Abstract
Evaluation of non-invasive imaging modalities is shifting to an assessment of their effect on clinical outcomes rather than of their diagnostic accuracy. For this reason, we present the most useful and commonly used non-invasive tests in the clinical scenario of patients with suspected or already known coronary artery disease in terms of their diagnostic accuracy and prognostic stratification. Each of the four sections, dedicated to a single imaging method (echocardiography, coronary computed tomography angiography, nuclear imaging and cardiac magnetic resonance), describes its early clinical applications, the main current indications and the more promising future field of interest.
Abbreviations
BOLD: blood oxygen level dependent
CAD: coronary artery disease
CCTA: coronary computed tomography angiography
CFR: coronary flow reserve
CMR: cardiac magnetic resonance
CTP: computed tomography perfusion
FFRCT: fractional flow reserve computed tomography
ICA: invasive coronary angiography
IHD: ischaemic heart disease
LGE: late gadolinium enhancement
LVEF: left ventricular ejection fraction
PET: positron emission tomography
SE: stress echocardiography
SPECT: single photon emission computed tomography
STE: speckle tracking echocardiography
TDI: tissue Doppler imaging
TTE: transthoracic echocardiography
Introduction
The anatomical assessment of coronary arteries by coronary computed tomography angiography (CCTA) and the evaluation of myocardial perfusion and left ventricle kinesis by stress echocardiography (SE), nuclear imaging and cardiac magnetic resonance (CMR) are the current reliable methods for the non-invasive assessment of patients with suspected or already known ischaemic heart disease (IHD). All four modalities have a recognised value in the diagnosis and prognostic stratification of these patients.
Echocardiography
PAST
Transthoracic echocardiography (TTE) came into clinical use in the early 1960s with “M”-mode, characterised by high temporal resolution. It is still used whenever the depth changes of echoes, which correspond to the cardiac walls or to valvular movements, have to be observed as a function of time. Subsequently, two-dimensional (2D) TTE and colour Doppler imaging were introduced. Despite the fact that the first commercial echo colour Doppler hardware was introduced 142 years after the presentation of “Doppler Effect” at the Royal Bohemian Academy by Christian Doppler, its technical progression has been very fast.
PRESENT
DIAGNOSIS
2D-TTE offers the possibility to calculate the left ventricular ejection fraction (LVEF), the main parameter of global left ventricle systolic function, easily and quite accurately, and to estimate the regional contractility of the myocardium. Several clinical indications for echocardiography have emerged in recent years. In case of suspected non-ST-elevation acute coronary syndromes, European guidelines1 rate 2D-TTE as first-line imaging technique (class 1c) to evaluate regional and global LVEF. With regard to suspected stable coronary artery disease (CAD), it is well known that the diagnosis and management of patients in this setting remains challenging. In these patients, and particularly in those with moderate-to-high pre-test probability of CAD, imaging is generally needed to evaluate the presence, extent, and functional severity of CAD. For this purpose, several meta-analyses have evaluated the diagnostic robustness of stress echocardiography (SE)2 to detect significant CAD with sensitivity and specificity ranging between 72-85% and 77-95%, respectively3. However, the presence of poor image quality affects the diagnostic accuracy and is associated with a low inter-observer reproducibility. In this regard, the development of contrast echocardiography was the most important breakthrough, which improved significantly the diagnostic accuracy of echocardiography4. Notably, thanks to the encouraging results of large multicentre studies, the latest European Society of Cardiology guidelines recommend the use of contrast in patients with stable angina, although it is still not approved for this clinical indication3. Technological advances have also improved the study of the entire function of the heart. For this purpose, tissue Doppler imaging (TDI) was first described in 1989 by Isaaz et al5. It uses frequency shifts of ultrasound waves to calculate myocardial velocity, and hence is able to sample accurately the longitudinal component of the myocardial motion, normally availing itself of colour coding. The ratio of peak velocity of mitral inflow to peak mitral annular velocity in early diastole (E/e’ ratio) permits diastolic function assessment as left ventricular filling pressure. Ommen et al6 showed that left atrial pressure could be measured non-invasively and demonstrated that an E/e’ ratio greater than 15 was associated with mean left ventricular diastolic pressure above 15 mmHg with a specificity and positive predictive value of 86% and 64%, respectively. More recently, with the introduction of 2D speckle tracking echocardiography (STE), some of the limitations of TDI, such as load and angle dependency, were partially overcome (Figure 1). Strain represents the modification of length (expressed as a percentage) of a segment relative to its baseline value measured in different directions (longitudinal, radial, transverse and circumferential). Therefore, through this kind of measurement it is possible to provide a quantitative regional myocardial function under stress conditions. However, 2D STE has some limitations such as relatively low frame rates, variability between different post-processing algorithms, and dependency on image quality.
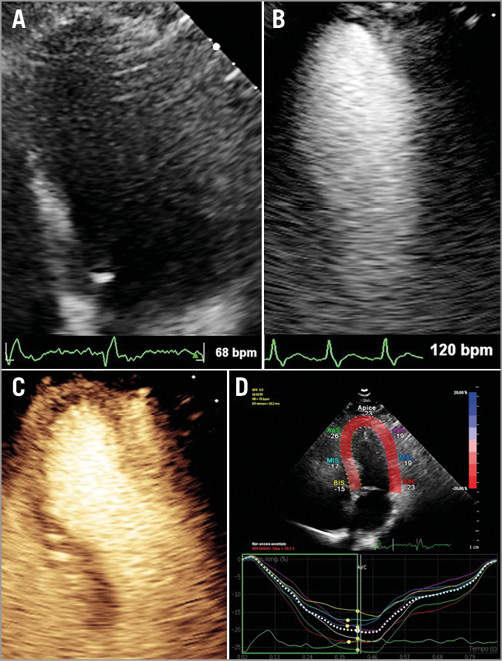
Figure 1. Dobutamine stress echocardiography. A) Apical four-chamber view of the left ventricle shows poor quality due to limited visualisation of endocardial border. B) The use of ultrasound contrast agent improves the endocardial detection, even at high heart rate. C) In the same data set a normal myocardial perfusion is assessed. D) Speckle-tracking strain analysis displaying peak systolic longitudinal strain in the four-chamber view of –20.3% which represents a normal value.
PROGNOSIS
Patients with negative SE have very low mortality and hard events7. Importantly, beyond the wall motion abnormalities evaluation, SE protocol may include the assessment of coronary flow reserve (CFR), which may add further prognostic power. In a large prospective observational study8 of dipyridamole SE including patients with known or suspected CAD, CFR on the left anterior descending artery was a strong and independent indicator of mortality, conferring additional prognostic value over wall motion analysis. A CFR ≤2 together with the presence of induced wall motion abnormalities identified a subset of the study population at high risk of one-year mortality (>10%). Moreover, some studies have demonstrated a high prognostic value of 2D STE in patients with known or suspected IHD9.
FUTURE
The introduction of 3D STE may allow us to overcome some of the above-mentioned limitations, improving reproducibility, even though it suffers even more deeply as compared to 2D STE from low temporal and spatial resolution, and its algorithms remain vendor-specific (Figure 2). A further technological advance is the possibility to detect the scar by echocardiographic approach. Gaibazzi et al10 found a good matching between TTE and CMR in scar detection despite an underestimation by TTE. This may represent a new step, leading echocardiography into the previously forbidden field of tissue characterisation.
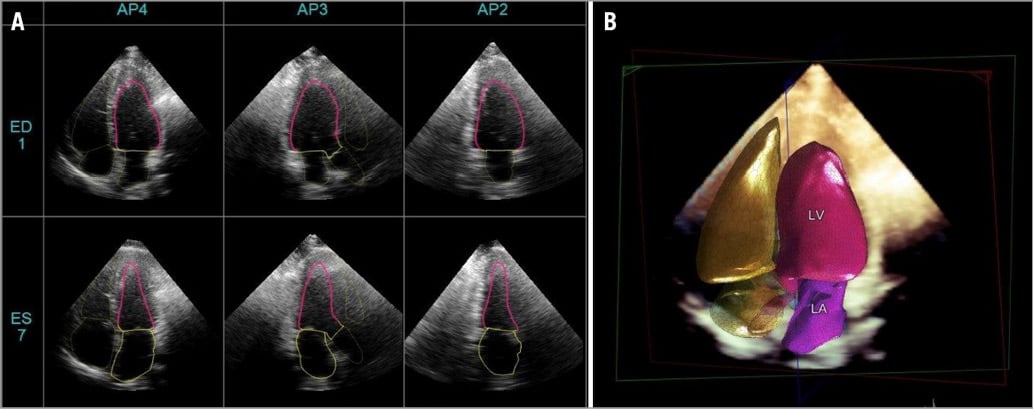
Figure 2. Heart model. Real-time fully automated transthoracic 3D echocardiographic chamber quantification using a model-based segmentation algorithm. A) Automatic endocardial detection of six different left ventricle (LV) long-axis views. B) A 3D heart model.
PERSPECTIVE
In conclusion, it is possible to hypothesise that, along with the refinement of the available software, echocardiography will have more and more diagnostic and prognostic skills in IHD and, at the same time, will represent a prompt benchside tool thanks to the fast miniaturisation of the hardware.
Coronary CT angiography
PAST
In the last decade, with the introduction into the clinical field of 64-s CT, CCTA started to be considered an appropriate tool for the evaluation of coronary arteries in some specific clinical subsets, as reported by the European Society of Cardiology11. The main clinical applications included stable chest pain and intermediate pre-test likelihood of CAD, acute chest pain after an early clinical ECG evaluation that ruled out an acute myocardial infarction, congenital abnormalities of coronary arteries and new-onset heart failure of unknown aetiology. Moreover, several papers have demonstrated a robust prognostic value of CCTA in the stratification of patients with suspected CAD on the basis of the presence of obstructive or non-obstructive CAD.
PRESENT
DIAGNOSIS
More recently, extensive literature has confirmed a very high sensitivity of CCTA in the detection of coronary stenosis, leading the European Society of Cardiology to include the method as a possible alternative to stress imaging techniques for first-line evaluation of suspected CAD3. The PROMISE trial12 recently underlined the potential of CCTA to reduce the number of unnecessary instances of invasive coronary angiography (ICA), whereas the SCOT-HEART trial13 showed that the addition of CCTA to standard clinical care clarifies the diagnosis of angina and results in more focused treatment regimes. A recent head-to-head comparison between cardiac CT and the other second-level imaging modalities showed that CCTA was the more accurate method vs. invasive coronary angiography (sensitivity, specificity and diagnostic accuracy of 91%, 92% and 91%, respectively) in patients with a low prevalence of CAD14. A recent meta-analysis on the diagnostic accuracy of CCTA in patients with unknown CAD showed a sensitivity and specificity of 98% and 84%, respectively15. Several randomised trials have established early cardiac CT as a viable, safe, and potentially more efficient alternative to functional testing in the evaluation of acute chest pain. In particular, CCTA has demonstrated the potential to reduce the length of hospital stay, the time to diagnosis, total emergency department costs and outpatient testing, and to increase the rate of direct discharge from the emergency department16. Figure 3 shows studies on the use of CCTA in the emergency department.
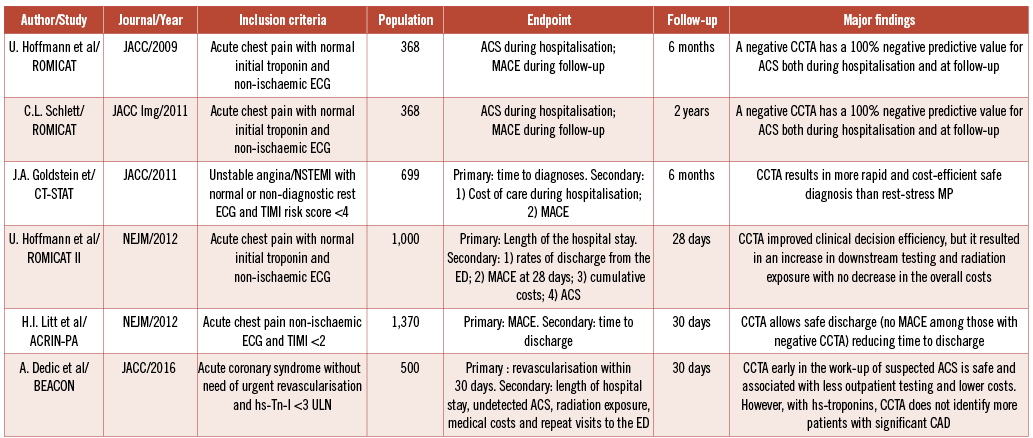
Figure 3. CCTA in the emergency department. Findings of multicentre studies on the use of CCTA in patients with suspected acute coronary syndrome. CCTA: coronary CT angiography
Recently, two methods for the evaluation of the functional relevance of stenosis by cardiac CT have been introduced in the clinical field, stress myocardial computed tomography perfusion (CTP) and fractional flow reserve computed tomography (FFRCT)17. Stress CTP demonstrated similar performance to nuclear imaging and additional diagnostic value to CCTA alone as compared to invasive FFR18. Moreover, FFRCT showed good accuracy vs. invasive FFR19 and an excellent cost-effectiveness as gatekeeper to ICA20,21. Figure 4 shows the major findings of the studies on CT perfusion and FFRCT. Elevated diagnostic performance has also been demonstrated in post-revascularisation patients22.
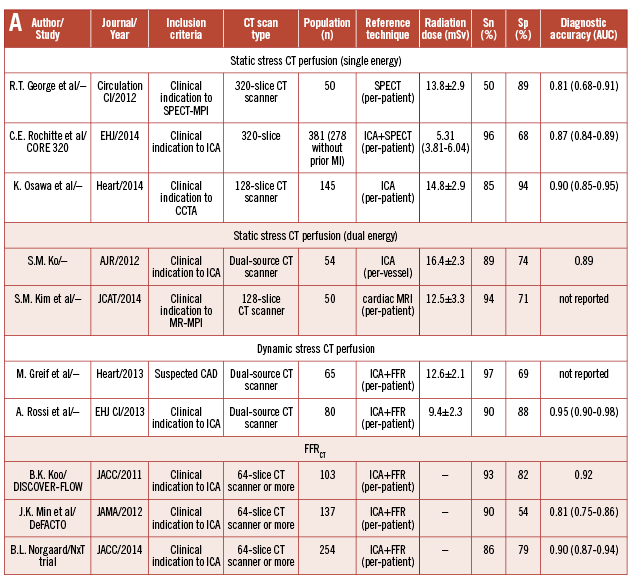
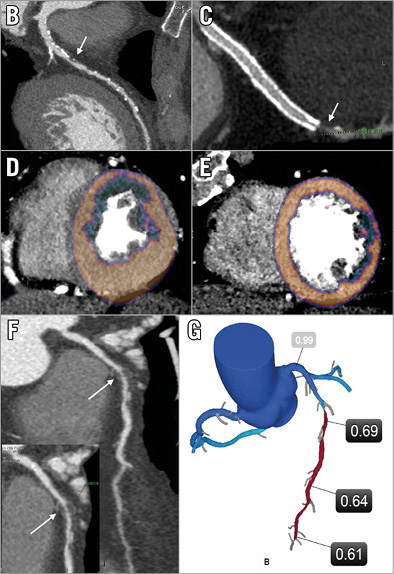
Figure 4. Stress CTP and FFRCT.. A) Major findings of the studies on CT perfusion and FFRCT.. B) & C) CCTA reconstructions of LAD (B) and LCX (C), showing significant stenoses (arrows). D) & E) Stress perfusion images showing perfusion defects on anterior (D) and lateral (E) wall of left ventricle. F) CCTA reconstructions of LAD showing a severe stenosis in the mid of the vessel (arrow). G) FFRCT evaluation showing the flow-limiting effect of the LAD stenosis. CCTA: coronary CT angiography; CTP: computed tomography perfusion; FFRCT: fractional flow reserve CT; LAD: left anterior descending coronary artery; LCX: left circumflex coronary artery
PROGNOSIS
A large number of studies have confirmed a long-term prognostic power of CCTA in attributing excellent prognosis to patients (including diabetics) without coronary plaques and intermediate prognosis in patients with non-obstructive lesions23. Recent findings have shown that some coronary plaque scores, such as the CT-adapted Leaman score, and the assessment of some high-risk coronary features, such as positive remodelling and low-attenuation plaques, allow improved prognostic stratification derived from the degree of stenosis alone24. Figure 5 shows how CCTA is able to predict cardiac events based on plaque characterisation.
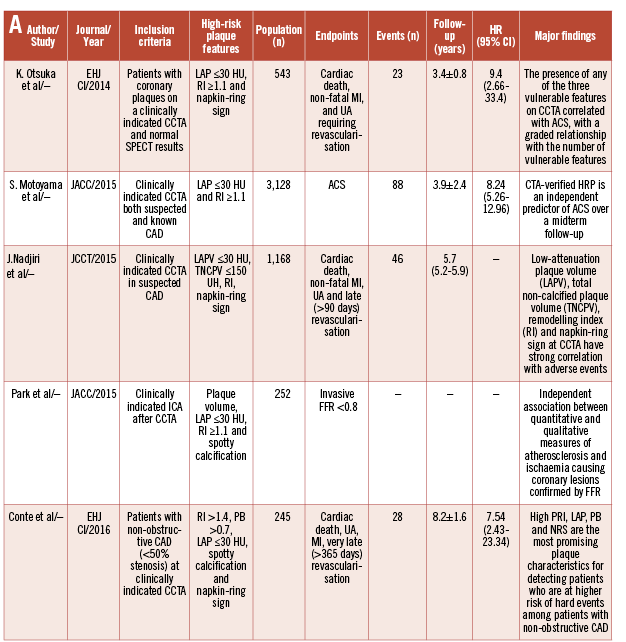
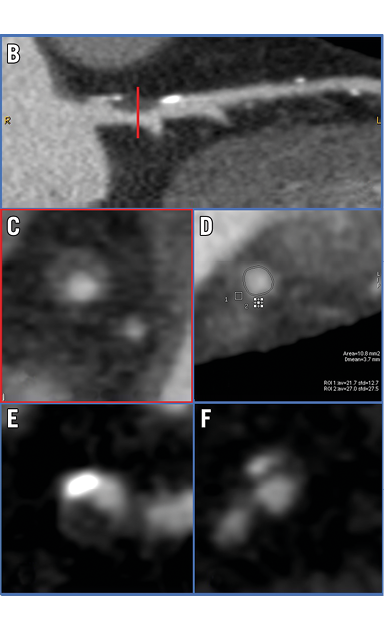
Figure 5. Plaque characterisation by CCTA. A) Findings of the studies on the prognostic value of plaque features. B) & C) Positive remodelling. D) Low attenuation plaque. E) Small spotty calcification. F) Napkin-ring sign.
FUTURE
Larger prospective trials on the comparison between CTP and FFRCT are ongoing25. Further studies on already revascularised patients are needed to support the full clinical use of the combined anatomical-functional evaluation of coronary lesions by computed tomography. Another important topic for the near future is the further implementation of coronary plaque characterisation by the use of dual-energy CT (DECT). Indeed, DECT may allow improved plaque differentiation. In addition, this approach seems promising in limiting the artefacts derived from large calcified plaque26. Moreover, to improve the prognostic power of CCTA, a better clarification of the relationship between plaque burden and cardiac biomarkers would be very useful. Finally, CCTA seems promising in the planning of complex coronary procedures, helping in the decision-making process for the treatment of three-vessel or left main CAD27.
PERSPECTIVE
The ability to combine an early identification and quantification of coronary stenosis, to go outside the lumen looking for atherosclerosis and to calculate an estimation of the coronary flow reserve supports the role of CCTA as a first-line non-invasive imaging technique in patients with unknown but suspected CAD.
Nuclear medicine
PAST
After early applications in the late 1970s, myocardial perfusion scintigraphy (MPS) by single photon emission computed tomography (SPECT) or positron emission tomography (PET) became a well-established clinical tool in patients with known or suspected IHD. Using tracers accumulating in viable myocardium proportionally to perfusion, MPS provides images of easy clinical use for the evaluation of myocardial ischaemia and viability (Figure 6).
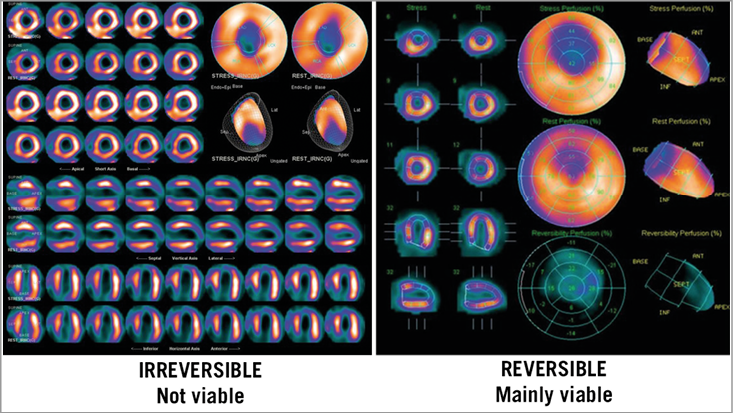
Figure 6. SPECT stress/rest perfusion imaging showing absence of ischaemia and viability (left panel) or presence of inducible ischaemia and viability (right panel) in two patients with LV dysfunction and left anterior descending coronary disease. LV: left ventricle; SPECT: single photon emission computed tomography
PRESENT
DIAGNOSIS
Thallium-201-chloride was the gamma-emitting radiopharmaceutical firstly used; it has been progressively replaced by technetium-based agents coupled with new SPECT technologies allowing better image quality and lower radiation dose28. Cardiac PET, based on the use of positron-emitting perfusion (H215O, 13NH3, 82Rb) tracers, allows a quantitative assessment of myocardial blood flow (MBF) improving the evaluation of IHD from the assessment of functionally significant coronary lesions to the recognition of microvascular dysfunction29. Actually, the main advantage of MPS over other modalities for the diagnosis of IHD is its high sensitivity due to the early occurrence of perfusion abnormalities as compared with wall motion and ECG changes according to the ischaemic cascade.
PROGNOSIS
Another major strength of SPECT and PET is the large amount of data establishing the prognostic significance of normal and abnormal MPS. A normal stress MPS has been associated with an average low (<1%) annual risk of major adverse cardiac events, while an abnormal scan holds at least a fivefold increase in relative risk30. In particular, a moderate-severe abnormality (≥10% ischaemic myocardium) identifies high-risk patients with a nearly 5% annual risk of cardiac death or myocardial infarction who benefit from ischaemia reduction by coronary revascularisation31. This evidence is at present considered robust enough to guide management of CAD patients as recommended in the current ESC guidelines3. In these patients, there is an additional incremental value in measuring absolute MBF by quantitative PET and, more recently, by quantitative SPECT. Quantitative MBF at rest and during stress is an integrated descriptor of the overall function of the whole coronary circulation and an independent predictor of cardiac mortality, providing incremental risk stratification over clinical variables and conventional perfusion imaging32. Together with the assessment of myocardial perfusion, SPECT and PET imaging (using 18F-FDG as metabolic tracer) are able to evaluate the extent of myocardial viability reliably in patients with IHD and left ventricular dysfunction33. While the STICH trial34 failed to demonstrate any relative benefit of revascularisation over optimal medical therapy in patients either with or without viability assessed by different methods, the PARR-2 study35 demonstrated that a PET-assisted management strategy improved outcome as compared with standard care in patients with severe ischaemic left ventricle dysfunction.
Despite the great success of nuclear medicine in IHD, the recent development of alternative advanced non-invasive imaging approaches, and the increased attention to a more cost-effective use of resources and to the reduction of medical radiation exposure, have mitigated its expansion. Moreover, increasing attention is being paid to justifying the use of imaging only when it translates into cost-effective management strategies able to improve patient outcome. For example, when CCTA or stress MPS-guided management strategies were directly compared in contemporary patients with a low burden of significant IHD and events, as in the PROMISE trial, neither of the two demonstrated a relevant effect on outcome. One fundamental doubt emerging from these data and from randomised treatment trials in IHD, such as the COURAGE trial, is whether revascularisation could improve outcome over optimal medical therapy in current populations of patients or in which subset of selected patients this may happen. To this purpose, some ongoing randomised studies such as the ISCHEMIA trial could shed some light.
FUTURE
Recent developments in radiopharmaceuticals and technologies for both SPECT and PET imaging are promising36. 18F-fluorpiridaz is a new PET perfusion tracer which provides high-quality perfusion images and quantitative MBF, and does not require an on-site cyclotron, potentially allowing extension of the use of PET MPS. The SPECT neuronal tracer 123I-meta-iodo-benzylguanidine is able to describe the status of myocardial innervation and could be used as a new tool of risk stratification/management in patients with ischaemic LV dysfunction. Advances in gamma camera technology, such as solid state detectors, and more accurate reconstruction techniques, have the potential to improve imaging quality, and to reduce radiation exposure and costs.
PERSPECTIVE
The introduction of hybrid PET/CT (Figure 7), SPECT/CT and PET/MR scanners and the development of fusion imaging software will allow synergistic information to be obtained, which cannot be obtained from either anatomical or functional imaging alone, and could improve management of patients with CAD14, resulting in nuclear imaging maintaining its pivotal role in the near future for the assessment of patients with IHD.
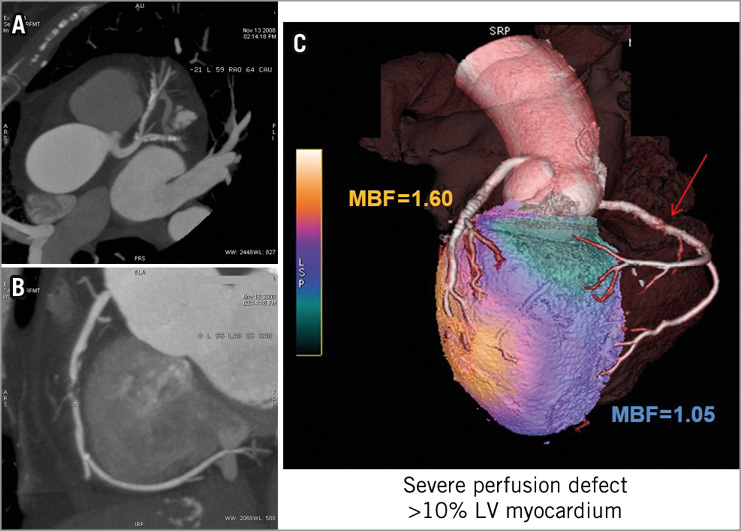
Figure 7. Anatomical and functional evaluation with hybrid CT-PET. CCTA (A) showing a diffuse coronary disease and fusion PET/CT imaging (B) demonstrating severe ischaemia in the territory of the right coronary artery in a patient with stable angina. CCTA: coronary CT angiography; PET: positron emission tomography
Cardiac magnetic resonance
PAST
Magnetic resonance imaging (MRI) is a young science but already considered pivotal for the diagnosis of numerous diseases, such that in 2003 Paul C. Lauterbur and Sir Peter Mansfield received the Nobel Prize for Medicine thanks to their discoveries in the field of MRI. Since the introduction of CMR in 1983, implemented sequences such as phase-encoded imaging for flow evaluation, contrast CMR, and steady state free precession sequences have enabled it to be considered the non-invasive gold standard for the measurement of left ventricular volumes and LVEF with a very high reproducibility, and low intra- and inter-observer variability37.
PRESENT
DIAGNOSIS
CMR is an excellent tool for the evaluation of myocardial viability and reversible perfusion defect. Regarding the first point, CMR is the best imaging technique for tissue characterisation thanks to the late gadolinium enhancement (LGE) technique that represents the cornerstone of myocardial viability. The distribution of the contrast agent within the myocardium may change according to the underlying cardiac pathology, and it progresses from endocardium to epicardium in CAD. The degree of LGE transmurality is related to the time of myocardial ischaemia and the potential functional recovery following revascularisation38. Myocardial tissue characterisation by CMR utilising T2-weighted short-tau inversion recovery imaging can also detect oedema, which is a typical feature of the initial stage following acute myocardial infarction and which represents the pathophysiological basis for the assessment of “area at risk”38. In addition, microvascular obstruction detected as a dark core within the otherwise bright region of LGE is a sign of large transmural infarcts correlating with the angiographic no-reflow phenomenon. Figure 8 shows a case of lateral myocardial infarction as detected by CMR. While the role of CMR is limited in the acute phase, it is recommended for the assessment of viability in the subacute phase of myocardial infarction with multivessel disease or in those in whom revascularisation of other vessels is considered39.
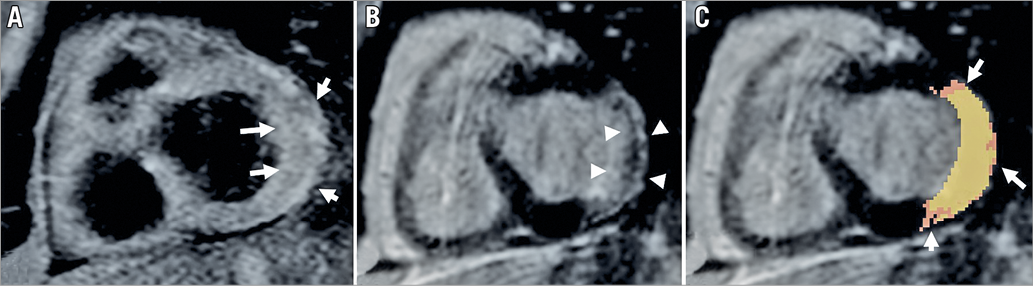
Figure 8. Tissue characterisation in acute myocardial infarction. Clinical case of lateral ST-elevation myocardial infarction due to occlusion of LCX treated with primary PCI. A) TIR-T2W sequence demonstrates oedema (arrows). B) Post-contrast inversion recovery sequence shows LGE of the lateral wall (arrowheads) with signs of microvascular obstruction (darker, hypointense area). C) Automatic evaluation of peri-infarct zone shows “grey zone” areas (arrows). LCX: left circumflex; LGE: late gadolinium enhancement; PCI: percutaneous coronary intervention; STEMI: ST-elevation myocardial infarction; TIR-T2W: triple inversion recovery T2-weighted
Regarding the diagnosis of reversible ischaemia, stress CMR represents an excellent alternative to other non-invasive stress tests to detect perfusion defects and regional wall motion abnormalities. Current European Society of Cardiology guidelines on the management of stable CAD3 recommend stress CMR in patients with intermediate-to-high (50-85%) pre-test probability of CAD or if LVEF is <50% in the absence of typical angina (class IB), and in patients with resting ECG abnormalities (class IB). The CE-MARC study, the largest prospective randomised single-centre trial on stress CMR, showed its superiority over SPECT, with a higher sensitivity (87% vs. 67%, p<0.0001) and negative predictive value (91% vs. 79%, p<0.0001) but similar specificity and positive predictive value40. Finally, the CE-MARC 2 study showed a lower probability of unnecessary ICA with CMR as compared to NICE guideline-directed care41. To complement CMR’s comprehensive multiparametric ability, the strain technique has recently been applied to CMR, proving to be a reproducible method for the evaluation of myocardial deformation. In addition, novel T1 relaxation time maps (“T1 mapping”) offer a quantitative evaluation of diffuse myocardial fibrosis, and hence overcome the limitation of traditional LGE sequences when no normal myocardium is present42 (Figure 9). The introduction of 3D CMR perfusion imaging represents a promising technique for measurement of myocardial blood flow over SPECT or PET. Compared to the conventional 2D multislice perfusion imaging, it allows quantification of the percentage of ischaemic myocardium and reduces the scan time by a simultaneous acquisition of all slices at the same point of the cardiac cycle43.
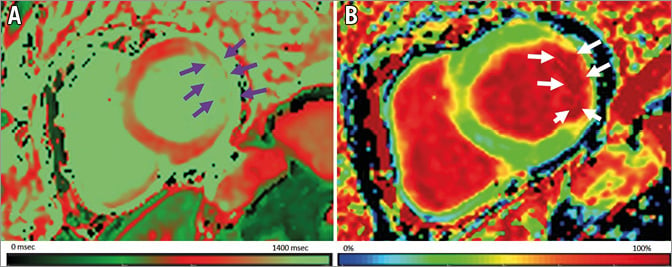
Figure 9. T1 mapping and extracellular volume in ischaemic heart disease. Same case as Figure 8. A) Native T1 mapping using a modified Look-Locker inversion recovery pulse sequence demonstrating higher T1 values in the lateral wall (arrows). B) ECV mapping that is increased in the lateral wall (arrows). ECV: extracellular volume
PROGNOSIS
Different parameters regarding tissue characterisation by CMR, such as oedema on T2-weighted images, signs of microvascular obstruction and LGE, are demonstrated to be independent predictors of poor prognosis in patients with reperfused ST-elevation myocardial infarction44 or in patients with suspected or known CAD45. As concerns the strain technique, recently applied to CMR in the field of myocardial deformation assessment, the initial literature demonstrates that it aids in the accurate identification of patients at high risk of future cardiac events and revascularisation procedures46 (Figure 10).
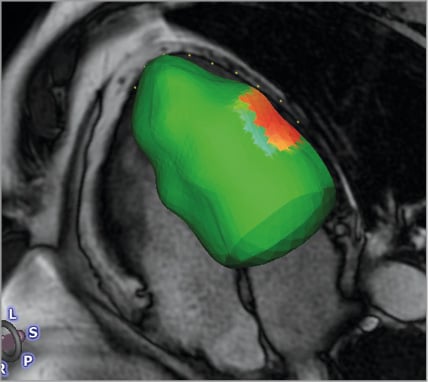
Figure 10. Myocardial strain in ischaemic heart disease. Same case as Figure 8. CMR-tissue tracking 3D model shows a reduced radial, circumferential and longitudinal strain of the anterolateral segment (orange area).
FUTURE
Coronary MR angiography offers the possibility to visualise the coronary tree directly. Currently, its indications are limited to the detection of aberrant origins of coronary arteries, coronary ectasia and/or aneurysms (class I) and evaluation of bypass grafts (class II)47. In addition, molecular imaging is an emerging method to study atherosclerotic plaque composition. It uses superparamagnetic and paramagnetic nanoparticulate probes with T1 and T2 contrast mechanisms that target molecular and cellular changes involved in early atherosclerotic lesion formation and in the process of plaque rupture and erosion48. Another promising application of CMR is the blood oxygen level dependent (BOLD) sequence that uses endogenous contrast between oxyhaemoglobin and deoxyhaemoglobin. This sequence is based on the changes of myocardial oxygenation under stress, revealing myocardial ischaemia49. The BOLD technique represents an important future application, particularly in patients with severe renal failure in whom the use of exogenous contrast agents should be avoided.
Authors’ perspectives
Despite its wide application in ischaemic heart disease, the main challenge of CMR consists in spreading its diffusion and in overcoming the organisational difficulties. Most likely, the further development of non-contrast techniques and “fast sequences” will help to achieve this objective.
Conclusion
In conclusion, as reported in the current guidelines, CCTA appears to be more appropriate in the setting of patients with suspected IHD and a low-to-intermediate pre-test likelihood of coronary artery disease, due to its very high diagnostic accuracy and robust prognostic value in this clinical scenario. On the other hand, stress imaging tests seem preferable in patients with an intermediate-to-high risk of coronary artery disease and in patients with known IHD. Echocardiography and CMR appear to be more appropriate than nuclear imaging in young patients because of the absence of radiation exposure.
Conflict of interest statement
G. Pontone has received institutional research grants or honoraria as a member of the speakers bureau of General Electric, Bracco, Medtronic, Bayer, and HeartFlow. A. Andreini has received research grants (to the institution) from GE Healthcare and Bracco. A. Guaricci and D. Neglia have no conflicts of interest to declare.