, created new definitions for the major adverse clinical events, including stent thrombosis.11
In October 2006 the FDA requested that the events in the pivotal Cypher and Taxus trials be re-adjudicated using these definitions.12-15 In ARTS-II, events were re-adjudicated by a new independent critical event committee, focusing on the incidence and timing of stent thrombosis.
The present study reports on the 3-year safety and effectiveness of the SES in patients with multivessel disease compared to the outcomes of the historical results of the two arms of ARTS-I applying the ARC definition to determine the incidence of definite, probable or possible stent thrombosis.
Methods
Study design
ARTS-II is a multicentre, non-randomised, open-label trial, designed to compare the safety and efficacy of the SES in patients with de novo multivessel coronary artery disease with the surgical group of ARTS-I acting as a historical control.5 In order to obtain a population comparable to ARTS-I, patients were stratified by clinical site in order to ensure the inclusion of at least 1/3 of patients with three-vessel disease.
Patient selection
Patients were eligible for coronary revascularisations if they had either stable angina (Canadian Cardiovascular Society class I-IV), unstable angina (Braunwald class I-III B or C), or if they had silent ischaemia and at least two lesions located in different major epicardial vessels and/or their side branches (not including the left main coronary artery) that were potentially amenable to stent implantation.16,17 Patients were required to have multivessel disease including treatment of the left anterior descending (LAD) artery and at least one other significant lesion (>50% diameter stenosis) in another major epicardial coronary artery. The goal was to achieve complete anatomic revascularisation.18 One totally occluded major epicardial vessel or side branch could be included. The stenosis had to be amenable to stenting using a SES with a diameter of 2.5 to 3.5 mm and length of 13 to 33 mm, without restriction on the total implanted stent length. Decisions to place stents in lesions with bifurcations, fresh thrombus, calcification, diffuse disease, complex anatomy or stenting of side branches were left to the discretion of the operators.
Patients with previous coronary intervention, left main coronary disease, overt congestive heart failure or a left ventricular ejection fraction of less than 30 percent were excluded. Additional exclusion criteria were: history of a cerebrovascular accident, transmural myocardial infarction in the preceding week, severe hepatic or renal disease, neutropenia or thrombocytopenia, an intolerance or contraindication to acetylsalicylic acid or thienopyridines, the need for concomitant major surgery and life-limiting major concomitant non-cardiac diseases. Written, informed consent was obtained from each patient prior to enrolment. The study was approved by the ethics committee of each participating site.
Study objectives
The primary objective of ARTS-II was to compare the safety and effectiveness of coronary stent implantation using the SES with the surgical arm of ARTS-I.19,20 Endpoints are measured in terms of major adverse cardiac and cerebrovascular events (MACCE) comprising all-cause death, any cerebrovascular event, non-fatal MI, or any repeat revascularisation.
The secondary objectives of this study were to compare the ARTS-II patients to both arms of ARTS-I with respect to MACCE at 30 days, one, three and five years; the composite end point death, CVA and myocardial infarction, and the itemised outcomes death, CVA, myocardial infarction and repeat revascularisation; resource utilisation at 30 days and one year; cost effectiveness at one year, and quality of life at six months, and one, three and five years.21 Finally, the study aimed at describing the prognostic value of the Syntax score on the MACCE rates in the ARTS-II population.
Endpoint definitions
Death was categorised as cardiac or non-cardiac. Cerebrovascular events were divided into three main categories: stroke, transient ischaemic attacks, and reversible ischaemic neurologic deficits. In the first seven days after the intervention, a definite diagnosis of myocardial infarction was made if there was documentation of new abnormal Q-waves and either a ratio of serum creatine kinase MB (CK-MB) isoenzyme to total cardiac enzyme that was greater than 0.1 or a CK-MB value that was five times the upper limit of normal22 Serum creatine kinase and CK-MB isoenzyme concentrations were measured six, 12, and 18 hours after the intervention. Commencing eight days after the intervention (the length of the hospital stay after surgery), either abnormal Q waves or enzymatic changes, as described above, were sufficient for a diagnosis of myocardial infarction. A myocardial infarction was confirmed only after the relevant electrocardiograms had been analysed by the core laboratory and adjudicated by the clinical-events committee. This two-part method of defining myocardial infarction was developed for ARTS-I to address the difficulty of diagnosing a myocardial infarction after cardiac surgery.5 These definitions have been adopted by the ARC Consortium and are applied whenever a comparison between DES and surgery is performed.11 In the final report, the window of seven days is not specifically mentioned and this window has been maintained for the sake of comparison with the historical data from ARTS-I. All repeat revascularisation procedures were recorded.
Secondary measures of efficacy were assessed by means of the EQ-5D questionnaire, which allows patients to grade their general health status.23
Endpoint measurement
In ARTS-II, the interventional procedure was performed within 48 hours of inclusion, while in ARTS-I patients were randomised after informed consent had been obtained and then entered a waiting list, with three deaths in the ARTS-I CABG arm occurring whilst patients were awaiting revascularisation. To compensate for the temporal difference since allocation between groups, events for the present report were counted from the time of the procedure for all three arms and not from the time of allocation as previously published.3,4,24
In ARTS-I and ARTS-II, only data on subacute thrombotic occlusion (<30 days) were collected in the case record form (CRF). In ARTS-II, stent thrombosis was re-adjudicated according to the ARC definitions.11 In this process, all coronary angiograms, both procedure-related (n=104) and non-procedure related (n=165) were reviewed by an independent core laboratory and adjudicated by an independent critical event committee. Thus far, no attempt has been made to assess data on stent thrombosis in ARTS-I in a similar fashion.
In addition, a detailed coronary risk score which had been previously published and tested in a subgroup of ARTS-II patients with 3-vessel disease (the Syntax score) was used to characterise the complexity of the coronary anatomy.25,26 In brief, each coronary lesion producing > 50% luminal obstruction lumen in vessels > 1.5 mm was separately scored and added to provide the overall Syntax. The Syntax score was calculated using a dedicated software that integrates the number of lesions with their specific weighting factors based on the amount of myocardium distal to the lesion according to the score of Leaman et al,27 and the morphologic features of each single lesion, as previously reported26 (available at http://www.europcronline.com/eurointervention/2nd_issue/36/). This Syntax score is now available for the entire ARTS-II population and its implications in terms of prognosis at three years are reported in the present document.
Statistical analysis
The sample size justification was based on the comparison of 1-year MACCE rates in the ARTS-II patients and the ARTS-I surgery patients for the primary endpoint. A MACCE-free survival rate of 90.9% was assumed in the ARTS-II trial, requiring a sample size of 600 patients to guarantee a power of at least 90%.5,20 Binary variables are reported as percentages, and the difference between groups was presented with 95% confidence intervals. Time-to-event variables are presented as Kaplan-Meier curves and incidences were compared using the log-rank test. Safety data up to three years are presented as Kaplan-Meier estimates, with relative risks and 95% confidence intervals. The final analyses will be performed at five years.
A separate multivariate regression analysis was performed to determine independent predictors of MACCE and ST within the ARTS-II population only. Baseline and procedural characteristics listed in Table 1 were tested on a per patient basis by univariate analysis to determine suitability for inclusion in the multivariate model. Finally, a logistic regression model was built using the significant univariate predictors (p<0.1).
Results
Baseline and procedural characteristics
Between April 1997 and June 1998 a total of 1,205 patients were randomly assigned to PCI with BMS (n=600) or CABG (n=605) in 67 participating centres in the ARTS-I trial. Between February 2003 and November 2003, 607 patients at 45 participating centres were treated (Figure 1).
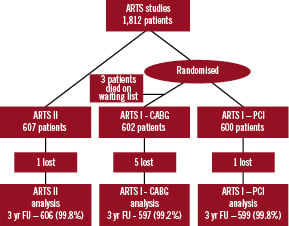
Figure 1. Flowchart of ARTS-I and ARTS-II.
Table 1 presents their baseline demographic and angiographic characteristics.
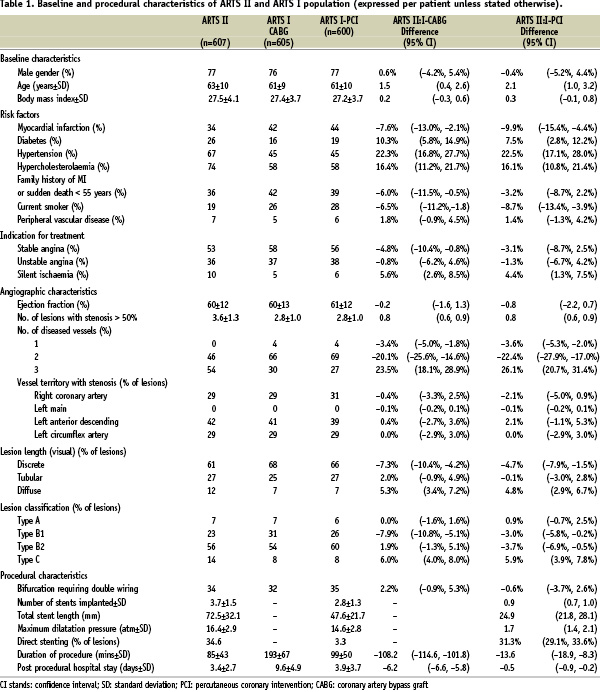
Patients treated in ARTS-II were significantly older than those in ARTS-I. ARTS-II had a significantly higher incidence of diabetes mellitus, hypertension, hypercholesterolaemia and silent ischaemia, and a lower percentage of current smokers or patients with a history of prior myocardial infarction as compared to the ARTS-I CABG groups. Seven patients did not receive any stents during the index procedure (four underwent elective CABG, one required emergent CABG, one underwent percutaneous treatment 35 days later and one remained on medical therapy).
The percentage of percutaneous 3-vessel treatment was 46.6% in ARTS-II versus 18.0% in ARTS-I PCI (p<0.001). The mean number of significant lesions per patient was 3.6±1.3 in ARTS-II versus 2.8±1.0 in ARTS-I CABG (p<0.001) and 2.8±1.0 in ARTS-I PCI. ARTS-II patients received 3.7±1.5 stents with average total stented length of 72±32 mm vs. 2.8±1.3 and 48±22 mm in ARTS-I PCI (p<0.001).
Post-procedure creatinine kinase (CK) release was within the normal range (< 1 x Upper limit of normal (ULN)) in 81.7% (496/607). Fourteen percent (85/607) of the patients had a CK release of >1 and < 2 x ULN and only 4.3% (26/607) of the patients had a post-procedure CK release of > 2 x ULN, thereby fulfilling the ARC criteria for peri-procedural MI.
Three-year follow-up
MAJOR ADVERSE CARDIAC AND CEREBROVASCULAR EVENTS
The 3-year event rates are depicted in Table 2 and Figure 2.
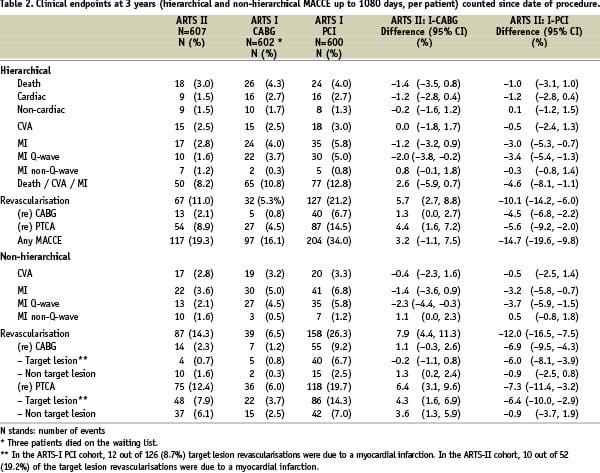
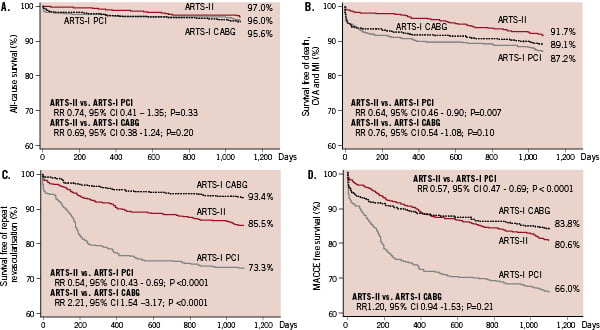
Figure 2. Kaplan-Meier curves out to three years in ARTS-I and ARTS-II; all-cause survival (A); freedom from all-cause death, cerebrovascular accident (CVA) or myocardial infarction (MI) (B); freedom from repeat revascularisation (C) and freedom from all-cause death, CVA, myocardial infarction or repeat revascularisation (MACCE) (D). Thick black line depicts the ARTS-II cohort. The thin black line depicts the ARTS-I PCI cohort and the dotted line the ARTS-I CABG cohort. P-values are Log rank.
In brief, the survival rate in ARTS-II was comparable to those of the historical surgical and PCI cohorts of ARTS-I. The death/CVA/MI event free survival was 91.7% in ARTS-II, versus 89.1% (log rank p=0.1) and the 87.2% (log rank p=0.007) in the ARTS-I CABG and PCI cohorts, respectively. Freedom from revascularisation in ARTS-II was 85.5%, which was lower than ARTS-I CABG (93.4%; log rank p<0.0001) but higher than the ARTS-I PCI (73.3%; log rank p<0.0001). The MACCE free survival was 80.6% in ARTS-II and did not differ significantly from the MACCE event free survival rate of 83.8% in ARTS-I CABG (log rank p=0.21) but was superior to ARTS-I PCI (66.0%; log rank p <0.0001).
STENT THROMBOSIS ACCORING TO THE ARC DEFINITIONS
In ARTS-II, a total of 39 patients (Table 3) experienced at least one stent thrombotic event (definite, probable or possible).
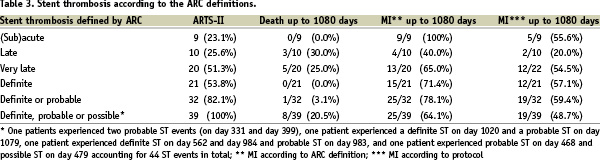
One patient experienced two probable ST events (on day 331 and day 399), one patient experienced a definite ST on day 1,020 and a probable ST on day 1,079, one patient experienced definite ST on day 562 and day 984 and probable ST on day 983, and one patient experienced probable ST on day 468 and possible ST on day 479 accounting for 44 ST events in total. The rate of stent thrombosis (definite or probable or possible) in ARTS-II was 1.5% at 30 days, 3.1% at one year, 4.4% at two years and 6.4% at three years, respectively. The rate of definite stent thrombosis in our study rose from 1.0% at 30 days to 1.6% at one year, 2.1% at two years and 3.5% at three years. By contrast, the rate of angiographically documented (definite) stent thrombosis in the ARTS -I PCI cohort was 2.8% at 30 days.3
Among the 21 patients with definite ST, six were subacute (within 30 days), four late (within 30 days – one year) and 11 very late (after one year). Four of the subacute thrombotic events occurred within the first four days post procedure. Three of these were due to suboptimal treatment, according to the independent CEC. No clear cause for the thrombotic event in the remaining three patients could be identified. Five of the subacute thrombotic events were treated with repeat intervention (four PCI, one CABG) and one lesion was left untreated. Two patients experienced a non-Q wave MI and four patients experienced a Q wave MI. There were four late definite ST (day 30-365). In one patient, the index procedure failed due to a wide dissection and on day 40 the patient was admitted with angina (CCS 3) and a total occlusion of the failed PCI was diagnosed. No increase
in enzymes or appearance of a Q wave was documented. The three remaining patients presented with in-stent restenosis and (un)stable angina but an in-stent thrombus was diagnosed by the CEC, who adjudicated the in-stent stenotic lesion as stent thrombosis. Eleven very late definite stent thromboses occurred: three were described as restenoses with intrastent thrombus, eight as total occlusion; four presented with unstable angina, seven as STEMI with enzyme elevation and/or new Q-waves.
There was no relation between the use of periprocedural GP IIb/IIIa inhibitors and ST. GP IIb/IIIa inhibitors were used in 197 out of 607 cases in ARTS-II. In this group, 9.1% (18 patients) experienced stent thrombosis. In the group without IIb/IIIa inhibitor use (n=410), 5.1% (21 patients) experienced stent thrombosis (p=0.08). Early stent thrombosis occurred in 1.2% (five patients) in the no GP IIb/IIIa inhibitor group versus 2.0% (four patients) in the GP IIb/IIIa inhibitor group (p=0.48).
Although clopidogrel was only recommended for three months, a total of 266 were still using clopidogrel or thienopyridine at one year. A stratified analysis revealed that the survival free of MACE (79.2% vs. 80.7; log rank p=0.70) and ST (92.4% vs. 95.4%; Logrank p=0.13) was identical between patients who were still on clopidogrel or thienopyridine at one year versus those without.
The impact of stent thrombosis on the clinical event rates is depicted in Figure 3a and b.
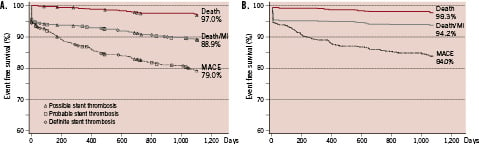
Figure 3. Kaplan Meier survival curves for death; death or myocardial infarction (MI) and death, MI or repeat revascularisation (MACE), with superimposed on the curves, individual hierarchical thrombotic event (definite or probable or possible stent thrombosis according to the ARC definitions) (A); (B) shows the same Kaplan Meier curve, after removal of the individual clinical events related to stent thrombosis – resulting in an upward shift of the three curves, reflecting higher event free rates.
Including only pre-procedural risk factors, type B2 and C lesions and the presence of an intracoronary thrombus at baseline on the diagnostic film emerged as independent predictors of stent thrombosis. Including post-procedure risk factors, the presence of an intracoronary thrombus, maximum CK post-procedure and stent length per 10 mm increase emerged as independent predictors of stent thrombosis re-adjudicated according to the ARC definitions.
Impact of Syntax score on clinical outcome
Multivariate analysis was performed on the ARTS-II population to determine independent predictors of MACCE (Table 4).
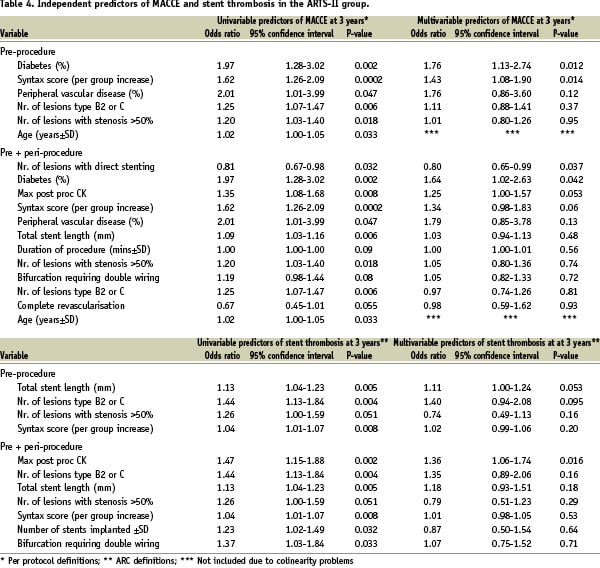
The Syntax score proved to be among the strongest predictors of MACCE (OR 1.43, 95% CI 1.08 – 1.90; p=0.014) together with the presence of diabetes mellitus (OR 1.76, 95% CI 1.13 – 2.74; p=0.012).
The entire population of ARTS-II was subdivided into patients with a Syntax score <16 (n=209), >=16 and < 24 (n=199) and > 24 (n=199). The Kaplan Meier estimates of MACCE free survival (Figure 4) show that the two subgroups with the highest Syntax score had significantly worse prognosis than the subgroup with the lowest Syntax score.
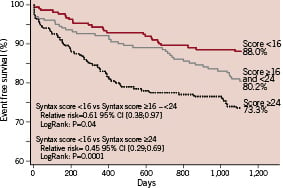
Figure 4. Kaplan-Meier curve of MACCE out to 3 years of the ARTS-II population stratified to the Syntax score: <16 (n=209), > 16 and <24 (n=199) and > 24 (n=199).
Quality of life
There were no differences in the quality of life as assessed by the self-rated thermometer of the EQ-5D questionnaire at three years among patients allocated to either CABG or PCI with bare-metal stents or SES (78, 76 and 76 in the ARTS-I CABG, ARTS-I PCI and ARTS-II respectively; p=0.1).
Discussion
Events per protocol
At three years, there was no significant difference in overall mortality between the ARTS-II and the ARTS-I PCI and CABG cohorts, despite a higher angiographic and clinical risk profile in the more contemporary ARTS-II cohort. Although the present study might have been underpowered to demonstrate any significant difference mortality, the findings concur with the previously published 10-year follow-up of the BARI study in which PCI was performed without coronary stents.28
The composite endpoint of death, CVA and MI was the lowest in the ARTS-II group and was significantly better than in the ARTS-I PCI cohort. When the MACCE rates in the three cohorts were compared, the surgical group had the lowest MACCE rate, but the actual difference in MACCE at three years between the ARTS-I CABG and the ARTS-II group was 3.2%, which did not reach statistical significance. When considering the rate of re-intervention over time it became apparent that surgical revascularisation is more durable than percutaneous revascularisation. The actual difference in MACCE between ARTS-I CABG and ARTS-II increased progressively from 4.2% at 1 year to 6.2% and 7.9% at two and three years respectively. However, it is noteworthy that the freedom from surgical or percutaneous re-intervention at three years increased from 73.7% in ARTS-I PCI BMS era to 85.7% in the ARTS-II study using SES. Furthermore, at three years, only 2.3% of patients in ARTS-II required CABG as compared to 9.2% in the ARTS-I PCI cohort treated with BMS.
A major criticism that could be levelled at the present report is that a comparison with a cohort of patients treated surgically ten years ago is inappropriate and potentially misleading considering the progress in surgical techniques and post-operative management over the past decade. The recently completed Syntax trial comparing surgery to multivessel treatment using paclitaxel-eluting stents has reported a rate of complete arterial revascularisation and use of bilateral thoracic arteries of 18.6% and 26.9%, respectively.29 Only a true randomised comparison in all-comers can definitively address the the respective merits of surgery and PCI with a particular type of stent for multivessel treatment.29 Nevertheless, the use of a comprehensive coronary score, recently designed and tested in a subgroup of three vessel treatment cohort in ARTS-II at one year is informative: testing this score anew on the entire population and for a period of three years confirms our initial observation that patients with a score of < 16 have a MACE-free survival rate greater than 88% when treated with the SES, while those with a score > 24 may potentially have better outcomes with surgery, based on the population specifically included in ARTS-II.
Comparative assessment of MI per protocol and according to the ARC definitions
Comparing the MI rates of the ARTS-II per protocol and according to the ARC definitions revealed a difference of 5% (3.6% vs. 8.6%, respectively). In ARTS-II, the criteria for an MI according to the protocol (see methods) are those applied to ARTS-I which allows comparison with the historical PCI and CABG cohorts of ARTS-I, using less sensitive criteria for diagnosing a MI. Therefore, it may be argued that the incidence of periprocedural and spontaneous MI in ARTS-II is under-reported. However, this would likely also apply to both cohorts of patients in ARTS-I. When assessing levels of enzyme release in the peri-procedural period, it became apparent that 4.3% of the ARTS-II patients had an enzyme release > 2 x ULN, the threshold criterion used for the ARC definitions. This difference in threshold alone explains the entire difference between the variation in two incidences of MI rates at three years.
Stent thrombosis
Very late stent thrombosis, perceived as a safety issue, can potentially result in an erosion of the long-term beneficial effect of multivessel treatment with DES. ARTS-II is the first study to report the impact of stent thrombosis on the long-term outcome in a population with 2- and 3-vessel disease. The rate of stent thrombosis (definite, probable or possible) in ARTS-II was 1.5% at 30 days, 3.1% at one year, 4.4% at two years and 6.4% at three years, respectively. The rate of definite stent thrombosis in this study increased from 1.0% at 30 days to 1.6% at one year, 2.1% at 2 years and 3.5% at three years; a steady increase comparable to the rate reported in an all-comer population treated with DES.7 However, the rates of overall death and MI at three years are reassuring when one compares the rates of death (3.0% vs. 4.0%) and MI (3.6% vs. 6.8%) in ARTS-II and ARTS-I PCI, respectively, despite the higher baseline risk profile in ARTS-II. Despite the fact that two third of these patients sustained an MI or underwent a repeat revascularisation, none of the patients with definite angiographic stent thrombosis died up to three years. While we recognise that late and very late stent thromboses also occur with bare metal stents, we are unable to quantify the number of these events in ARTS-I PCI cohort for comparison at this time.
Figure 3 illustrates the fact that early, late and very late, as well as definite, probable or possible stent thrombosis contributed to an erosion of the treatment effect expressed as freedom from death, death/MI and death/MI/repeat revascularisation. Out of the 127 patients who had a major adverse cardiac event (ARC definitions), 21 had a definite, 11 a probable and seven a possible thrombosis (total 39 or 30.7% of adverse events). If this incidence of stent thrombosis could be reduced significantly, as a result of better stent implantation, less thrombogenic devices, and more effective antithrombotic therapy, up to 30% of the adverse events could potentially be prevented. In the early days of bare metal stenting, more than a decade ago, we suggested that bare metal stenting could reduce the impact of restenosis in angioplasty if the early phenomenon of subacute thrombosis could be adequately controlled. 30
Limitations
First, a five year time lag exists between the groups that are being compared. Both PCI and CABG have improved with time. Second, this study is non-randomised and thus the groups are not directly comparable, precluding a formal non-inferiority comparison. Furthermore, statistical adjustment was required to correct for the differences versus the historical control group. Thirdly, while the protocol required that the lesions in ARTS-II be potentially treatable by CABG, the absence of dialogue with the surgeons prior to intervention may have caused a selection bias. However, this is not obvious considering that patients actually enrolled in ARTS-II were more complex than those enrolled in ARTS-I. Finally, the incidence and impact of stent thrombosis was not re-adjudicated according to the ARC definitions in the ARTS-I study preventing the authors to compare the results of ARTS-II to the historical PCI arm of ARTS-I.
Conclusion
At three years there was no significant difference in the incidence of the irreversible hard clinical endpoints of death, CVA and MI between the ARTS-II cohort and the ARTS-I PCI and CABG cohorts. Although CABG remained more effective in reducing the need for repeat revascularisation as compared to both PCI cohorts, the significant improvement in the reintervention rates in the ARTS-II SES cohort as compared to the bare metal ARTS-I PCI cohort resulted in a comparable MACCE rate in the ARTS-II and ARTS-I CABG cohorts at three years.
Addendum
In this study, one patient had a probable and definite stent thrombosis triggered on two consecutive days. It is clear that they may reflect the same event. As the current ARC definition does not indicate how these triggers should be reported we counted them as two separate events.
Acknowledgement
We appreciate the critical review of this manuscript by Dr Brian G. Firth.

