A 71-year-old male with schizophrenia and chronic subdural haematoma was transferred to our hospital in cardiogenic shock. Cardiopulmonary resuscitation combined with extracorporeal membrane oxygenation (ECMO) and an intra-aortic balloon pump (IABP) was initiated via the bifemoral artery and vein, leading to return of spontaneous circulation. Transthoracic echocardiography showed a severely stenotic, calcified aortic valve with an area of 0.6 cm2 and a mean pressure gradient of 23 mmHg. The stroke volume index was 18.5 mL/m2 and the left ventricular (LV) ejection fraction was 20%. Computed tomography confirmed severe calcification (calcium score of 3,310 Agatston units), consistent with low-flow, low-gradient severe aortic stenosis.
Given the patient’s comorbidities and haemodynamic instability, the Heart Team opted for urgent transcatheter aortic valve implantation (TAVI) using a 26 mm SAPIEN 3 valve (Edwards Lifesciences). Left subclavian access was chosen because both femoral arteries were occupied by ECMO and IABP devices. With a vessel diameter of >6 mm, aortic arch angle of 120°, and ascending aorta length of 74 mm, the left subclavian route was deemed feasible (Figure 1A). An 18 Fr sheath was inserted into the aortic arch over a SAFARI XS wire (Boston Scientific). The prosthetic valve with its delivery system was advanced into the ascending aorta, and prosthesis-balloon alignment was attempted, notably near the aortic arch (Figure 1B). However, strong resistance disrupted alignment at the balloon’s midportion, preventing withdrawal to the warning marker. The balloon could only mount two-thirds of the valve, and fracture of the unretractable distal balloon shaft was confirmed (Figure 1C, Moving image 1). Blood return from the inflation device indicated balloon rupture. Removal via the subclavian artery was impossible because of the deformed balloon obstructing passage (Figure 1D, Figure 1E).
Ultimately, the stuck prosthesis and delivery system were retrieved via the LV apex. After LV apex puncture via a standard transapical approach, the stiff wire of the SAPIEN delivery system was folded using a 10 mm gooseneck snare from the LV apical sheath (Figure 1F1) and pulled through the LV apex sheath (Figure 1F2). The distal end of the delivery system combined with the 24 Fr sheath was extracted via the left ventricle (Figure 1F3, Figure 1F4, Moving image 2). After cutting the delivery system at the balloon shaft, a new 24 Fr sheath was immediately reinserted via the apex over the stiff wire (Figure 1F5). A second 26 mm SAPIEN 3 valve was successfully deployed via the transapical route (Figure 1F6). Haemodynamic assist devices were successfully removed after TAVI with an improved LV ejection fraction of 40%. The patient was transferred to a rehabilitation hospital 1 month later.
Prosthesis-balloon alignment failure and balloon rupture during TAVI are rare, mostly reported in cases with femoral access. With left subclavian access, the limited straight segment may contribute to such complications. To prevent this, alignment should occur in a straight portion, a stiffer wire should be used, and a Certitude system (Edwards Lifesciences) should be considered. Transoesophageal echocardiography also aids in identifying causes. The bailout technique described here is not standard; access site selection and avoidance of balloon alignment near bends are crucial.
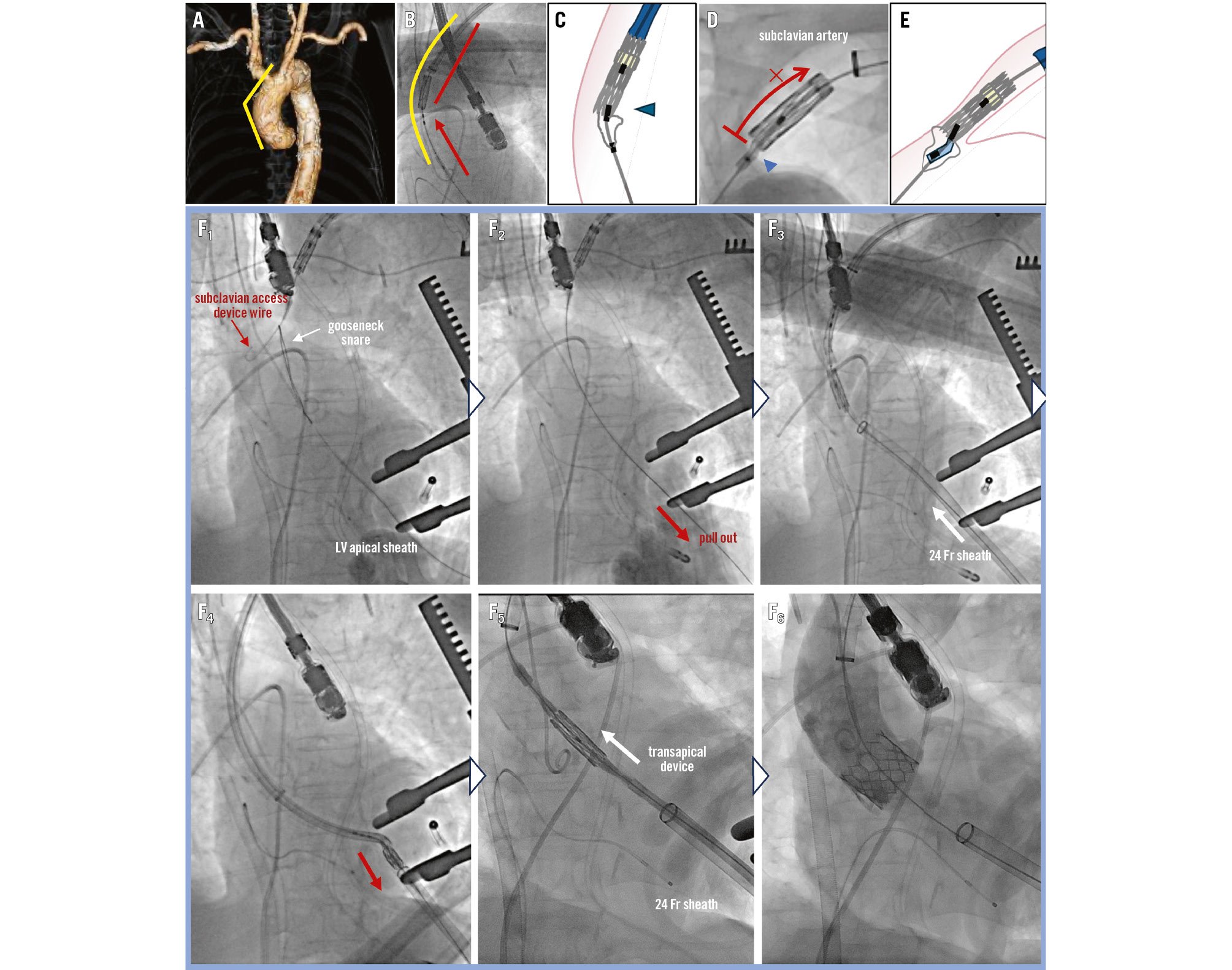
Figure 1. Procedural image of the stuck prosthesis caused by balloon alignment failure and its removal via the left ventricular apex. A) Angle of the aortic arch and ascending aorta. B) Balloon-valve alignment performed in the ascending aorta. C) Balloon injury occurred due to alignment in a curved segment, resulting in failed positioning. D, E) The deformed balloon, indicated by the blue arrowheads, could not be withdrawn via the subclavian artery. F1) The stiff wire was folded using a 10 mm gooseneck snare from the LV apical sheath. F2) The wire was pulled through. F3, F4) The SAPIEN 3 delivery system was extracted from the LV along with the 24 Fr sheath. F5) A new 24 Fr sheath was reinserted via the apical site over the stiff wire. F6) A second 26 mm SAPIEN 3 valve was deployed through the 24 Fr sheath using a transapical device. LV: left ventricle
Acknowledgements
We thank Angela Morben, DVM, ELS, from Edanz for editing a draft of this manuscript.
Conflict of interest statement
G. Nakazawa serves as a proctor for Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Prosthesis-balloon alignment failure and balloon rupture.
Moving image 2. Retrieval of the stuck prosthesis via LV apex and transapical implantation.