Abstract
Aims: Despite the advances in treatment for acute ST-elevation myocardial infarction (STEMI) during the past decades for both men and women, most previous studies reported on significantly higher unadjusted in-hospital and long-term mortality rates among women compared with men. Most of these studies have been performed in the (pre-)thrombolytic and early post-thrombolytic era. Many studies reported on myocardial infarction or acute coronary syndromes and did not specifically address STEMI. Moreover, the association of gender, quality of care and mortality has not been systematically assessed.
Methods and results: Early as well as long-term clinical outcome and delivered quality care was evaluated in an unselected cohort of 3,277 (2,367 men and 910 women) consecutive STEMI patients treated by primary PCI in a tertiary referral institution between January 1995 and 2006. Mean follow-up was 3.2±2.2 years. The unadjusted early and late hazards of mortality were not significantly different between men and women (30-days HR 0.87; 95%CI 0.67-1.12; 3-year HR 0.87; 95%CI 0.71-1.10), despite more adverse clinical characteristics in women. Gender was not an independent predictor for mortality and adjustment for covariates did not alter these results. Quality of care was similar between both sexes.
Conclusions: Despite higher age and more disadvantageous clinical characteristics, unadjusted early as well as long-term mortality in women with STEMI treated by primary PCI was equal compared with men. Women have longer ischaemic times compared with men but not due to a difference in delivered care. Quality of care before, during and after reperfusion was equal for men and women.
Introduction
Cardiovascular disease is the leading cause of death in men as well as in women, with mortality rates primarily driven by acute ST-elevation myocardial infarction (STEMI) and cardiogenic shock.
Reperfusion therapy has improved survival of patients with STEMI markedly. Primary percutaneous coronary intervention (PCI) is the optimal reperfusion therapy for both men and women with STEMI1, 2.
Since women with STEMI have higher risk profiles compared with men, the similar relative risk reduction observed with primary PCI would translate into an even larger absolute benefit for women3-5.
However, despite advances in the treatment of STEMI over the past decades, most previous studies reported on significantly higher unadjusted in-hospital and long-term mortality rates in women as compared with men6-16. The increased mortality could be explained at least in part by the fact that women with STEMI are older than men and have a higher prevalence of comorbidities such as hypertension and diabetes. In the majority of studies, adjustment for these unfavourable factors resulted in similar long-term mortality rates as men7-9,12. Adjustment for these factors also reduces the difference in in-hospital mortality. However, in most studies in-hospital mortality remains higher in women compared with men6,8-11,13-15,17. It has been suggested that the apparent difference in in-hospital mortality might be attributed to other confounding variables including less aggressive STEMI treatment16,18,19 and fundamental biological differences in the patho-anatomy and pathophysiology of acute myocardial infarction between men and women10,13,19,20. Numerous studies have been performed to investigate whether female gender independently carries a worse prognosis after STEMI. However, most previous studies have been performed in the (pre-) thrombolytic and early post-thrombolytic era6,8,10,12,13,16,18-20. The available data on how technical progress of angioplasty, use of intracoronary stents and current pharmacotherapy impact on the outcomes of women with STEMI are limited17,21. Many studies reported data on acute myocardial infarction or acute coronary syndromes (i.e., differing in distribution of unstable angina, non-STEMI and STEMI) and did not specifically address STEMI7,8,18-22. Moreover, the association of gender, quality of care and mortality has not been systematically assessed. Therefore, the purpose of this study was to determine short and long-term mortality after STEMI, as well as delivered quality of care in women compared with men treated with primary PCI.
Methods
Patient population
Between January 1997 and January 2006, a total of 3,562 unselected and consecutive patients were admitted to our hospital (tertiary PCI centre with designated surrounding referral hospitals) with acute STEMI. STEMI was diagnosed when patients had symptoms of an acute myocardial infarction lasting 30 minutes to six hours, and up to 12 hours when signs of ongoing infarction were present, accompanied by an electrocardiogram with ST-segment elevation >1 mm (0.1 mV) in ≥2 contiguous leads. All patients underwent an immediate angiography with view to perform primary percutaneous coronary intervention (PCI). If the coronary anatomy was suitable for primary PCI, the procedure was performed with standard techniques. All patients were treated with heparin and aspirin before primary PCI. Baseline characteristics, including demographic, clinical presentation and angiographic data, and hospital procedures were collected prospectively in a dedicated database. Per protocol, follow-up data, including information on cardiac medication, was collected by written questionnaire sent to all patients after one year. In addition, hospital records and outpatient reports were reviewed and treating cardiologists were contacted. Finally, information on vital status was obtained from the Dutch national population registry (Statistics Netherlands, Voorburg, The Netherlands) per January 2007. Data for the 3,562 patients were checked for inconsistency and completeness. Duplicate patients due to recurrent STEMI (n=96), patients without confirmed diagnosis of STEMI (n=132) and patients lost to follow-up (n=57) were excluded, resulting in a final cohort of 3,277 patients with a mean follow up of 3.2±2.2 years (range one to 9 years).
Residual left ventricular function
Global left ventricular ejection fraction (LVEF) was usually assessed within one month after index hospitalisation by either echocardiography or scintigraphy. In addition to first measured LVEF, the number of echocardiographic and/or scintigraphic assessments during follow-up was scored and entered into the database.
Quality of care
In the absence of generally defined and accepted methods to retrospectively assess care after STEMI we used available parameters or treatment performance measures that may qualify for quality of care or delivered care. The selected parameters were categorised in ‘quality of care before reperfusion’, ‘quality of care during reperfusion’ (i.e. delivered care during primary PCI and index hospital admission), and ‘quality of care after reperfusion’.
Call-to-needle time and door-to-balloon time, both established performance measures of STEMI treatment, were defined as indicators of quality of care before reperfusion2. In addition to call-to-needle and door-to-balloon times, call-to-door, door-to-needle and needle-to-balloon times were determined separately. Total ischaemic time was also determined, but was not considered to be a representative indicator for delivered care, as it also entails time of onset of symptoms to call of the primary PCI centre.
Quality of care during reperfusion was assessed by evaluation of type of PCI (i.e., primary angioplasty, primary stenting), success of PCI (i.e., angiographic determined thrombolysis in myocardial infarction [TIMI] 3 flow after PCI), abciximab administration during PCI, and IABP usage.
Finally, quality of care after PCI was assessed by evaluation of aspirin, -blocker, ACE inhibitor and statin use and the number of echocardiographic and/or scintigraphic assessments of global LVEF during FUP. LVEF assessment and ACE inhibitor prescription are both recognised measures of heart failure quality of care23. Assessment of LVEF was defined as in-hospital or post-discharge assessments of LVEF with a reported LVEF, or notation of a performed or planned LVEF assessment.
Statistical analysis
Data are presented as means±SD or median [IQR] for continuous variables and as frequencies for categorical variables. Normal distribution of variables was assessed visually and by the Shapiro-Wilk test. Differences between men and women in continuous variables were tested with Student’s t test or the Mann-Whitney U statistic test, as appropriate. Differences in categorical variables were tested by chi-square test. LVEF (<40%) was dichotomised according to classical data from literature for analysis. Cumulative mortality at 3-years was calculated according to the Kaplan-Meier method. Cox regression analyses were performed to assess the effect of gender on 30-day, 1-year and 3-year mortality. Models including as covariates, gender alone, gender and age, and all significantly different baseline characteristics and univariate predictors for mortality, were sequentially assessed to elucidate how these factors confounded the gender effect. Interaction and multicollinearity were investigated. In addition, estimated survival curves for men and women at 3-year follow-up were constructed. All tests were 2-tailed, and a p value <0.05 was considered statistically significant. SPSS 15.0 (SPSS, Inc., Chicago, Illinois) was used for statistical analysis.
Results
Patient characteristics
Of the final cohort of 3,277 patients with STEMI 910 (28%) were women and 2,367 (72%) were men. Women were on average 6.4 years older (65.5±13.7 vs. 59.1±12.4; p<0.001). For both men and women, the mean age at admission increased gradually over the years, but without significant variation in the age difference by gender (Figure 1). Baseline characteristics for men and women are detailed in Table 1. Women were more obese compared with men (BMI >30 kg/m2, 20% vs. 14%, p<0.001). Furthermore, women had a higher prevalence of diabetes (15% vs. 10%, p<0.001) and hypertension (36% vs. 28 %, p<0.001) and were more likely to have cardiogenic shock (12% vs. 9%, p<0.05), while they were less likely to have ventricular fibrillation before PCI (4% vs. 7%, p<0.01).
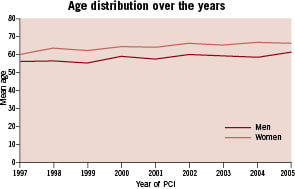
Figure 1. Mean age of STEMI patients at admission (men vs. women) over the years.
Angiographic characteristics
The distribution in infarct-related artery location differed between women and men. In women, the infarct related artery more often was the right coronary artery (RCA; 43% vs. 37%, p<0.01) and less frequently the left anterior descending coronary artery (LAD; 44% vs. 49%, p<0.05). Women were less likely to have multivessel disease (32% vs. 36%, p<0.05) compared with men. There were no significant differences in the TIMI flow before and after PCI by gender, neither were there any differences in the proportions of primary angioplasty and primary stenting. The median stent diameter in women was smaller than in men (3.0 mm vs. 3.5 mm; p<0.001).
Quality of care before reperfusion
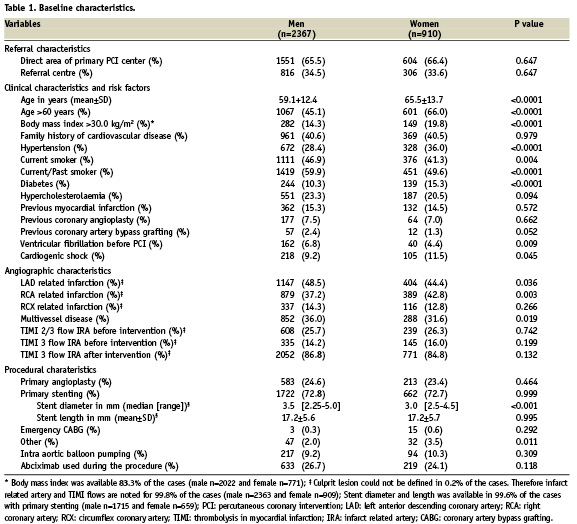
The total ischaemic time (from onset of symptoms to balloon) was longer in women compared with men (median [IQR]; 205 [153] min vs. 177 [123] min; p<0.001). This difference resulted from a longer time of symptom onset to call of the primary PCI centre (median [IQR]; 125 [127] min vs. 105 [100] min; p<0.001). There were no differences in the defined quality of care parameters, call-to-needle time (48 [22] vs. 49 [22] min) and door-to-balloon time (39 [50] vs. 39 [49] min; Figure 2A).
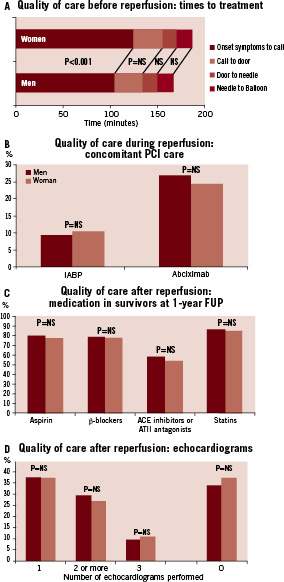
Figure 2. Quality of care (men vs. women). Panel A shows quality of care before reperfusion: no significant differences in the defined quality of care parameters, call-to-needle time and door-to-balloon time. Panel B shows quality of care during reperfusion: the concomitant PCI care (IABP or Abciximab) patients received during reperfusion. Panel C shows quality of care after reperfusion: medication received in survivors at 1-year follow-up by men and women. Aspirin, ß-blockers, ACE inhibitors/AT2 antagonists and statins were assessed in respectively in 96.5% (1947 vs. 712), 96.0% (1929 vs. 715), 93.8% (1887 vs. 698) and 96.4% (1943 vs. 712) of the cases (men vs. women). Panel D shows quality of care after reperfusion: the amount of echocardiograms performed after reperfusion for men and women.
Quality of care during reperfusion
There were no significant differences between women and men in type of PCI (i.e., primary angioplasty, primary stenting) or success of PCI (defined as TIMI 3 flow after PCI; 84.8% vs. 86.8%). Neither were there any differences in concomitant PCI care, determined by the equal usage of IABP therapy and abciximab administration (Figure 2B).
Quality of care after reperfusion
In survivors at 1-year follow-up, there were no differences in the distribution of medication between men and women (Figure 2C). LVEF was assessed in 65.5% of the cases (men n=1571 vs. women n=576).There were no significant differences between men and women concerning first reported post-STEMI global LVEF lower than 40%. Furthermore women had equal rates of documentation of echocardiographic, as well as scintigraphic LVEF assessment (Figure 2D). During follow-up a single echocardiogram was performed in 37% of both male (n=883) and female (n=336) patients (p=NS) and two or more echocardiograms were performed in respectively 29% (n=688) and 27% (n=241) of male and female patients (p=NS).
Outcomes
The unadjusted early and long-term mortality rates did not significantly differ between women and men. Mortality rates at 30 days and one year for men versus women respectively were 8.1% vs. 9.2% (p=0.283) and 10.5% vs. 12.2% (p=0.185). The Kaplan-Meier estimate for mortality at three years for men versus women was 13.8% vs. 15.6% (p=0.199). There was no significant variation in mortality rates across year of STEMI groups or age groups between men and women. In multivariate analysis there was no significant interaction between age and gender. However, there was a trend towards higher mortality rates for men in the older age groups (age ≥60; Figure 3).
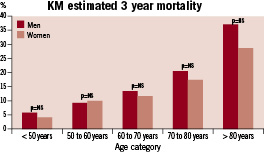
Figure 3. Kaplan Meier estimate of 3 year mortality across age groups (men vs. women). There was no significant variation in 3 year mortality across age groups between men and women. However, there was a trend towards higher mortality rates for men with age age ≥60.
The unadjusted early and late hazards of mortality were not significantly different between men and women (HR [95%CI] at 30 days, one year and at three year respectively 0.87 [0.67-1.12], 0.85 [0.68-1.06] and 0.87 [0.71-1.10]; Table 2, Figure 4). Adjustment for age did not result in significant differences in early and late hazards of mortality for men and women, though there was a trend towards lower hazards for women. However, further adjustment for differences in comorbidities and other covariates rather consolidated the similar hazards of early and late mortality for men and women.
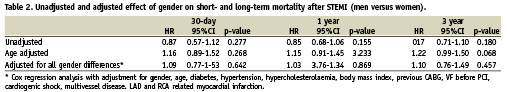
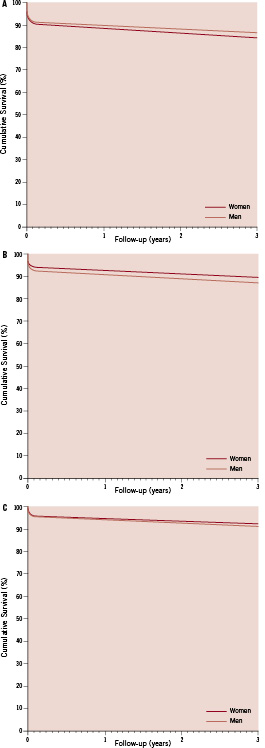
Figure 4. Cox regression cumulative survival curves at 3 years (men vs. women). Panel A depicts the unadjusted survival curves for men and women. Panel B depicts the age adjusted survival curves for men and women. Panel C depicts the survival curves adjusted for all significantly different baseline characteristics and univariate predictors of mortality for men and women (age, gender, diabetes, hypertension, hypercholesterolaemia, body mass index, previous CABG, VF before PCI, cardiogenic shock, multivessel disease, LAD and RCA related myocardial infarction).
Discussion
This study evaluates gender differences and their relation with outcome in a single centre large unselected population of patients with STEMI treated with primary PCI and contemporary pharmacotherapy. Most prior studies concerned patients from randomised clinical trials often confined to selected patients (i.e., low inclusion rates of elderly and women)9,17 or population based studies often with incomplete data for adjustment of outcomes or uncontrolled confounders18,19,22. Moreover, most prior studies concerned patients treated in the (pre-)thrombolytic and early post-thrombolytic era6,8,10,12,13,16,18-20 or cohorts of acute myocardial infarction in general, without the distinction between STEMI and non-STEMI7,8,18-22. The latter being particularly important, as previous studies showed significant differences between sexes in acute coronary syndromes with regard to distribution of male and female gender, baseline and angiographic characteristics, and outcome11,13.
The main findings of this study are the similar unadjusted short- and long-term mortality between men and women with STEMI treated by primary PCI, despite more disadvantageous baseline characteristics for women and the equality in observed quality of STEMI care. Adjustment for these disadvantageous baseline characteristics and other baseline differences between men and women did not alter the gender-specific mortality rates. Although previous studies have reported on declining mortality rates in STEMI patients, primarily attributed to the advances in treatment in the past decades, our study is the first to demonstrate equal unadjusted short-and long-term mortality rates between male and female STEMI patients.
Our study confirms the persisting and well-defined comorbidity differences between men and women9,10,18. Women were older and more likely to have diabetes and hypertension, as well as STEMI complicated by cardiogenic shock. Although these covariates were predictive for mortality for both men and women, the higher disadvantageous baseline characteristics in women in our study did not result in higher mortality rates. Of note, gender per se was not an independent predictor for mortality. In accordance to observations in other studies9,10,17, women in our study had longer ischaemic times compared with men. Notably, the difference was driven by longer times from onset of symptoms to call of primary PCI centre (pre-hospital delay). However, also the longer ischaemic times did not result in higher mortality rates in women, while every delay in primary angioplasty is known to be associated with adverse outcome24. The equal mortality rates in men and women, despite more disadvantageous characteristics in women, might indicate a diminished treatment bias and/or greater efficacy of contemporary STEMI treatment in women3.
All measured parameters to study delivered quality of medical care, were equal in men and in women. Although ischaemic times were different, this was clearly not driven by differences in delivered care before reperfusion as defined by the call-to-needle and door-to-balloon time. Both these quality of care parameters were equal in men and women. During reperfusion, again no differences were observed between men and women. The rates of primary angioplasty and primary stenting, as well as the PCI success rate were equal. In addition, concomitant PCI care, as defined by the use of IABP therapy and provisional procedural glycoprotein IIB/IIIA inhibitor administration, was equal.
When considering the quality of care delivered after reperfusion in our study, both men and women received equal post-infarction pharmacotherapy (i.e. aspirin, ace-inhibitors/ATII receptor antagonists, -blockers and statins) at rates that are notably higher than in previous studies. The fact that also long-term mortality differences seem to be abolished in our study, may reflect the increased focus on modifiable risk factor treatment after reperfusion therapy for STEMI in current practice25. Finally, the number of performed echocardiograms, another parameter defined as quality of care parameter after reperfusion was similar between men and women.
Several studies suggest that women compared with men derive an even higher absolute benefit from primary angioplasty compared with thrombolysis or from primary stenting compared with primary angioplasty3-5,12,17. Therefore, the remaining gender gap even after adjustment for the more disadvantageous risk profile of women in many previous studies primarily was attributed to treatment bias. Women have been reported to be significantly less likely to receive thrombolytic therapy, primary angioplasty, and CABG, as well as proven pharmacotherapy. In the present study, all patients underwent a primary PCI strategy, thereby largely eliminating possible differences in mortality caused by treatment bias. The equal unadjusted early mortality and quality of care in our study, particularly reflects acute STEMI treatment performance. Thus, the results of our study may reflect the increased awareness of potential acute and subacute treatment bias towards women and increased adherence to the current clinical practice guidelines. Indeed, we observed a significant trend for higher average age over the years in women, as well as men, being the consequence of an over time even more liberal PCI therapy for the elderly (including women) in our hospital. Moreover, the age gap between men and women over the years remained stable. Interestingly, there was a trend for higher mortality in the higher age groups of men compared with women. This was also recently shown in a contemporary study of AMI patients and might be explained by the well-established survival advantage of women compared with men in the general population or the existence of a differential mortality rate in younger versus elder women20,26. It is likely that some differences in pathophysiology of coronary heart disease and/or genetic predisposition between men and women, but also between young versus older women, exist. However, it may be that the general survival advantage of women is of greater influence than the suggested biological differences10,13,19,20. Of note, it was recently shown that in the setting of intensive risk factor modification with established medical therapies progression or regression of the extent of coronary atherosclerosis as assessed by IVUS did not differ between men and women27.
In addition to equality in delivered care, the results of our study may also reflect the advances of contemporary STEMI treatment, which particularly may have favoured female patients, as many focused on risk factors coinciding with female gender. Especially, improvements in PCI technology and pharmacology; i.e., smaller guiding and balloon catheters, primary stenting, smaller stents, weight adjusted anti-coagulation and glycoprotein IIB/IIIA use28, resulted in more effective treatment of patients with small vessels, complex lesions and diabetes. Indeed, the majority of patients in our study were treated by primary angioplasty and primary stenting with equal rates in both men and women. The observation that significantly smaller stents were used in women is in line with the fact that women are known to have smaller coronary arteries.
Notwithstanding, though it may be true that contemporary STEMI treatment has improved outcome for both women and men in general, it remains important for future research to focus on tailoring clinical practice guidelines and resulting STEMI treatment to specific high-risk subsets of STEMI patients. In addition, to specific age-subsets of men and women, recent studies for example show black women or diabetic women younger than 65 years still to have higher mortality rates compared with other women as well as men29,30. Furthermore, our study again emphasises the need for national programs to focus on the pre-hospital or pre-medical contact delay that women have compared with men. A recent meta-synthesis revealed, aside from clinical (different clinical presentations) and socio-demographic factors (age, socio-economic status), several psychosocial factors (i.e. correct attribution of symptoms to the heart, perceived seriousness of symptoms, low self-perceived vulnerability to heart attack, other coping strategies, media focussing on male cardiovascular risk) that contribute significantly to the pre-hospital delay of women31.
Limitations
There are several important limitations to our study. First, our study is a single centre study. However, the study cohort consists of a large homogeneous group of STEMI patients treated by primary PCI in a high volume tertiary centre with surgical back-up, as part of a national network of tertiary PCI centres with designated surrounding referring hospitals, and is representative of contemporary STEMI treatment in western countries. Second, the quality of care parameters were not pre-specified in the prospectively built database and were all conceived after final data gathering. However, this rather enabled unbiased analyses of quality of care, as at data entry it was not known to the operators, which parameters were going to be used. Third, the database did not contain detailed information on other outcome measures as revascularisation rates and other major adverse cardiac and cerebral events (i.e., recurrent MI, revascularisation rates, stroke and major/minor bleeding).
Conclusions
Despite higher age and more disadvantageous clinical characteristics, unadjusted early as well as long-term mortality rates in women with STEMI treated by primary PCI were equal compared with men. Women have longer ischaemic times compared with men, but not due to a difference in delivered care. Quality of care before, during and after reperfusion was equal for both men and women.
Acknowledgements
We are indebted to the many general practitioners and cardiologists from our region for their speedy referral of patients with acute myocardial infarction and for their superb assistance in obtaining follow-up information; and to the staff of the catheterisation laboratory, without whose enthusiastic assistance this work would not have been possible.
Appendix
The cardiologists who participated in the study were as follows: Academic Medical Center – University of Amsterdam, the Netherlands (J. Baan Jr, MD, PhD, B.J. Bouma, MD, PhD; R.B.A. van den Brink, MD, PhD; J.D. Durrer, MD, PhD; J.P. Henriques, MD, PhD; R.E. Knops, MD; K.T. Koch, MD, PhD; W.E.M. Kok, MD, PhD; R.W. Koster, MD, PhD; B.J. M. Mulder, MD, PhD; R.J.G. Peters, MD, PhD; J.J. Piek, MD, PhD, R.J.van der Schaaf, MD; H.L.Tan, MD, PhD; M.D.Trip, MD, PhD; M.M. Vis, MD, A.A.M. Wilde, MD, PhD; R.J. de Winter, MD, PhD), Ziekenhuis Amstelland, Amstelveen, the Netherlands (M. den Hartoog, MD; W.L. ten Holt, MD; Dr. H.F.J. Mannaerts, MD, PhD), BovenIJ Ziekenhuis, Amsterdam, the Netherlands (A.L.M. Bakx, MD; S.L.C. Muilwijk, MD, PhD; L.J. Jansen, MD; M.G.C. Pieterse, MD), Flevoziekenhuis, Almere, the Netherlands (L.M. Konijnenberg, MD; R.A.M. Kortz, MD, A.S.J.M. Sadée, MD; J.A.Verheul, MD, PhD), Gemini Ziekenhuis, Den Helder, the Netherlands (J.C.A. Aalders, MD; A.E. de Porto, MD; J.G.M. Tans, MD), Ter Gooi Ziekenhuizen, Blaricum , the Netherlands (E.M. Buijs, MD, PhD; G. Hoedemaker, MD; R.H.J. Peters, MD; R. van Stralen, MD) , Ter Gooi Ziekenhuizen, Hilversum, the Netherlands (J.T. Keijer, MD, PhD; P.A.R. de Milliano, MD, PhD; J. Plomp, MD; F.N. Wempe, MD), Rode Kruis Ziekenhuis, Beverwijk, the Netherlands (P.A. Boom, MD; C.H. Groen, MD; L.M. Konst, MD; M.A.C. Koole, MD, PhD; J.H.M. Spekhorst, MD, PhD; I.C.D. Westendorp, MD, PhD), Slotervaart Ziekenhuis, Amsterdam, the Netherlands (R.H. Bakker, MD; R. Bolansingh, MD, PhD; C.A. de Groot, MD; R.A. van Liebergen, MD, PhD; M.R. MacGillavry, MD, PhD; A.G. Veerbeek, MD), West Fries Gasthuis, Hoorn, the Netherlands (A. Anneveldt, MD; D.C.G. Basart, MD; P.F.M.M. van Bergen, MD, PhD; P. Dekkers, MD; C.L. Janus, MD; H.A. van de Klippe, MD).

