Abstract
Background: Health related quality-of-life (HRQL) beyond one year of treatment of multivessel coronary artery disease with stenting or coronary artery bypass grafting (CABG) is yet unknown. The Arterial Revascularisation Therapy Study (ARTS) was designed to compare CABG and stenting in multivessel disease.
Methods and results: HRQL was evaluated at baseline, at 1- month and at 6-, 12- and 36 months after revascularisation using the Short Form Health Survey (SF-36) in patients randomised to stenting (n=483) versus CABG (n=492). Both stenting and CABG resulted in significant improvement of HRQL and anginal status. Although there was a trend for better HRQL after CABG up to one year, the disparity between the two procedures decreased long-term. Most of the difference between the two procedures was attributed to repeat interventions in the stent group; at three years, 19% of stent patients versus 13% of CABG patients (p<0.0001) had undergone a repeat intervention. On most of the SF-36 scores, there was no difference between diabetics and non-diabetics, with diabetic patients having a worse score only on general health and physical functioning at all time points (p<0.0001).
Conclusions: Both stenting and CABG resulted in a significant improvement in HRQL especially up to one year, but CABG was associated with less angina at all time points. There was a trend for better HRQL after CABG, but this difference was mainly attributed to repeat revascularisation in the stent group. Based on these findings, patients should select for themselves whether or not they would prefer the improved HRQL benefits after CABG, or whether they would prefer more angina after PCI and avoid a major operation.
Introduction
Multiple randomised studies have demonstrated similar mortality rates for percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG). However, patients undergoing PCI are much more likely to have recurrent ischaemia with subsequent repeat interventions. When there is an absence of a clear advantage for either CABG or PCI, revascularisation strategies are selected based solely upon technical considerations and perceived procedural risks. Because the elimination of ischaemia is more complete with surgery, patients may derive a greater health related quality-of-life (HRQL) benefit with CABG compared with PCI. In the early 1990s, the pre-stent era, several clinical trials comparing CABG with balloon angioplasty included HRQL and showed that CABG patients had greater improvement in HRQL scores1-3. More recently, the AWESOME investigators reported equivalent six-months HRQL between PCI and CABG4. On the other hand, the Stent or Surgery (SoS) study group reported a significant improvement in angina-related health status at six months and at one year after intervention5. Furthermore, a few observational registries identified that over 12 months of follow-up health status was more improved after CABG than after PCI, but this was primarily driven by the adverse influence of restenosis after PCI6,7. However, almost no data are available to describe the HRQL recovery after revascularisation beyond one year. Only the Arterial Revascularisation Therapy Study (ARTS) reported the HRQL, assessed by the 5-item EuroQOL EQ-5D health status, at one and three years8. ARTS was a randomised trial comparing stenting with CABG in patients with multivessel disease9. At five years, there was no difference in mortality, myocardial infarction or stroke between the two procedures10. However, increased repeat revascularisation was needed in the stent group.
Besides the EQ-5D, ARTS also evaluated the more well-known and more detailed Short Form Healthy Survey (SF-36). The objective of this study was to evaluate the SF-36 and anginal status at baseline, at 1-month, and 6-, 12 and 36-months of patients enrolled in the ARTS trial.
Methods
Population
Between April 1997 and June 1998, 1,205 patients who had multivessel disease and considered equally treatable with the two modalities were randomised to either stent implantation (n=600) or CABG (n=605) at 67 participating centres worldwide as part of the ARTS trial. Details of this study have been described previously11. The indications for revascularisation included silent ischaemia, stable or unstable angina pectoris, and the presence of at least two de novo lesions located in different major epicardial coronary arteries, potentially amenable to stent implantation. For each patient, entry into the study required agreement from both the surgeon and interventional cardiologist that an equivalent degree of revascularisation could potentially be obtained using either approach. Specific exclusion criteria from the randomised trial may be summarised as follows: left ventricular ejection fraction <30%, left main stenosis, history of cerebrovascular accident, transmural myocardial infarction within the preceding week, severe hepatic or renal disease and need for concomitant major surgery. All patients gave written informed consent.
As the SF-36 questionnaire was not translated in all languages of the participating centres, of the total 1,205 patients, 1,035 patients were eligible to participate in this substudy. Of these eligible patients, 975 (94%) agreed to participate. At respectively 1-, 6-, 12- and 36 months follow-up six, 20, 24 and 43 patients had died (equally divided among both treatment groups). The corresponding participating rates were 100% at baseline and at one month, and 92% at 6-, 12- and 36 months.
Health-related quality of life and anginal status
The Short Form Health Survey (SF-36) is a generic measure of HRQL that assesses eight domains, i.e. physical functioning, role physical functioning, role emotional functioning, mental health, vitality, social functioning, bodily pain, and general health12. Scale scores are obtained by summing the items together within a domain, dividing this outcome by the range of scores and then transforming the raw scores to a scale from zero to 100. A higher score on the SF-36 sub domains represents a better HRQL with a high score on the bodily pain scale indicating freedom from pain. The scale has good reliability with Cronbach’s alpha ranging from .65 to .96 for all subscales12. The SF-36 was administered at baseline, and at one, six, 12 and 36 months’ post-index procedure.
Anginal status was assessed by the Canadian Cardiovascular Society (CCS) classification.
Statistical analysis
Comparisons between treatment groups were analysed according to the intention-to-treat principle. Baseline characteristics were compared by unpaired Student’s t test for continuous variables and Fisher exact tests for categorical variables. Health status recorded over follow-up time was analysed with repeated measures analysis of variance with Bonferroni correction. All tests of statistical significance were 2-tailed and a probability value of <0.05 was considered significant. A pre-specified subgroup analysis was performed in the stent group to investigate the effect of repeat revascularisation on HRQL. Since the BARI investigators reported better survival in diabetics after CABG, much attention has been seen in this subgroup. Therefore, also, an analysis was performed on patients with and without diabetes3.
Results
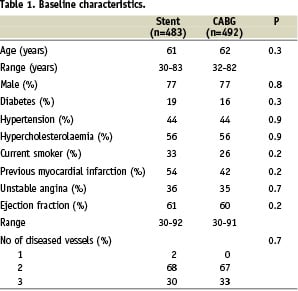
Baseline clinical and procedural characteristics of the 975 patients who participated in this ARTS randomised HRQL substudy were similar in both treatment groups (Table 1).
Mean age was 61 years and 77% were male. There were no differences in baseline characteristics between responders and non-responders on the SF-36.
The time course of recovery from the coronary intervention differed by treatment strategy (Figure 1).
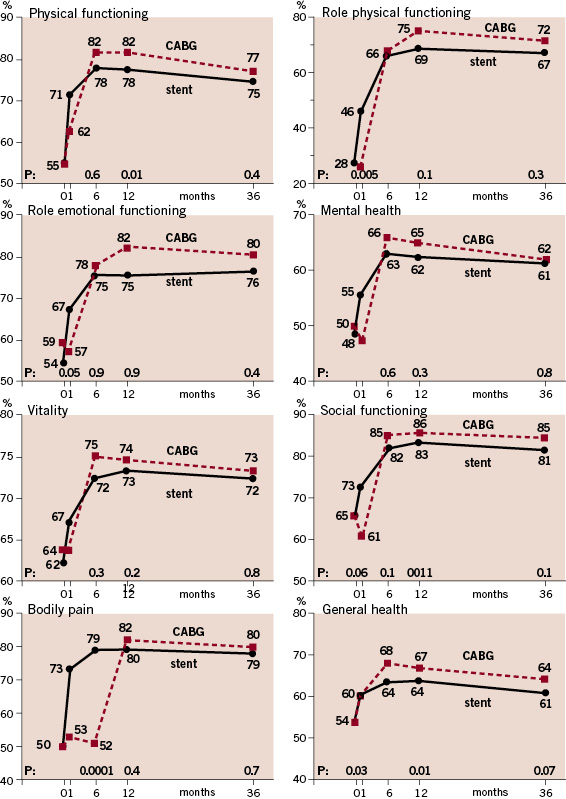
Figure 1. SF 36 subscales according to CABG and stenting at baseline, 1, 6, 12 and 36 months.
Patients undergoing CABG experienced a decrease in most SF-36 subscales in the first post-operative month, whereas in the group of patients undergoing PCI the HRQL immediately increased significantly. This improvement varied between 10% to 64% at one month. Between one and six months, most HRQL scores improved substantially, but the strongest in the CABG group up to an equal or greater level than the PCI group. Only bodily pain remained low in the first six months in patients undergoing CABG. Between six and 12 months, the HRQL sub domain scores for all stent and most CABG remained similar. Physical and emotional role functioning further increased after CABG, and bodily pain finally improved to the same stent level. Ultimately, three of the SF-36 sub domain scores (physical functioning, social functioning and general health) were significantly higher in the CABG than in the stent group. During longer follow-up up to three years, all sub-domain scores in both treatment groups slightly decreased and converged to the same level.
To better explain differences in HRQL between CABG and stenting, an additional analysis was performed to investigate the effect of repeat revascularisation on the relative benefit of CABG versus stenting. Although among those PCI patients who did not require repeat revascularisation (73% of the stent patients), average HRQL scores at six months and later were similar with the scores in the CABG patients, whether or not these CABG patients had a repeat intervention (Figure 2).
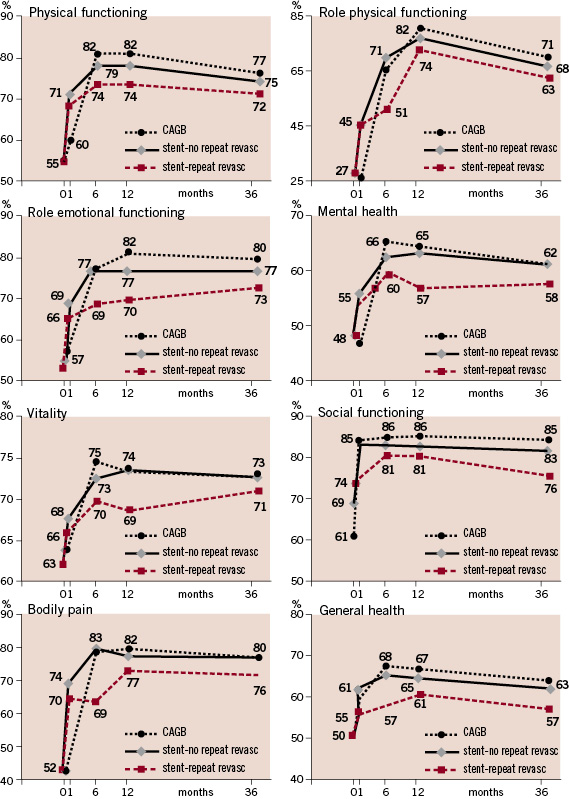
Figure 2. SF 36 subscales according to CABG and stenting with or without repeat revascularisation at baseline, 1, 6, 12 and 36 months.
Anginal status
The incidence of angina after stenting and CABG is shown in Figure 3.
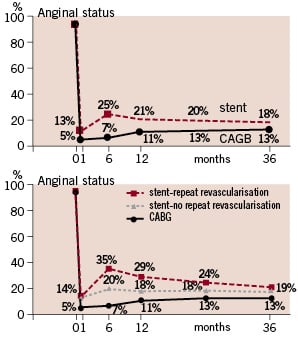
Figure 3. Anginal status according to CABG and stenting with or without repeat revascularisation at baseline, 1, 6, 12 and 36 months.
At all time points, angina was more prevalent in the stent group, although the differences getting smaller with prolonged follow-up. At three years, 19% of the stent patients and 13% of the CABG patients had angina (p<0.0001). In the group of stent patients in whom no repeat revascularisation was needed, the prevalence of angina was lower compared with those stent patients with a repeat revascularisation, but it was still higher than the CABG group at all time points (p<0.0001).
Patients with diabetes
In the stent group there was no difference between diabetics and non-diabetics in most of the SF-36 scores. Only on general health, the diabetic patients scored significantly worse than the non-diabetic patients at all time points (p<0.0001), and physical functioning decreased gradually with longer follow-up among the diabetic stent patients. Also in the CABG group, most SF-36 scores were similar among the diabetics and non-diabetics. Only a trend in worse emotional well-being was observed in the diabetics long-term.
Discussion
The main reason for treating patients with severe ischaemia is to restore the patient to as normal a life as possible. As a consequence, evidence of a meaningful benefit from the patient’s perspective is an important consideration in the comparison of treatment strategies. Both stenting and CABG resulted in significant improvements in HRQL and anginal status. Although this improvement was clear immediately following stenting, due to the major surgery, at six months HRQL after CABG was at the same level as after stenting. The first month assessment allowed us to detect both the drop in both physical and mentally function with CABG and the impact of repeat revascularisation on HRQL with stenting. Between six months and 12 months patients who underwent CABG had, in general, a better HRQL than those who underwent PCI. However, most of this difference was attributed to repeat interventions in the stent group. At one year, and up to three years, HRQL of both groups converged to each other. Furthermore, CABG surgery was associated with less angina at all time points, but again much of this difference was due to the repeat revascularisations after stenting. Therefore, with the recent introduction of the drug-eluting stents, with subsequent substantial reduction of restenosis, it is to be expected that HRQL after stenting will converge to the same as CABG.
Recently, this study reported a HRQL measurement, by means of the 5-item EuroQOL EQ-5D, beyond one year and up to three years after the procedure8. At one year after the intervention the stent group scored better on the subscales “mobility”, “anxiety and depression” and “usual activity”, but at three years all differences had diminished. However, it has been suggested that the EQ-5D is not sensitive enough as disease specific instrument and that the more well known and widely accepted 36-item SF-36 more adequately discriminates HRQL13. A limitation of this study is the lack of a disease-specific health status survey. Disease specific surveys have multiple advantages over generic surveys such as the SF-36, especially when comparing interventions within a disease state. A survey such as the MacNEW or SAQ would have captured domains most relevant to the question at hand, and could have added much to the results.
Multiple clinical trials have reported and demonstrated improvement in HRQL for both stenting and CABG1-3. However, all these studies date from the pre-stent era. Only the AWESOME and SoS investigators have reported HRQL after stenting and CABG4,5. The AWESOME trial found equivalent HRQL outcomes at 6-months and the SoS study reported improved HRQL up to 12 months after CABG.
In the diabetic subgroup of this study (n=208), no difference in 5-year mortality was found10. In general, no difference in HRQL was found between patients with and without diabetes in both the stent and CABG groups.
The present study has shown improved health status after either stenting or CABG, especially in the stent patients who didn’t undergo a repeat intervention. Many patients may refuse to undergo the greater initial suffering of CABG compared to PCI in order to achieve only similar HRQL on the long-term. Therefore, from a HRQL point of view, there seems no reason to believe that CABG should be the first choice. All the more in this drug-eluting stent era, the need of repeat of revascularisation after stenting is decreasing rapidly.
Conclusion
Both stenting and CABG resulted in a significant improvement in HRQL especially up to one year, but CABG was associated with less angina at all time points. There was a trend for better HRQL after CABG, but this difference was mainly attributed to repeat revascularisation in the stent group. Although, based purely on HRQL outcomes, there seems little reason to prefer CABG to stenting in order to provide long-term pain relief. However, the decision should be made on an individual patient basis, including balancing the larger ‘upfront’ risks of CABG with the risk of repeat revascularisation and residual angina with PCI. Furthermore, based on these findings, patients should select for themselves whether or not they would prefer the improved HRQL benefits after CABG, or whether they would prefer more angina after PCI and avoid a major operation.

