Abstract
Aims: It is unclear whether primary aspiration can prevent distal embolisation and thereby improve myocardial perfusion in patients presenting with acute myocardial infarction (AMI) within 12 hours after onset.
Methods and results: At 24 centres in Europe and India, 249 AMI patients were randomised to primary aspiration with the Export aspiration catheter (Medtronic Vascular, Santa Rosa, CA, USA) followed by stenting (N=120) or to conventional stenting without primary aspiration (N=129). There were no significant differences between the 2 groups in baseline characteristics or target lesion TIMI scores. Procedure time was 36.7±18.0 minutes for primary aspiration followed by stenting versus 34.5±21.5 minutes for conventional stenting (P=0.08). Debris was obtained by primary aspiration from 85.3% of the arteries. The use of a bailout technique was significantly lower for primary aspiration than for conventional stenting (5.8% vs 14.7%, P=0.02).
For the primary endpoint of the combined rate of myocardial blush grade 3 and/or ST-segment resolution >50% to assess myocardial perfusion, primary aspiration followed by stenting was superior to conventional stenting (85.0% vs 71.9%, P=0.025). Immediately postprocedure, the rate of myocardial blush grade 3 was 35.8% for primary aspiration followed by stenting versus 25.4% for conventional stenting (P=0.094). At 60 minutes post procedure, the rate of ST-segment resolution >50% was 73.5% for primary aspiration followed by stenting versus 64.8% for conventional stenting (P=0.218). Primary aspiration was also associated with a significantly higher postprocedure corrected TIMI frame count than conventional stenting (20±14.9 vs 22.8±14, P=0.02). At 30 days, there were no differences between the treatments in the rate of major adverse cardiac and cerebral events.
Conclusions: Compared with conventional stenting, primary aspiration with the Export aspiration catheter followed by stenting improved myocardial reperfusion in AMI patients presenting with TIMI flow grade 0 to 1. Further study of primary aspiration involving larger numbers of patients is warranted to assess its effect on longer-term clinical outcome.
Introduction
In the treatment of acute myocardial infarction (AMI), primary percutaneous coronary intervention (PCI) is superior to thrombolytic therapy for the restoration of normal epicardial coronary blood flow.1-3 However, improvements in coronary artery flow after primary PCI do not always lead to anticipated improvements in myocardial perfusion, as assessed by either myocardial blush or electrocardiographic ST-segment resolution.3-6 In a significant proportion of patients, abnormal myocardial perfusion contributes to increased infarct size and reduced survival.7-12
Macroscopic distal embolization has been shown to occur in approximately 15% of patients after primary PCI,13 potentially resulting in reduced myocardial perfusion, more extensive myocardial damage, and a poor prognosis. Distal protection of the microcirculation during primary PCI retrieves embolic debris in more than 70% of patients, and it may result in greater rates of normal Thrombolysis in Myocardial Infarction (TIMI) flow and blush and a higher rate of complete ST-segment resolution.14-18
Several studies have found that the use of distal protection and/or thrombectomy is safe and might improve TIMI flow and myocardial blush postprocedure.14-17,19 However, in the Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris (EMERALD) trial, 500 patients with acute MI were randomised to the combined use of these devices followed by PCI or to PCI without distal protection.18 Although the combined use of the devices effectively retrieved embolic debris, it did not result in improved microvascular flow, greater reperfusion success, or enhanced event-free survival.
The purpose of the EXPORT study was to examine the use of the Export aspiration catheter (Medtronic Vascular, Santa Rosa, CA, USA) for primary aspiration followed by stenting in AMI in comparison with conventional stenting without use of any adjunctive devices to improve myocardial perfusion.
Methods
Protocol and randomisation
Individuals eligible for enrollment were consecutive patients aged 18 years or older with AMI presentation within 12 hours of symptom onset, with 2 mm or more of ST-segment elevation in 2 or more contiguous leads, with a visual reference vessel diameter > 2.5 mm, and with a TIMI flow of 0 or 1 before placing the wire in the infarct-related artery. Principal clinical exclusion criteria were cardiogenic shock; cardiac arrest at any time before the intervention; pre-catheterisation therapy with lytic agents, with glycoprotein IIb/IIIa inhibitors, or with pacemakers; a current medical condition with expected survival less than 1 year; and current participation in other investigations. The study was approved by the institutional review board at each centre, and consecutive, eligible patients or legally authorised patient representatives signed written informed consent. Recruitment began in May 2005 and was completed in April 2007.
After eligibility criteria had been verified and signed informed consent had been obtained but before the procedure, patients were randomised – using a computerized telephone system (Linburgia Telefonische Antwoord Service BV, Rotterdam, The Netherlands) – on a 1:1 basis to 2 different patient groups: primary aspiration followed by stenting or conventional stenting without thrombectomy. The choice of PCI including stent treatment was at the investigator’s discretion, with the permissible options including predilatation followed by stenting, direct stenting, and stenting with postdilatation.
The choice of medication during the procedure – such as aspirin, heparin, clopidogrel, and glycoprotein IIb/IIIa inhibitors – was also at the investigator’s discretion, and were administrated according to standard hospital procedure.
Device description and instructions for use
The Export aspiration catheter is a 6 Fr thrombus-aspiration catheter (Figure 1).

Figure 1. The Export aspiration catheter (Medtronic Vascular, Santa Rosa, CA, USA).
The total employable length is 145 cm. The catheter has an oblique aspiration tip design, with an aspiration lumen of 0.041 inches and a crossing profile of 0.068 inches. A radiopaque marker is located 2 mm from the distal tip. Suction is provided by hand with a lockable 20-mL syringe. The aspiration rate is >30 cc of fluid per minute.
It was suggested that operators start aspiration proximal to the occluded site, gently pushing the catheter through the occlusion and then pulling it in a proximal direction, keeping negative pressure once the occlusion was crossed or if there was no longer backbleeding in the syringe. A second pass was also made with a second syringe. Withdrawal of the catheter from the artery and from the guiding catheter was performed with permanent negative pressure. After each pass, the Export aspiration catheter was flushed and the syringes emptied over a filter, and photos of the retrieved debris were immediately taken. The primary aspiration procedure ended when the following criteria were met after 2 passes with 2 full syringes: (1) achievement of normal coronary flow; (2) there was no significant remaining thrombus; and (3) the filters contained debris. If 1 of these 3 criteria was not met, then up to 2 more sets of 2 passes (up to 6 passes in total) were possible. After 6 passes, continued use of the Export aspiration catheter was at the operator’s discretion.
Postintervention data management
Electrocardiograms were collected immediately before the procedure (that is, within 12 hours after onset of AMI symptoms), immediately after the procedure, at 60 minutes after the procedure, and at 24 hours postprocedure or at discharge, whichever came first. Angiography of the index procedure was recorded for analysis. ECG and angiographic results were analysed by an independent core laboratory (Diagram BV, Zwolle, The Netherlands). Clinical follow-up was performed at 30 days.
Data collected on each patient was recorded on a web-based electronic case report form (CRF). The investigator or an authorised member of the investigational team was required to sign all completed CRFs by means of an electronic signature. The manager of the electronic CRFs and the database was the contract research organisation ClinSource (Kraainem, Belgium). A clinical events committee, consisting of 3 independent interventional cardiologists, reviewed major adverse cardiac and cerebral events (MACCE) as well as any serious adverse device effects.
Endpoints and definitions
The EXPORT trial was designed to test the hypothesis that primary aspiration followed by stenting in the treatment of AMI would result in greater reperfusion success than conventional stenting, as evidenced by a greater combined rate of ST-segment resolution >50% at 60 minutes postprocedure or myocardial blush grade 3 immediately postprocedure. Each of these two endpoints has been recognised as a surrogate marker for long-term mortality rates in patients with AMI.7,9-11,20 Even though the threshold for ST resolution and the classification for myocardial uptake of contrast have varied according to different studies, the 2 criteria chosen for the EXPORT trial reflected the most common choices. Because myocardial blush scores and ST-segment resolution are not well correlated, it was decided that the primary endpoint was met if patients fulfilled either of the 2 criteria.21
Secondary endpoints included the magnitude of ST-segment resolution; improvement in TIMI flow; the corrected TIMI frame count; MACCE (defined as the composite of death, reinfarction [Q- and non-Q-wave], emergent bypass surgery, target lesion or vessel revascularisation; or cerebrovascular accidents; the rate of distal embolisation; and the rate of required bailout techniques (defined as rescue use of the aspiration catheter, distal protection, or glycoprotein IIb/IIIa inhibitors).
Statistical methods
The study size was powered to demonstrate that the rate of the primary endpoint – the combined rate of ST-segment resolution >50% and myocardial blush grade 3 – would differ between the primary aspiration group and the conventional stenting group. With an estimation that the difference between the primary aspiration and conventional stenting groups in terms of the primary endpoint would be 18%, the calculated number of patients in each arm was 115 α= 0.05, power = 80%). Considering a potential dropout rate of 8% during the study, the sample size in each arm was increased to 125 patients.
All analyses were performed according to the intention-to-treat principle. Categorical variables are presented as frequency values and were compared with the Fischer exact test. Continuous variables are expressed as mean ±SD and were compared using unpaired Student’s t-test. A P value <0.05 was interpreted as statistically significant.
Results
Patient population
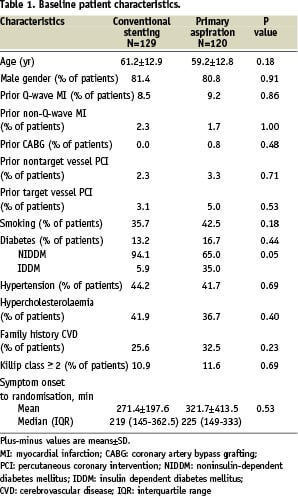
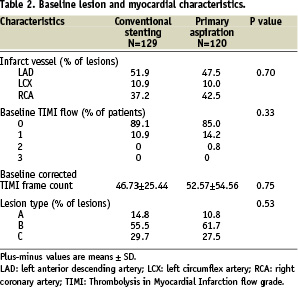
Between May 2005 and April 2007, 249 patients with AMI at 24 academic and community-based centres in Europe and India were randomised to receive either primary aspiration followed by stenting (N=120) or conventional stenting alone (N=129). Baseline demographic and angiographic features were well matched between the 2 randomised cohorts (Table 1 and Table 2).
Procedural results
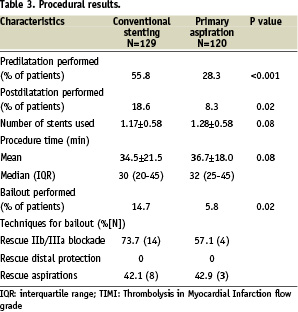
Procedural data are reported in Table 3.
Among the 120 patients randomised to receive primary aspiration, the Export aspiration catheter was used in 97.5%. Mean aspirate volume was 38.08±26.51 cc, and visible debris was extracted from 85.3% (99/116) of patients. The mean number of primary aspiration runs was 2.42±1.15. Figure 2 shows an example of the material retrieved by primary aspiration.
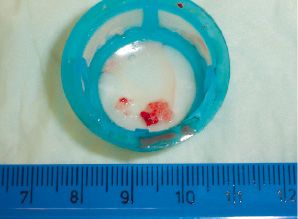
Figure 2. An example of atherosclerotic debris retrieved by primary aspiration. The cell strainer holds gross specimens, showing a large red thrombus and smaller atheroma and white thrombus debris.
The procedure duration was longer in the primary aspiration group than in the control group, but the difference was not statistically significant (36.7±18.0 vs 34.5±21.5 minutes, P=0.08). In the conventional stenting group, a significantly higher number of patients underwent predilatation and postdilatation. The rate of bailout was significantly higher for the conventional stenting group than for the primary aspiration group (14.7% vs 5.8%, P=0.02). Reported reasons for bailout were the presence of thrombus (5.4% in the conventional stenting group vs 0.8% in the primary aspiration group), slow reflow (5.4% vs 1.7%), distal embolisation (2.3% vs 3.3%), lack of ST resolution (0.8% vs 1.7%), and other (3.9% vs 0.8%). Techniques used to manage bailout were rescue glycoprotein IIb/IIIa inhibitors (14 patients in the conventional stenting group vs 4 patients in the primary aspiration group) and rescue aspirations (8 patients vs 3 patients).
There were no significant differences between the two groups in the use of procedural medications. In the primary aspiration group, 65.8% of patients received glycoprotein IIb/IIIa inhibitors, 75.0% heparin, 43.3% aspirin, and 44.2% clopidogrel. In the conventional stenting group, 69.8% of patients received glycoprotein IIb/IIIa inhibitors, 70.5% heparin, 43.4% aspirin, and 39.5% clopidogrel.
Assessment of myocardial reperfusion
Postprocedural ST-segment elevation regressed >50% in a significantly higher number of patients treated with primary aspiration (73.5% vs 64.8%, P=0.218) (Table 4).
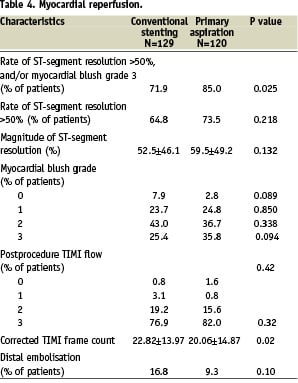
There was no difference between the groups in terms of myocardial blush grade, but the percentage of patients with myocardial blush grade 3 tended to be higher in the primary aspiration group than in the conventional stenting group (35.8% vs 25.4%, P=0.094). There was also a trend for a higher rate of a myocardial blush grade 0 in the conventional stenting group (7.9% vs 2.8%, P=0.089). For the combined primary endpoint of the rate of postprocedural ST-segment resolution >50% and/or a myocardial blush grade 3, primary aspiration was significantly superior to conventional stenting. With primary aspiration, 85.0% of patients achieved the combined primary endpoint versus 71.9% without aspiration (P=0.025). The primary aspiration group had a significantly lower corrected TIMI frame count (20.06±14.87 frames vs 22.82±13.97 frames, P=0.02).
Clinical outcomes
At 30 days, the occurrence of death, reinfarction, target lesion revascularisation, and cerebrovascular accidents was similar in both groups, resulting in similar MACCE rates. In the primary aspiration group, 3 patients died from cardiac causes, and in the conventional stenting group, 5 patients died from cardiac causes. Reinfarction occurred in 2 patients in the primary aspiration group and 1 person in the conventional stenting group.
Discussion
The use of percutaneous intervention for the treatment of AMI has two goals: the achievement of normal epicardial flow and optimal myocardial tissue reperfusion. The quality of reperfusion is a strong predictor of long-term outcomes.7,22-26 By causing capillary obstruction, endothelial dysfunction, and inflammation, thrombus and plaque embolisation affect myocardial reperfusion and are associated with a poor long-term outcome.10 Both protection devices and thrombectomy catheters have been proposed to reduce the impact of microscopic and macroscopic embolisation from thrombus-containing lesions.
In the present randomised study, compared with conventional stenting, employment of primary aspiration was associated with a significantly improved epicardial reperfusion, as assessed by the combined primary endpoint of ST-segment resolution and/or myocardial blush grade 3. Although myocardial blush has been related to infarct size and long-term mortality after AMI in previous studies,7,20,22 the core laboratory evaluation showed only a trend for a higher rate of myocardial blush grade 3 in patients treated with primary aspiration. A possible explanation is that myocardial blush is not as powerful as ST-segment resolution as a surrogate marker of myocardial reperfusion. The selected cut off point (50%) for ST resolution was the most frequently used in past studies assessing ST resolution after lytic therapy or PCI in acute myocardial infarction. Both of these surrogate markers have been correlated with late survival after AMI, but they are weakly correlated together21. The EXPORT trial was the first to combine both surrogates into a single primary endpoint. The benefit of primary aspiration as represented by the primary endpoint was obtained in this study even though 69.8% of patients in the conventional stenting group received glycoprotein IIb/IIIa inhibitors. At 30 days, there was a similar rate of MACCE in both groups, but the study was not powered to detect a difference in this secondary endpoint.
In general, distal embolic protection devices consist of occlusion balloons or filters. Occlusion balloons block the outflow of debris, which is then aspirated out of the vessel by an export catheter. Filtering devices attached to guidewires trap embolic material downstream from the lesion. In two randomised trials, including the 500-patient EMERALD study, the distal protection system did not result in improved reperfusion, reduced infarct size, or improved clinical outcome.27 In contrast, a recent meta-analysis of the use of adjunctive mechanical devices to prevent distal embolisation in patients undergoing PCI for AMI, which identified 21 randomised trials, found that these adjunctive devices are associated with better myocardial reperfusion and less distal embolisation but without any benefit in 30-day mortality.28
Aspiration has been attempted with devices like over-the-wire balloons or angiography catheters themselves, but these techniques have limitations. Because the lumen of an over-the-wire balloon system is barely large enough to allow passage of a 0.014-inch wire, it may not allow rapid aspiration. The use of an angiography catheter as an aspiration tool is limited by its inability to be manipulated deeply enough into the infarct-related artery to approach the culprit lesion without also risking vessel injury.
However, a few studies have found that the use of an aspiration catheter alone may be beneficial for embolic protection.29-31 In the Randomized Evaluation of the Effect of Mechanical Reduction of Distal Embolization by Thrombus-Aspiration in Primary and Rescue Angioplasty (REMEDIA) trial, manual thrombus aspiration in patients with acute ST-segment elevation MI resulted in higher rates of postprocedural myocardial blush grade > 2 (68.0% vs 58.0%, P=0.020) and ST-segment resolution > 70% (44.9% vs 36.7%, P=0.034) than customary PCI alone. As in the current EXPORT study, the rate of patients achieving both angiographic and electrocardiographic criteria of optimal reperfusion was significantly higher in the aspiration group compared with the customary PCI group (46.0% vs 24.5%, P=0.025). In multivariate analysis, randomisation to aspiration was a significant independent predictor of achievement of myocardial blush grade >2 and ST-segment resolution >70% (P=0.013).31
Recently, Svilaas et al published the results of the single centre randomised TAPAS trial comparing primary aspiration using Export catheter versus conventional approach in 1071 all-comers AMI patients at the exclusion of rescue PCI32. Export use is associated with a significant reduction of blush < 2 (17.1% versus 26.3%, p < 0.001) and a greater ST resolution. This study strongly confirms the power of the two surrogate endpoints chosen in the EXPORT trial to predict clinical outcome. Despite a larger sample size, this study failed to demonstrate mortality or MACE benefit at 30 days. Histopathologic examinations demonstrated mainly platelet thrombus inside particles while plaque was present in 17% of cases. The absolute difference of blush <2 is lower in our study. Possible reasons for these differences are the enrolment of only TIMI 0/I arteries that are possibly representing those with a higher thrombus/plaque burden, the absence of direct stenting in the control group of TAPAS and the multicentre design of the EXPORT trial.
Sianos et al have shown that thrombus reduction before DES implantation decreased the rate of late stent thrombosis33. The benefit of a systematic strategy of aspiration might not be only related to a reduction in thrombus burden but also to a reduction in the amount of plaque embolisation. Kotani et al have shown that when patients with no reflow were distally aspirated, the embolic material content was more related to plaque components (macrophages, cholesterol, inflammatory cells) than fibrin alone in comparison with patients without flow impairment.34 Thus the friable part of ruptured plaque may be responsible for the microscopic embolisation that causes reperfusion impairment. These studies underscore the potential benefit of a systematic strategy of aspiration rather than the use of aspiration only in cases of high thrombus burden. Moreover, in cases of total occlusion, it is difficult to assess thrombus versus plaque volume. The TAPAS trial confirms that composition of aspirated debris is similar whatever the angiographic presence or absence thrombus.
Study limitations
This study reflected multicentre experience in a limited number of patients over a 30-day time span. Moreover, as the enrolment rate was low in some centres , a selection bias is possible even if a large majority of patients have been enrolled in high recruiting centres. No conclusions about the relationship between primary aspiration and long-term myocardial function can be drawn. The study evaluated a systematic strategy of aspiration in patients with TIMI flow grade 0 or 1. Consequently, it was not possible to form conclusions about a strategy of the use of aspiration only in lesions with a high grade of thrombus score. However, the benefit of aspiration was not reduced in patients with TIMI III flow after placement of the wire in the target vessel. Finally, the study was not powered to demonstrate benefits in clinical outcome, which would have required the enrolment of thousands of patients.
Conclusions
Compared with conventional stenting, primary aspiration with the Export aspiration catheter followed by stenting improved myocardial reperfusion in AMI patients, enrolled in 24 centres, presenting with TIMI flow grade 0 to 1 as confirmed by a composite endpoint of ST-segment resolution and/or myocardial blush grade 3, and by a significantly lower corrected TIMI frame count. Further clinical trials involving larger numbers of patients are warranted to assess the impact of primary aspiration with the Export aspiration catheter on clinical outcomes and long-term myocardial function.
Appendix
This study was supported by Medtronic Vascular, Santa Rosa, CA, USA. In addition to the co-authors of this paper the following investigators and institutions participated in this prospective, multicentre, randomised study of the Export aspiration catheter: V. Stratiev, Hôpital Lariboisiere, Paris, France; J.E. Wolf, Hôpital du Bocage, CHU Dijon, France; P. Coste, Hôpital Cardiologique du Haut Leveque, Pessac, France; D. Cacela, Hospital de Santa Marta, Lisboa, Portugal; Z. Olivari, Ulss 9 Ospedale Ca’Foncello, Treviso, Italy; P. MacCarthy, King’s College Hospital, London, United Kingdom; P. Brunel, Nouvelles Cliniques Nantaises, Nantes, France; J. Castro Rodriguez, CHU Brugmann, Brussels, Belgium; P. den Heijer, Amphia Ziekenhuis, Breda, Netherlands; P. Vermeersch, AZ Middelheim, Antwerpen, Belgium; A.L. Marques, Centro Hospitalar de Coimbra, Portugal; P. Loschiavo, Ospedale Sasdro Pertini, Rome, Italy; D. Dudek, SPZOZ University Hospital, Krakow, Poland.

