“Rules are for the guidance of wise men and the obedience of fools.”
Sir Douglas Robert Steuart Bader
Recently in these pages, we discussed what lessons interventionalists could learn from the aviation industry1. One of the key messages was that recognising the importance of interpersonal communication in interventional cardiology could impact on the quality of care received by our patients. “Mitigated speech” – the term linguists use for any attempt to downplay or sugar-coat the meaning of a statement usually in an attempt to be polite or to be deferential – was mentioned as an aspect of interpersonal communication that the aviation industry aims to avoid in cockpits and that we should aim to avoid in cath labs. Reading a viewpoint published last year in JAMA on the language used in some clinical practice guidelines (CPGs)2, one was struck by the parallels between “mitigated speech” and a type of indirect language, sometimes found in CPG documents.
In that viewpoint2, the authors highlighted the differences in the type of language that doctors use in communicating directly with each other for patient care and that is sometimes used in CPG recommendations. Communication for patient care, for example during handover, is typically directive and unambiguous, sometimes incorporating lists of tasks to be done. On the other hand, language used in guideline documents, particularly in areas where intermediary grade recommendations are made, can sometimes be couched in cautious, ambiguous language, limiting its usefulness for the physicians it is intended to guide. The term “hedging” is used to describe what linguists call “intentional equivocation”, part of a broader group of communication strategies that fall under the umbrella of indirectness. Reasons for “intentional equivocation” are myriad, including deference, politeness or deliberate vagueness. In guideline documents, deliberate vagueness can reflect the uncertainty that exists in a particular aspect of care but, whatever the reason, the point is well made that highly qualified recommendations or conditional statements are unlikely to serve the community the CPG is directed at. The central lesson of the viewpoint is that “in no place is the need for straightforward language greater than in clinical practice guidelines”. This echoes one of the key recommendations from the United States National Academies of Sciences, Engineering, and Medicine that guidelines should use clear, unambiguous language in framing their recommendations3. In the months and years of work that go into the drafting of a guideline – the countless papers researched and indexed, the multiple drafts and rounds of discussion, the disagreements resolved, the careful reviewing and revising, and the final checking and proofing – this tenet should remain foremost for all who contribute to the process.
The current edition of EuroIntervention is published at the time of the ESC Congress in Munich, Germany. At this meeting, the ESC continues its practice of publishing a number of guideline documents to coincide with its major annual meeting. This year four documents are scheduled to be published (Figure 1): a definition update – the Fourth Universal Definition of MI and Myocardial Injury (Chairpersons: Kristian Thygesen, Joseph Alpert and Harvey White) – and three new guidelines – CVD During Pregnancy (Chairpersons: Vera Regitz-Zagrosek and Jolien Roos-Hesselink), Arterial Hypertension (Chairpersons: Bryan Williams and Giuseppe Mancia) and Myocardial Revascularization (Chairpersons: Franz Joseph Neumann and Miguel Sousa Uva). Publication at the time of the congress facilitates wide dissemination through dedicated presentation sessions, on-site interviews and meet the experts sessions with the chairs and members of the various guideline committees, along with widespread print and electronic distribution of the documents and their highly popular pocket summaries.
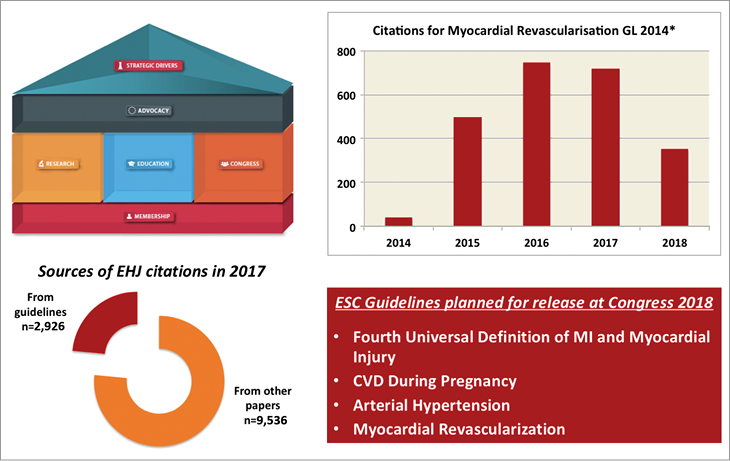
Figure 1. Impact of clinical practice guidelines. Guidelines are an important part of ESC activity; education is one of the pillars of the ESC strategic plan (upper left panel). The guideline on Myocardial Revascularization is a widely cited document (*numbers of citations of the version of the 2014 guideline published in the European Heart Journal) (upper right panel). Citations of guideline documents make up a significant portion of the total number of citations a journal receives in a given year. An example of citations for the European Heart Journal is shown in 2017 categorised according to whether the citations related to guideline documents or other documents (data on file) (lower left panel). Three guidelines and an update on the Universal Definition of Myocardial Infarction are planned to be published at the upcoming ESC Congress in Munich, Germany (lower right panel). EHJ: European Heart Journal; GL: guideline
Indeed, CPGs have become increasingly important documents in recent years for a variety of reasons. The primary aim of these documents is to provide advice and guidance for clinicians in everyday practice as well as to inform researchers and scientists regarding standard-of-care treatments in the field. The increasing body of clinical trial and systematic review evidence4,5 makes keeping up to date extremely challenging for most doctors, and this increases reliance on the review of evidence carried out by CPG task forces. Guidelines of the ESC in particular are among the most widely read and cited of the major professional societies in cardiology. This reflects in no small part the work of staff and volunteers of the society in general, and of the Committee for Practice Guidelines – responsible for ensuring the quality and accuracy of the guidelines since 1994 – in particular. Increasingly, however, these documents have often come to assume a wider importance, frequently serving as a basis for internal institutional protocols, for insurance coverage decisions and for quality of care assessments, as well as commonly being cited in expert reports in medico-legal liability cases6. All of this, of course, places pressure and scrutiny on the processes for compiling and reviewing the documents, not infrequently generating discussion and controversy in its own right7.
The Myocardial Revascularization guideline is one that is of particular relevance for readers of this journal. This guideline came into being as one of the first joint guidelines drafted and published in cooperation with the European Association of Cardio-Thoracic Surgeons. William Wijns and Phillippe Kohl chaired the first version, which was a milestone in guideline development, and was published in 20108. Subsequently, Stephan Windecker and Phillippe Kohl updated and extensively revised the document in 20149. The Myocardial Revascularization guideline is a document with broad reach, covering important areas as diverse as decision making and type of revascularisation, management of patients with acute myocardial infarction and stable coronary disease, antithrombotic therapy, revascularisation in heart failure and cardiogenic shock, how to handle revascularisation failure, and specific detailed advice on procedural aspects of coronary bypass surgery and percutaneous revascularisation.
These guidelines become widely cited papers. According to Scopus, the Myocardial Revascularization 2014 version published in the European Heart Journal was cited 2,357 times, which puts it in the top 1% of all cited manuscripts not only in cardiology but in medicine in general. This metric does not even take into account the multitude of citations from other journals that co-published the guideline – the EuroIntervention version was cited 132 times – nor the reach of the paper in terms of consultation and downloads – the European Heart Journal website shows that since January 2016 alone it has been downloaded 76,489 times. By way of comparison, the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, which is considerably older, has been cited 1,076 times in Circulation (including citation of the main guideline and the executive summary). Indeed, the number of citations generated by guideline documents has become a topic of heated discussion itself among journal editors and publishers10, because a large proportion of a journal’s impact factor score can be derived from CPG papers that it publishes. For example, in examining citations used to calculate the 2017 impact factor, one can see that a considerable proportion of the citations in the European Heart Journal come from a small number of guideline papers (Figure 1) (metrics last accessed 1st July 2018; all other metrics in this paragraph last accessed 20th July 2018). This observation requires qualification (being careful not to be charged with “intentional equivocation”): even if such papers were not taken into account, the impact factor of that journal remains very high – in excess of 18.
As the foregoing discussion illustrates, clinical practice guidelines are important documents for different stakeholders, for a variety of reasons. Nevertheless, we should not lose sight of their principal aim, which is to provide guidance for day-to-day clinical practice, particularly at a time when staying up to date with the medical literature is more challenging than ever. With this in mind, we look forward to the ESC Congress in Munich, and the opportunity to read and digest the new guidelines and updates which will be launched at the meeting.