Coronavirus disease 2019 (COVID-19) has exposed gaps in healthcare systems. Recognition of the impact of these gaps offers an opportunity for healthcare professionals working with political institutions to improve the intersection between health and society. Healthcare systems will need simultaneously to deal with non-COVID-19 chronic conditions (“the people left behind”) as well as maintain hospital facilities at a high level of preparedness for urgent care pandemic patients.
Chronic diseases account for 50-75% of total healthcare costs and the majority of deaths globally1,2,3,4. Current delivery models are poorly constructed to manage these chronic diseases with low adherence to quality indicators and poor control of treatable conditions. These same systems also lack flexibility to adjust to rapid swings in demand such as those imposed by the very acute, complicated COVID-19 patients requiring intensive care for an extended period of time (1-3 weeks). This further compromises the care of chronic disorders such as cardiovascular disease, diabetes, hypertension, and cancers, with delays of up to 2-3 months.
In sub-Saharan Africa, in anticipation of the pandemic, elective cardiac surgery and outpatient clinics for patients with heart failure, diabetes, and hypertension were cancelled. In Europe, in some hospital systems, 90%-95% of elective procedures were delayed, and outpatient visits for ischaemic heart disease and heart failure plunged (Figure 1). In addition, some emergency rooms have reported dramatic decreases in general patient visits for strokes, transient ischaemic attacks, and acute coronary syndromes5,6,7,8. In the USA, early on in the pandemic, federal data documented that non-coronavirus deaths exceeded those attributable to the pandemic by nearly twofold9. Similar trends were observed globally10.
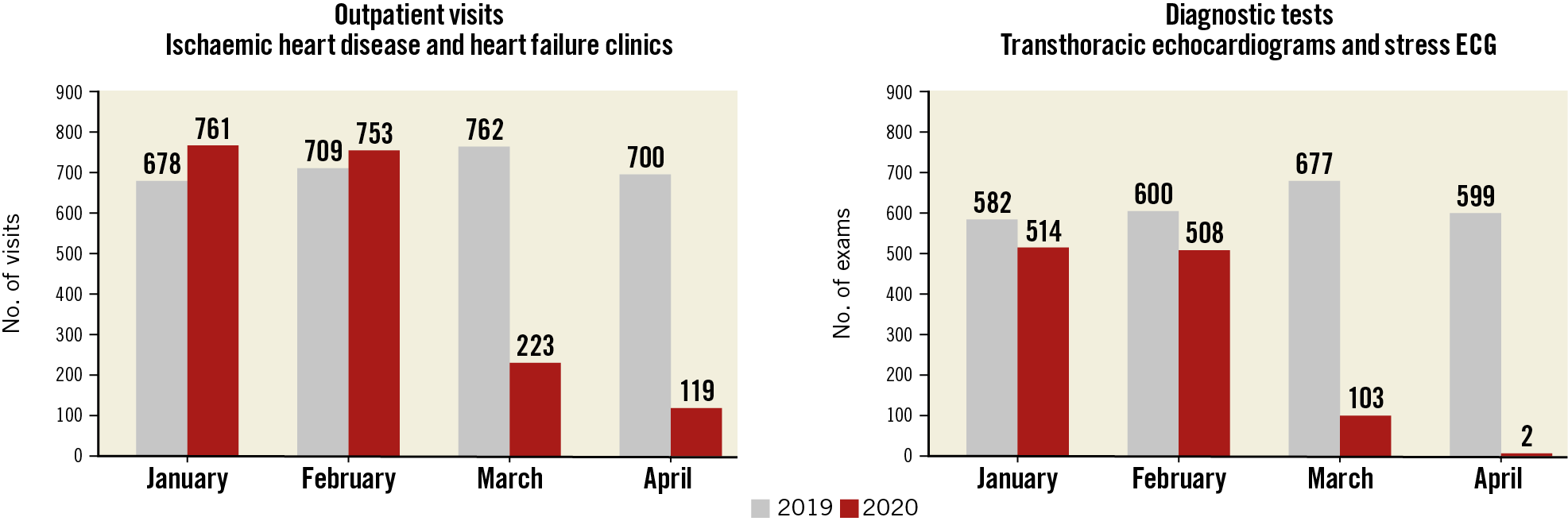
Figure 1. Number of outpatient visits (left panel) and diagnostic tests (right panel) performed in patients with chronic cardiovascular diseases (i.e., ischaemic heart disease and heart failure) at the Cardiovascular Department of Humanitas Clinical and Research Center in Milan, Italy, between January-April 2019 and January-April 2020.
In view of these considerations, both acute and chronic care will require re-engineering in the near future.
Changing healthcare systems
Variability in healthcare delivery has been associated with substantial differences in outcome for both acute and chronic patients. In Italy, early in the COVID-19 crisis, in areas where care was mainly concentrated in highly specialised private hospitals, outcomes had different timelines from those with a fully public healthcare service with a radial orientation of healthcare distribution. This allowed out-of-hospital care of both a large number of COVID-19 patients as well as improved ability to address chronic conditions such as hypertension, diabetes, and cancer. Future systems will require a higher degree of interaction between community-based physicians, specialists involved in chronic care, and intensivists. During future pandemics, specialties which focus on chronic diseases may need to deliver more general care either in outpatient facilities or in emergency room settings for non-infectious patients.
As next waves of infections occur, societies will need to implement policies that work effectively to ensure continuity of care for non-infected patients. Policies include delivering care at home with prospective protocols and remote monitoring, the re-purposing of already existent public structures as temporary regional health facilities, the development of care teams in nursing homes, the extended use of telemedicine and task shifting.
Task shifting and telemedicine will optimise management of chronic disease and during recovery from acute illnesses as part of transitional care management. Tools to deliver telemedicine have been available in selected circumstances for several years and have been approved for reimbursement. The post-pandemic restructuring of healthcare systems represents an opportunity to expand implementation of their use greatly for the continued treatment of chronic diseases.
A central issue will be the development of payment mechanisms, as the current prospective payment systems are not best suited to both the care of chronic outpatient medical conditions as well as pandemics which require high intensive care costs. Multiple tiered strategies will need to be developed tailored to the specific countries involved. For this, informed affirmative political action working in concert with professional societies will be required.
The future post COVID-19
The future will be built on identification of the gaps in the foundation of health care exposed by the current epidemic. Working with what has proven effective regionally and locally, every society and healthcare organisation needs to be mobilised with appropriate resources and reorganised to address the likely recurrence of the current epidemic as well as future pandemics but, equally as importantly, to manage the chronic disease conditions which often form the majority of clinical cases of “the people left behind”.
Conflict of interest statement
W. Wijns reports an institutional research grant and honoraria from MicroPort, being a medical advisor for Rede Optimus Research and co-founder of Argonauts, an innovation facilitator. G.G. Stefanini reports research support to the institution from Boston Scientific, and speaker fees from Boston Scientific, B. Braun, and Biosensors, not related to the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.