Abstract
Aims: Identification of subclinical high-risk plaques is potentially important because they may have greater likelihood for rupture and thrombosis. The aim of this study was to assess the relationship between in vivo coronary artery plaque composition using intravascular ultrasound virtual histology (IVUS-VH) and cardiovascular risk as predicted by clinical risk scores in patients with non-obstructive stable coronary artery disease.
Methods and results: Forty patients undergoing elective coronary angiography revealing <50% coronary artery stenoses were prospectively included. Of these, 38 (29 men; mean age 65±9 years) underwent a satisfactory IVUS-VH investigation of the affected vessel. For each patient, the 10-year risk of cardiovascular events was calculated using the Framingham and the SCORE-Deutschland risk prediction algorithms, and compared to the VH-derived plaque composition at the site of the minimal lumen area (MLA).
For both algorithms, patients at low estimated risk of events showed more fibrous tissue percentages than patients at high risk (67.4±9.7% versus 53.2±10.4% for the SCORE algorithm, and 65.6±13.4% versus 51.5±9.4% for the Framingham algorithm, p=0.002 and p=0.004, respectively). Plaques of patients with higher risk showed a non-significantly higher necrotic core percentage. For the SCORE algorithm, dense calcium percentage was higher in patients with high risk compared to patients with low risk (13.9±10.4% versus 4.9±4.9%, p=0.008). The prevalence of IVUS-derived thin cap fibro-atheromas at the MLA site was higher in patients at high risk (80% of lesions in patients at high risk using the SCORE algorithm and 92% of lesions in patients at high risk using the Framingham algorithm), whereas patients at low risk had more stable plaque phenotypes (p=0.002 and 0.003 for the SCORE and Framingham algorithms, respectively).
Conclusions: In vivo plaque composition and morphology assessed by IVUS-VH were related to the cardiovascular risk predicted by established risk prediction algorithms in patients with non-obstructive coronary artery disease, suggesting a link between the higher risk for future events and the VH-derived plaque morphology.
Introduction
Sudden death and acute myocardial infarction are common occurrences of coronary atherosclerosis1,2. Most such events are related to thrombotic occlusion at the site of non-flow limiting atherosclerotic plaques in epicardial coronary arteries. Autopsy studies suggest that plaque composition plays a central role in the pathogenesis and clinical consequences of epicardial occlusion, independent of the severity of the underlying stenosis3. On the basis of knowledge of types of plaques retrospectively identified as causes of thrombosis, thin cap fibro-atheromas (TCFAs), proteoglycan-rich plaques and plaques with a calcified nodule were suspected to be high risk/vulnerable plaques4. The identification of subclinical high-risk plaques is important because they may not only have a greater likelihood of rupture and subsequent thrombosis5, but may also be an important contributor in the pathophysiology of plaque progression6.
Intravascular ultrasound (IVUS) is the gold standard for evaluation of coronary plaque, lumen, and vessel dimensions in vivo7,8. However, although visual interpretation of grey-scale IVUS can identify calcification within plaques, it cannot reliably differentiate lipid-rich from fibrous plaques8. Recently, spectral analysis of IVUS radiofrequency data (IVUS-Virtual Histology [IVUS-VH]) has demonstrated a capability to provide detailed quantitative information on plaque composition and morphology and has been validated in histopathological studies of explanted human coronary segments9.
However, so far, there is a lack of data linking in vivo plaque composition as measured with IVUS-VH and clinical outcome. Guidelines on prevention of coronary heart disease use predicted 10-year risk of cardiovascular events to identify candidates for risk factor modification10,11. Published primary prevention risk-scoring methods use equations derived from large cohort studies, such as the European Systematic Coronary Risk Evaluation (SCORE) Project12 and the US Framingham Heart and Offspring Studies13 to calculate the estimated risk of cardiovascular events. In the present study, we evaluated the relationship between in vivo coronary artery plaque composition using IVUS-VH and cardiovascular risk as predicted by established risk prediction algorithms in patients with non-obstructive stable coronary artery disease.
Methods
Study protocol and patient enrolment
This was an investigator-driven, prospective, observational study, conducted at the Heart Centre of the Segeberger Kliniken GmbH in Bad Segeberg, Germany. A total of 40 patients referred for elective coronary angiography for suspected coronary artery disease (based on symptoms and/or a positive exercise test) and having non-obstructive (< 50%) coronary artery stenoses were included in this study. All plaques had to be de novo, angiographically non-significant, proximally located in a major epicardial coronary artery, and judged suitable for safe IVUS pullback (absence of extensive calcification and severe vessel tortuosity). According to the protocol, only one vessel was evaluated per patient. Patients with previous coronary or cerebrovascular events were excluded from this study, because all risk scores are validated only for primary prevention of cardiovascular events. The study complied with the Declaration of Helsinki, the study protocol was approved by the local ethics committee, and all patients provided written informed consent.
Cardiovascular risk factors, laboratory parameters and medications
In all included patients, demographics, cardiovascular risk factors, medications, and results of key laboratory tests were prospectively recorded. Tabulated cardiovascular risk factors and parameters included sex, age, body mass index (BMI), systolic blood pressure, serum total cholesterol level, serum LDL cholesterol level, serum HDL cholesterol level, serum triglyceride level, history of smoking during the previous 12 months, family history of coronary artery disease (myocardial infarction of first-degree relative <60 years of age), and diabetes mellitus (known diabetes or repeated fasting blood glucose levels >126 mg/dl). Plasma concentrations of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides were measured by standard enzymatic methods.
Cardiovascular risk assessment
The 10 year risk of cardiovascular events was calculated using the Framingham score and the SCORE risk assessment system.
The Framingham score was calculated by using an algorithm previously described11. This score considers sex, age, total cholesterol, HDL cholesterol, systolic blood pressure, and smoking. The Framingham score is based on data from a sample of the Framingham Heart and Offspring studies13. It was used to predict the 10-year risk of coronary events (fatal/nonfatal myocardial infarction or sudden death).
For patients below the age of 70 (n=26), the SCORE risk was determined from a risk assessment algorithm previously described12. The SCORE risk assessment system considers sex, age, total cholesterol, HDL cholesterol, systolic blood pressure, and smoking. We used the recently published tables for the German population (SCORE-Deutschland) on the basis of total/HDL cholesterol levels14. These specific risk tables were developed within the framework of the European HEARTSCORE project. The representative national health survey of 1998 and the official cardiovascular mortality statistics of Germany for the year 1999 form the basis of the calculations for SCORE-Deutschland14. It was used to predict the 10-year risk of fatal cardiovascular events12.
IVUS-VH acquisition and analysis
Details regarding the validation of the technique on explanted human coronary segments and in vivo post-atherectomy have been previously reported9,15. Briefly, IVUS-VH uses spectral analysis of IVUS radiofrequency data to construct tissue maps classifying plaques into four major components. In preliminary in vitro studies, four histological plaque components (fibrous, fibrolipidic, necrotic core, and calcium) were correlated with a specific spectrum of the radiofrequency signal9, and were assigned colour codes. Densely calcified, fibrous, fibrolipidic, and necrotic core regions were labelled white, green, greenish yellow, and red, respectively. In addition to compositional data, IVUS-VH software also provides geometric data of the vessel.
IVUS-VH data were acquired after intracoronary administration of nitrates by means of a continuous pullback (0.5 mm/s) with a commercially available mechanical sector scanner (Eagle-Eye 20 MHz catheter, Volcano Therapeutics, Rancho Cordova, California, USA) by a dedicated IVUS-VH console (Volcano Therapeutics). The IVUS-VH data were stored on a DVD for off-line analysis, which was performed by an experienced analyst who was blinded to the baseline clinical and lesion characteristics. IVUS B-mode images were reconstructed from the RF data by customised software (IVUSLab, Version 2.0, Volcano Therapeutics). Subsequently, semi-automatic contour detection of both the lumen and the media-adventitia interface was performed using cross-sectional views to provide geometrical and compositional data. To account for catheter to catheter variability, the acquired radiofrequency data were normalised by a technique known as ‘’blind deconvolution’’, an iterative algorithm that deconvolves the catheter transfer function from the backscatter, thus enabling automated data normalisation16,17.
In this study, compositional data are expressed as absolute area (in mm2) and relative percentage of the plaque cross sectional area (CSA) corresponding to each plaque component at the site of the minimal lumen area (MLA). Percent plaque burden of the MLA site is reported as the external elastic membrane (EEM) area obstruction ([EEMareaMLA – LumenareaMLA/ EEMareaMLA] x 100). Remodelling index (RI) was calculated as the EEM CSA at the minimal lumen site divided by the proximal reference EEM CSA. Positive remodelling was defined as a RI > 1.05.
In accordance with previously reported data, we classified lesions as pathological intimal thickening (mainly fibrotic- fibrolipidic tissue, with the necrotic core constituting 0% to < 3% of the CSA), fibrocalcific lesions (featuring mainly fibrotic plaques, with some calcification and a necrotic core occupying between 3-10% of the CSA), fibrous cap atheroma (necrotic core-rich [> 10% CSA] plaques with overlying fibrous tissue), and IVUS-derived thin cap fibro-atheroma (necrotic core-rich [> 10% CSA] plaques with no overlying fibrous tissue)18,19 (Figure 1).
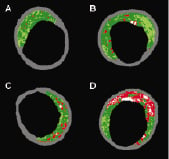
Figure 1. Morphological plaque classification with intravascular ultrasound virtual histology. Minimum lumen area (MLA) sites showing the different plaque phenotypes using intravascular ultrasound virtual histology. MLA sites showing (A) pathological intimal thickening, (B) fibrocalcific, (C) fibro-atheromatous, and (D) IVUS-derived thin cap fibro-atheromatous lesions (refer to text for detailed definitions).
To classify lesions, these criteria had to be met at the MLA frame plus the immediate distal and proximal cross sectional frames, with a plaque burden of > 40% in all three frames18,19.
Statistical analysis
Data evaluation was performed using a statistical software package (SPSS 13.0, SPSS Inc., Chicago, Illinois, USA). No formal sample size was calculated as this was meant to be a hypothesis generating analysis. Discrete variables are presented as counts and percentages. Continuous variables are presented as mean values±SD. The frequencies of categorical variables were compared using Pearson’s chi-square test. Mean values for continuous parameters were compared using the Student t test or by one way analysis of variance. Patients were grouped according to their 10-year Framingham cardiac event risk into a “low risk” group (estimated 10-year hard event risk <10%), an “intermediate risk” group (10% to 20%), and a “high risk” group (>20%)11. Patients were grouped according to their 10-year SCORE cardiac event risk into a “low risk” group (estimated 10-year fatal event risk <5%) and a “high risk” group (> 5%)10. Multiple logistic regression analysis with a stepwise elimination approach was performed to assess independent predictors of IVUS-derived thin cap fibro-atheromas (IDTCFAs) at the MLA site. A 2-tailed p value <0.05 was considered to represent a significant result.
Results
From February 2006 to January 2007, 40 consecutive patients were included. Two patients were subsequently excluded from the final analysis because of an incomplete IVUS pullback. Thus, 38 patients (29 men), age 43 to 79 years (mean age 65±9 years) constituted the final patient population. Their baseline characteristics are provided in Table 1.
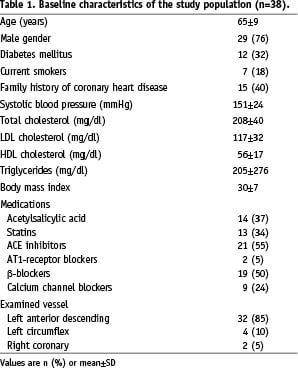
The study vessel was the left anterior descending in the majority of patients (32 patients, 85%), the left circumflex in four (10%) and the right coronary artery in two (5%) patients. Overall absolute and relative values of plaque composition at the MLA site are presented in Table 2.
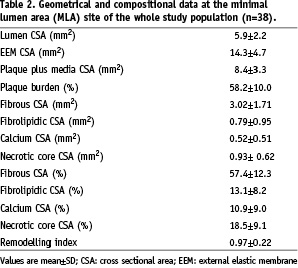
The predominant (57%) plaque component was fibrous tissue.
Estimated risk of clinical events and IVUS-VH data
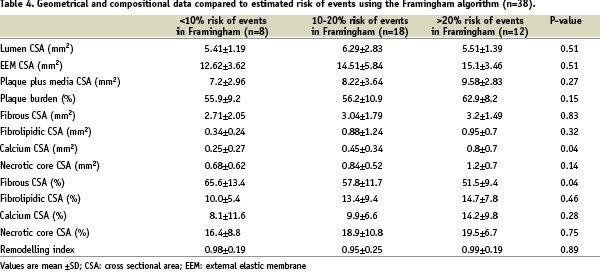
For the two risk algorithms (SCORE and Framingham), absolute and relative plaque composition at the MLA site were compared among patients with different estimated risk of clinical events (Tables 3 and 4).
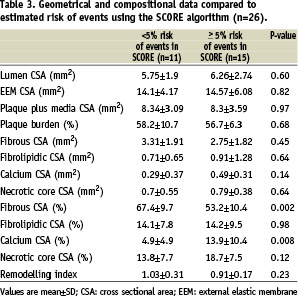
For the SCORE risk prediction algorithm, dense calcium percentage at the MLA site was significantly higher in patients with high risk compared to patients with low risk (13.9±10.4% versus 4.9±4.9%, p=0.008). Conversely, low risk patients showed more fibrotic plaques than patients with high risk (67.4±9.7% versus 53.2±10.4%, p=0.002). Plaques of patients with higher risk showed a non-significantly higher necrotic core percentage (18.7±7.5% versus 13.8±7.7%, p=0.12), and there was no significant difference in fibrolipidic percentages between patients with high and low estimated risk of clinical events (14.2±9.5% versus 14.1±7.8%, respectively, p=0.98) (Table 3).
Using the Framingham risk prediction algorithm, patients at lowest estimated risk of events showed significantly more fibrous tissue percentage at the MLA site than patients at highest risk (65.6±13.4% versus 51.5±9.4%, p=0.004). All other plaque components showed a minor trend towards an increase with increasing risk, but this was not statistically significant (Table 4).
With regard to plaque type at the MLA site, IDTCFAs comprised 80% of lesions in patients at high risk using the SCORE algorithm, and the remaining 20% where lesions of a more stable phenotype. On the other hand, only 36% of lesions in patients at low risk were IDTCFAs and 64% were more stable plaque forms (p=0.02) (Figure 2).
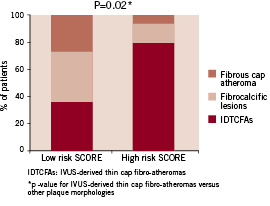
Figure 2. Lesion types and the SCORE algorithm. Bar diagrams illustrating the lesion type frequencies at the MLA site according to risk groups calculated using the SCORE algorithm.
This was also true when patients were stratified according to the Framingham algorithm, where IDTCFAs comprised 92% of lesions in patients with high risk, 61% in patients with intermediate risk, and 37.5% in patients with the lowest estimated risk of events (p for trend=0.03) (Figure 3).
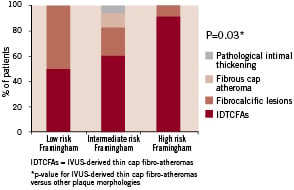
Figure 3. Lesion types and the Framingham algorithm. Bar diagrams illustrating the lesion type frequencies at the MLA site according to risk groups calculated using the Framingham algorithm.
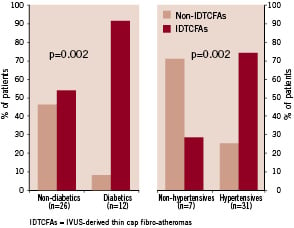
Figure 4. Lesion types in diabetic and hypertensive patients. Bar diagrams showing the lesion type frequencies at the MLA site in relation to the presence or absence of diabetes mellitus and hypertension.
For both risk prediction algorithms, remodelling index did not significantly differ between patients at different categories of calculated risk for future events (Tables 3 and 4).
Individual risk factors and plaque phenotype
As shown in figure 4, IDTCFAs at the MLA site were significantly more prevalent among patients with diabetes (p=0.002) and hypertension (p=0.002), and were significantly associated with older age (mean age 67±8 years versus 60±10 years for patients with and without IDTCFAs, respectively, p=0.03) and a higher body mass index (31.5±7.5 versus 26.5±3.3, respectively, p=0.03). On the other hand, no relation was found between gender (p=0.38), smoking (p=0.73), hypercholesterolaemia (p=0.69) or family history of coronary heart disease (p=0.54) and the presence of IDTCFAs, and LDL levels only correlated with the fibrolipidic core percentage at the MLA site (r=0.446, p=0.006).
Multivariate logistic regression analysis with a stepwise elimination approach including all clinical variables with p values <0.2 in the univariate analysis (high risk SCORE, high risk Framingham, diabetes, hypertension, older age and a high BMI) in addition to male gender, smoking, hypercholesterolaemia and a family history of coronary artery disease indicated that a high calculated risk of events using the SCORE algorithm was the only independent predictor of IDTCFAs (odds ratio 3.18, 95% confidence interval 1.05 to 9.62, p=0.019) at the MLA site of non-obstructive lesions in our study population.
Discussion
The main findings of this study were first that, at the narrowest site of non-obstructive coronary lesions, the prevalence of IVUS-derived thin cap fibro-atheromas was significantly higher in patients with high calculated risk of cardiovascular events, whereas patients with lower risk had more stable plaque phenotypes. Secondly, there were significant differences in plaque composition at the MLA site between patients with high and those with low estimated risk of events. Percentage calcium core was significantly greater in high risk than in low risk patients identified using the SCORE risk prediction algorithm, whereas a converse trend was observed for fibrotic content using both the Framingham and SCORE algorithms. Percentage necrotic core tended to be greater in higher risk patients, though this did not reach statistical significance.
We focused on analysing plaque morphology and composition at the MLA sites of non-obstructive coronary lesions, though it has been previously reported that plaque rupture rarely occurs at the site of the MLA, and that the VH-derived plaque composition is significantly different between the MLA site and ruptured plaques20. However, pathological studies have shown that plaques that do rupture are significantly more obstructive than non-ruptured plaques21. Moreover, in a recently published study by Hong et al, significant differences in the relative plaque composition of patients with unstable versus stable coronary artery disease were noted when the MLA site was analysed. These differences almost disappeared when the analysis was extended to a 10 mm segment surrounding the MLA site22. Analysis of long segments and the inclusion of less diseased segments might therefore obscure differences in highly diseased coronary segments when plaque composition and morphology is being analysed.
The thin cap fibro-atheroma
At present, the most detailed evidence about the plaque nature causing coronary thrombosis and rapid lesion progression is largely derived from autopsy studies23,24. These post-mortem observations have documented several characteristic histological patterns that form substrates for sudden death related to epicardial coronary occlusion, of which the most common is TCFA6,24. Until recently, no technique could identify TCFAs in vivo. However, spectral analysis of IVUS radiofrequency data has demonstrated potential to provide detailed information both on overall plaque composition and on the anatomic relation of specific plaque components to the lumen of the vessel9. Using IVUS-VH, Rodriguez-Granillo et al defined an IVUS-derived TCFA as a lesion fulfilling the following criteria in at least three consecutive frames: 1) necrotic core > 10% without evident overlying fibrous tissue and 2) plaque atheroma volume > 40%19. Because the axial resolution of IVUS-VH is between 100 to 150 µm, they assumed that the absence of visible fibrous tissue overlying a necrotic core suggests a cap thickness of below 100 to 150 µm, and used the absence of such tissue to define a thin fibrous cap19. Using this definition, important findings that are known from histopathology were also confirmed with VH in vivo. It has been shown that these plaques are more frequent in patients presenting with acute coronary syndromes than in those with stable angina19, that they are typically located in the proximal third of the coronary arteries25, and that they are commonly associated with positive vessel remodelling18. Our study further identified IDTCFAs to be more prevalent at the MLA site of patients at high estimated risk of cardiovascular events, suggesting that the higher risk for future events may be at least partially derived from a more complex plaque phenotype in this patient cohort, though remodelling patterns were not different. Nevertheless, using the Framingham score, IDTCFAs comprised more than 60% of lesions in patients at intermediate risk of events (estimated 10-year hard event risk 10-20%). Analyses of modern risk prediction algorithms have shown that – in absolute figures – most acute cardiovascular events occur in patients at intermediate risk26. Especially in this group of patients, plaque characterisation with IVUS-VH may have an additive value in refining risk stratification of subclinical unstable atherosclerotic coronary artery disease by providing means to identify high-risk plaques.
Coronary calcium and the risk of cardiovascular events
On the other hand, coronary calcium is intimately associated with coronary atherosclerotic plaque development. Based upon histopathological and electron-beam computed tomography (EBCT) studies, it has been argued that calcium is characteristic of stable coronary artery disease, and that plaque rupture and acute coronary syndromes frequently occur in the absence of coronary calcium27,28. However, Farb et al29 reported that calcium is a frequent feature (in almost 70% of subjects) of plaque rupture and is less frequently associated with plaque erosion. Burke et al30 classified culprit plaques in 108 victims of sudden cardiac death as “stable” (n=520), “erosion” (n=533), “acute rupture” (n=537), and “healed rupture” (n=518). The most frequently calcified plaques were acute ruptures (80%). The most extensively calcified plaques were healed ruptures. Eroded plaques displayed the lowest frequency and extent of calcium. Moreover, with the introduction EBCT, which allows the quantitative assessment of coronary artery calcification in the total coronary tree, some studies have shown that EBCT-detected coronary calcification is a powerful predictor of future coronary events in symptomatic31 and asymptomatic patients32. However, the imaging of coronary calcification by EBCT cannot be used to identify a localised unstable plaque, and has a limited predictive value in identifying potential sites of plaque-related complications, and therefore cannot direct local therapies. In our study, using a localised IVUS-VH examination of non-obstructive coronary plaques, patients at higher estimated risk of events showed more calcifications at the MLA site than patients with low risk, further suggesting a link between coronary calcium and the overall risk of cardiovascular events. Though the available data about the role of coronary calcium in identifying “high risk plaques” are controversial, it surely has the potential to identify a “higher risk patient”.
Risk scores
The risk-scoring methods studied in the present report were derived from the European SCORE Project12 and the US Framingham Heart and Offspring Studies11. As these scores have been validated for primary prevention of coronary events, we only included patients who had no history of myocardial infarction or cerebrovascular disease. However, all our patients had established, though non-obstructive, coronary artery disease. We consider applying these risk scores in this patient population reasonable, especially in the absence of a validated risk score for secondary prevention33. All patients examined in the present study probably have an absolute risk of clinical events that is higher than suggested by the nominal results of the two algorithms. Nevertheless, we were able to demonstrate with both algorithms a significant relationship between estimated risk of clinical events and the morphology and composition of atherosclerotic plaques as measured with IVUS-VH.
We used the recently published tables for the German population (SCORE-Deutschland) on the basis of total/HDL cholesterol levels14. Therefore, perhaps not surprisingly, we observed a particularly strong relationship between plaque composition and estimated risk of clinical events using the SCORE algorithm. Conversely, the Framingham risk score showed relationships with the current IVUS-VH data that were less strong but still significant. This suggests that risk scores derived from population studies may have a limited applicability when applied to another population with a different risk profile from a different geographical region33. Of note, SCORE and Framingham algorithms used different endpoints (fatal versus combined fatal and nonfatal endpoints). Since the SCORE chart predicts fatal events, the threshold for being at high risk was defined as > 5%, instead of the >20% in the Framingham score, where a composite coronary endpoint is being used10. Nevertheless, our findings were quite similar among the two risk scores.
VH and risk stratification
Finally, the clinical implications of these observations are less certain than their scientific implications. The ongoing PROSPECT trial is a large prospective natural history study, which will provide important information on the clinical significance of IVUS-VH analysis and its possible value in refining risk stratification in patients harbouring non-obstructive atherosclerotic plaques. In this patient population, the question will be not whether, but how aggressively we should treat and follow-up these patients to prevent future cardiovascular events.
Study limitations
The present was a pilot, observational study that included a small population. Accordingly, a potential selection bias cannot be disregarded. Only a short segment of the coronary tree was evaluated, therefore this may not be representative of the whole coronary tree. In addition, classifying lesion types by this technique needs further histopathological validation, which renders our observation only exploratory. Moreover, the IDTCFA definition adopted throughout this manuscript has been originally identified using a catheter with a different frequency (30 MHz)19, and therefore slight differences in the relative content of each plaque component (particularly of necrotic core) cannot be excluded. Accordingly, interpretation of our findings must be done cautiously. However, a significant relation was found by using this classification. Although histopathological classification remains the ideal, spectral analysis of IVUS radiofrequency data may have the potential to provide detailed information regarding in vivo tissue characterisation and plaque morphology.
Conclusion
In this small clinical study, in vivo plaque composition and morphology assessed by IVUS virtual histology were related to the cardiovascular risk predicted by established risk prediction algorithms in patients with non-obstructive stable coronary artery disease. At the MLA site of non-obstructive coronary lesions, plaques of patients at higher risk for future events were more calcified and less fibrotic than those of lower risk patients. Furthermore, IVUS-derived thin cap fibro-atheromas were more prevalent in high risk patients, suggesting a link between the higher risk for future events and the VH-derived plaque morphology. Larger studies are needed in order to evaluate the prognostic value of these findings in natural history studies.
Acknowledgement
Our thanks to the clinical research group at the Herz-Kreislauf-Zentrum Segeberger Kliniken GmbH, especially Mrs. Daniela Schuermann-Kuchenbrandt, Mrs. Kirstin Kassner and Mr. Guido Kassner.
This study was supported by an educational grant from Novartis, Germany.
Excerpt from a reviewer
The manuscript of Abdel-Wahab explores, in patients with non-obstructive coronary lesions, the relationship between plaque composition at the minimal lumen area and established risk scores such as Framingham and SCORE. In a small population, plaque composition, assessed by a validated technique, was related to the estimated risk. The findings seem to be intriguing although the potential clinical implications are difficult to foresee.
The main limitation of the manuscript is the fact that they report data only of the minimal lumen area (MLA). Plaque rupture rarely occurs at the site of the MLA, but most probably proximal or distal to the MLA. Furthermore, plaque composition is significantly different between the MLA and ruptured plaques. This has been published elsewhere. Therefore it might have been important to report data of a Region Of Interest of a certain length (i.e. 30 mm) that would have been more representative of the composition of (non-obstructive) plaques of stable patients throughout the coronary tree.
Although the authors acknowledge the preliminary characteristics of the study (“pilot”), linking population-based classifications such as Framingham to such as small sample size seems a little speculative.

