All science builds on the science that has been done before. In the case of the placebo-controlled assessment of the efficacy of modern stenting in angina relief, the science that had been done before was non-existent.
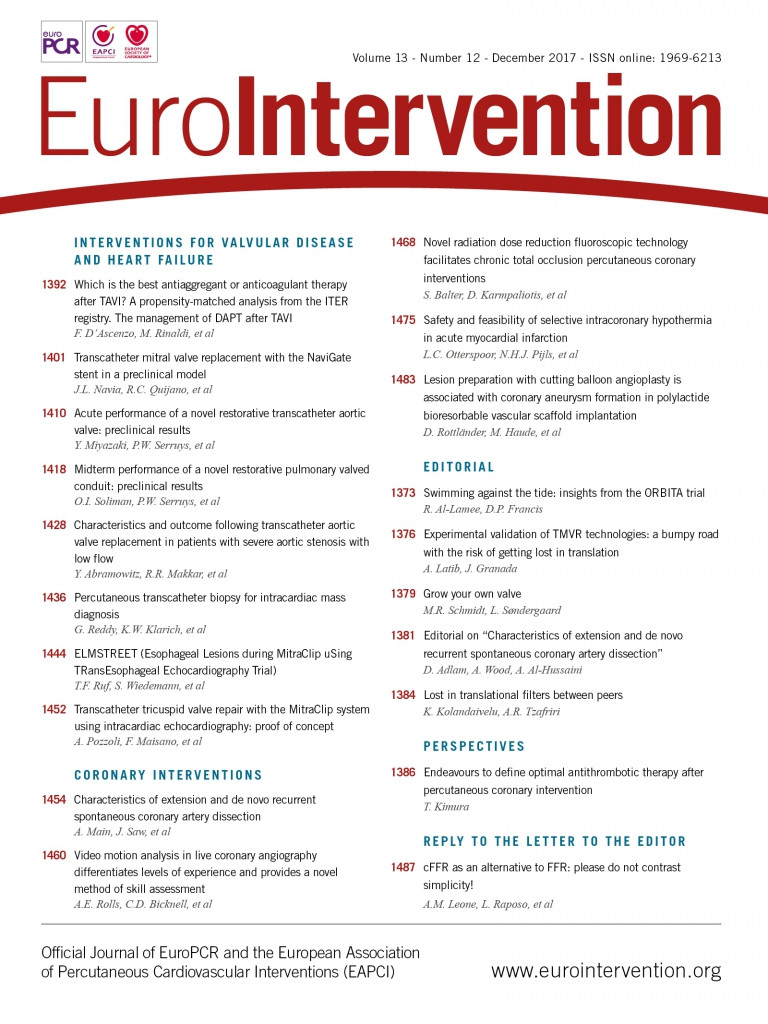
Through the retrospectroscope, critics can easily suggest modifications that might have made the effect size larger, but readers will recognise that the investigators had to plan the trial without knowing its results. In the four years of conception, design, execution and completion of the Objective Randomised Blinded Investigation with optimal medical Therapy of Angioplasty in stable angina trial (ORBITA), we fell into the trap of expecting the data to speak for itself1. We failed to anticipate the number of voices that would drown out ORBITA with competing choruses of overextrapolation and denigration.
ORBITA was conceived to deliver simple evidence for what we all believed was true, namely that patients with lesions like those in the ORBITA appendix and sufficient angina on medical therapy would indeed get a large benefit from percutaneous coronary intervention (PCI).
ORBITA was designed to expose no more patients (and for no more time) to placebo than necessary. The placebo arm needed to be sufficiently acceptable to patients and their clinicians to prevent undue selection bias and high rates of crossover or dropout. In COURAGE, 32% crossed over from the medical therapy arm to the PCI arm2. In FAME 2, the crossovers (with neither myocardial infarction nor ECG changes) comprised the majority of events, and indeed almost all occurred soon after the physician had explained that there was a haemodynamically significant lesion that had not been stented3.
The primary endpoint of ORBITA mirrored US Food and Drug Administration and European Medicines Agency recommendations for anti-anginal medications, i.e., treadmill exercise time4,5. The exercise protocol was based on the modified Bruce protocol, which is standard for anti-anginal therapies4,6.
The sample size was designed to be correct to address the question. Plain balloon angioplasty provided a +96-second exercise time improvement in the unblinded ACME trial6. ORBITA was designed to detect a 30-second effect size beyond placebo and needed ~200 patients. Readers will know that the sample size required falls with the square of the effect size one is trying to detect. To design a trial to detect 90 seconds (threefold larger) would need 32-fold fewer, i.e., only ~24 patients. The only reason to carry out a larger study would have been the belief that a smaller effect size than 30 seconds was clinically relevant. To detect a 15-second effect size (similar to the point estimate of ORBITA) would need 22 (fourfold) more patients, i.e., a trial size of ~800 patients. Randomising the additional 300 patients to placebo would only be justified if we would be prepared to recommend PCI for an average benefit of 15 seconds.
Ninety-four percent (94%) of ORBITA patients had evidence of ischaemia on one or more non-invasive or invasive tests. However, this was not an entry requirement because the majority of PCI worldwide is based on symptoms and angiographically evidenced disease, with approximately 90% of PCI performed without invasive pressure measurements7. Enrolment to ORBITA was designed to be representative of appropriate single-vessel elective PCI8.
Patients and their clinicians were only asked to remain blinded to treatment allocation for six weeks. Forty years of experience of PCI for stable angina and the previously reported dramatic symptom relief meant that it seemed unethical to ask patients to commit to a longer time period in this first blinded trial. Additionally, ORBITA needed to mirror clinical practice by including patients with high-grade stenoses in major epicardial vessels. While such patients would be expected to have the largest angina relief from PCI, they may also face greater risk of events. Therefore, a realistic blinded period had to be set in advance, to ensure the inclusion of lesions such as those in ORBITA.
The battle for funding came next. Applications to all major UK funding bodies and device companies were rejected for a variety of reasons. Expert reviewers informed us that:
– this trial is not important
– it does not address a clinically relevant question
– we know the answer to this question - of course PCI works
– investigators and patients will never agree to take part
– this trial cannot be done
Although their evaluation was disappointing, the planning of ORBITA continued. The trial was eventually funded internally by the Foundation for Circulatory Health and the Imperial Biomedical Research Centre with pressure wires donated by Philips Volcano.
Our fellow interventionists often marvel that we obtained ethical approval. In fact, the appraisal by the national ethics committee was as surprising as that of the funding bodies, but in the opposite direction. The committee raised three queries:
1. “Is it possible that we may be implanting unnecessary stents?”
2. “Does an angioplasty procedure have risks?”
3. “Are there long-term complications following angioplasty?”
When our answer to each of these questions was affirmative, their final question was, “then why has this trial not already been done?”. To that, we had no response.
Selection of ORBITA investigators was key to successful conduct. These interventionists had to understand the need for this trial and be driven by curiosity. Their hospitals would make an economic loss on each patient enrolled. They needed to be prepared to enrol all eligible patients including those with severe lesions that may have been excluded from previous trials. We are disappointed to hear accusations of selection bias because of the time taken to enrol 230 patients; in reality, it took time because unquestionably single-vessel coronary disease, with stable angina, is rarer than we had thought.
Recruitment of ORBITA participants required commitment from the investigators. A consultant cardiologist approached patients after the diagnostic angiogram. Explaining the rationale and design of ORBITA took time and dedication. We were fortunate that the majority understood the importance of this trial, and a respectable 63% of all eligible patients were recruited.
The ORBITA patients were consented to the 50:50 chance of having a placebo procedure. They understood that, if randomised to placebo, this procedure would carry risks, and that they might require another procedure to have clinical PCI after the trial end. They were also willing to measure their heart rate and blood pressure at home, and have telephone consultations several times per week with a consultant cardiologist, to introduce and up-titrate anti-anginal medications. The ORBITA patients showed that, with the commitment of an academic team and participants, placebo-controlled trials of procedures can indeed be done.
The results of ORBITA were a surprise to us. Since the design targeted a conservative expectation of effect size, we expected PCI, with anatomic stenosis resolution, easily to show a statistically significant effect beyond placebo. Checking and rechecking of the data only confirmed the same results and so, despite our preconceptions, we had to concede that the link between treating a severe epicardial stenosis with stenting and symptomatic relief was more complex than we had supposed.
More surprising than the results themselves was the subsequent reaction to them. The lay press, medical “key opinion leaders” and social media commentators competed in the speed and ferocity with which they voiced their opinions. Some overextrapolated the results to undermine PCI as a whole for stable angina. Others were just as quick to undermine the trial with remarks that were a mix of intemperate, innumerate and plain inaccurate.
The reception experienced by ORBITA, and by COURAGE a decade ago, emphasises the polarity of opinions and reflects a need for more such trials. Clinical trialists should be the first to acknowledge the limitations of their research, putting their own results into perspective. Every step in medical research should be seen as exactly that, “one more step forward”. The equal servings of praise and ridicule may continue for some time but ORBITA has undoubtedly shown that placebo-controlled interventional trials can be done, do provide new information, and should be as standard for interventional procedures as they are for medication.
Conflict of interest statement
R. Al-Lamee has received speaker’s honoraria from Philips Volcano. D. Francis has no conflicts of interest to declare.