Abstract
Aims: The goal of this study was to clinically evaluate the effectiveness of a new coronary stenting approach for bifurcation lesions designed to provide adequate main and side-branch ostial scaffolding and provide a simplified technique.
Methods and results: The technique was used in 100 consecutive patients with suitable bifurcation lesions. Sequential placement of two stents was performed in all patients, resulting in complete coverage of the bifurcation ostium and carina with minimal crushing of a small portion of the side-branch stent. Clinical follow-up was done for a six months period. The rate of clinically driven target vessel revascularisation at six months was 4%. One patient died during follow-up. Subacute thrombosis occurred in two patients.
Conclusions: Treatment of bifurcation lesions using this new approach is feasible, with a low rate of procedural and clinical events. Larger trials with angiographic follow-up are necessary to prove the potential advantage of this approach relatively to the currently used techniques for the treatment of coronary bifurcations.
Abbreviations list
DES: Drug-Eluting Stents
BMS: Bare-Metal Stents
LAD: Left Anterior Descending artery
LCX: Left Circumflex artery
TVR: Target Vessel Revascularisation
Introduction
Bifurcation lesions occur in more than 20% of coronary angioplasty interventions1. Percutaneous treatment of coronary bifurcation lesions pose a number of technical challenges to the interventional cardiologist. Each lesion has to be approached with its own, targeted solution in the context of the clinical picture, anatomy, and pathology. A number of established techniques are available in order to achieve acceptable clinical outcomes. Although the most common approach is the provisional stenting of the side-branch, various techniques that use two stents have been described and include the simultaneous ‘kissing stent’ technique, as well as approaches in which there is sequential placement of the stents (‘Y’,’T’, “crush”, ‘V’, and the ‘culottes’ technique). Novel “bifurcate” stent designs are developed to allow complete coverage with a single stent of both branches, but their testing is in a preliminary stage. Furthermore, difficulties in anatomy combined with reduced deliverability, still inhibit the widespread use of these dedicated devices.
In this report we describe our experience with a new approach for the treatment of bifurcation lesions with a new simplified technique that involves the sequential positioning of two stents, first in the side-branch (SB) and second in the main branch (MB). The main aim of this technique is to provide a complete coverage of the bifurcation lesion and of the carina with a relatively small portion of the main branch, only distally to the bifurcation, being scaffolded with a triple layer of stent. As a result, this procedure can be characterised as “a modified T stenting technique with minimal crush”. We report the clinical outcomes in the cohort of patients in which we have performed it.
Methods
Description of the technique
Our technique is a new T stenting approach that briefly can be described as follows (Figures 1-3): After the predilatation of the bifurcation, two wires are inserted in both branches of the bifurcation
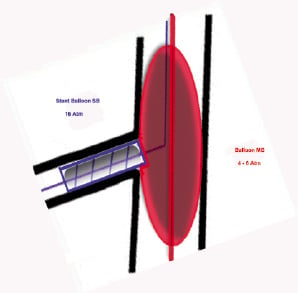
Figure 1. A stent is positioned in the side-branch, “cushioned” against a balloon being at the same time positioned in the main branch and inflated at low (4-6) Atm, followed by stent deployment at about 16 Atm. Following sequential inflations in the side – main branch, complete coverage with stent struts of the side-branch is achieved, leaving no gaps.
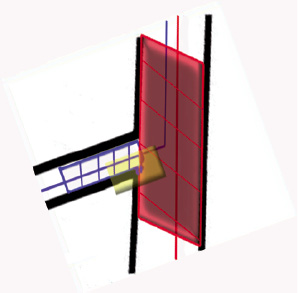
Figure 2. After complete removal of the side-branch delivery system, main branch stent deployment at high pressure follows.

Figure 3. Magnification of the area of “crushing”: a small portion of the proximal part of the side-branch stent at the distal carina is deployed and “crushed” inside the main branch (minimal distal crush).
lesion. Then a stent in the side-branch and a balloon in the main branch are advanced at the site of bifurcation. In order to ensure adequate scaffolding of the side-branch ostium, the side-branch stent is slightly pulled back, so that a small portion of the distal part of its proximal end is deployed inside the main branch. The stent is then correctly positioned at the side-branch ostium, “cushioned” against the balloon in the main branch during a low inflation of the MB balloon (~ 4 Atm.), followed by side-branch stent deployment at about 16 Atm. Thereafter, a sequential high-pressure inflation of the side and of the main branch is performed with these two balloons, in order to create a small detachment of the side-branch stent struts and to create a wide opening towards the side-branch. This should provide complete coverage of the side-branch ostium, leaving no gaps. After complete removal of the side-branch delivery system (included the wire), a stent is positioned in the main branch and deployed with high pressure, resulting in a small crush of the proximal part of the side-branch stent (only at the distal carina, [Figure 3]). It is important to stress here that this technique does not necessitate a final kissing balloon dilatation in order to open the struts of the main branch stent to facilitate the crossing towards the side-branch. Therefore no recrossing to the side-branch and final “kissing balloon” techniques were performed. This approach is completely different from previous described “modified T” techniques because of the double but sequential SB / MB stenting without post-stent dilatation procedures.
All patients were pretreated with aspirin and clopidogrel. A 300 mg loading dose of clopidogrel before the index procedure was administered, if patients were not pretreated. Initially, all patients received intravenous unfractionated heparin (70 IU/kg). Administration of glycoprotein IIb/IIIa inhibitors was left to the operator’s discretion. Every patient was on maintenance aspirin therapy and clopidogrel was administered for 12 months following DES implantation and for six months following bare-metal stents (BMS) implantation.
Study population
Patients with lesions involving a bifurcation lesion with a side-branch equal to, or greater than, 2.0 mm in diameter were considered eligible for the study. The angle between main and side-branch should be more than 45-50°.
A bifurcation lesion was defined as diameter stenosis > 50% involving the main parent vessel proximal or distal to the origin of a major (>2.0 mm in diameter) side-branch, with or without involvement of side-branch ostium, based on visual assessment on the angiogram2.
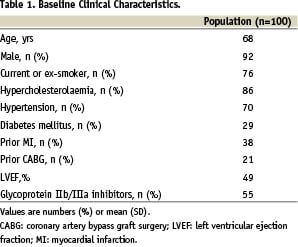
The clinical characteristics of our patients are summarised in Table 1. Of the patient population, 28% were diabetics.
Clinical definitions and follow-up
Clinical follow-up was performed by telephone contact or office visit throughout the entire follow-up period at one and six months after the index procedure.
Major adverse cardiac events (MACE) at six months follow-up was the primary end-point of our registry, and was defined as: cardiac death or myocardial infarction and target vessel revascularisation (TVR) either percutaneous or surgical. Q-wave myocardial infarction was diagnosed on the basis of the development of new Q-waves of more than 0.04 sec duration in two or more contiguous leads, with an increase of the creatine kinase level to more than twice the upper limit of the normal range and an elevated MB isoform level. A non-Q-wave AMI was defined as elevation of CK levels >2 times the upper limit of the normal value with an elevated CK-MB level in the absence of pathological Q-waves. TVR was defined as a repeat intervention to treat a luminal stenosis within the stent or in the 5 mm distal and proximal segments adjacent to the stent. Procedural success was defined as angiographic success with TIMI-3 flow both in the main and side-branch without the occurrence of death, emergency CABG, repeat PCI of the target vessel, and acute myocardial infraction (AMI) before discharge.
Stent thrombosis was defined as an acute coronary syndrome with angiographic documentation of either vessel occlusion or thrombus within or adjacent to a previously successfully stented vessel or (in the absence of angiographic confirmation), AMI in the distribution of the treated vessel not clearly attributable to other causes. According to the timing of the events, three categories of stent thrombosis were specified: intra-procedural; subacute stent thrombosis (from the end of the procedure to 30 days) and late stent thrombosis (> 30 days)3-5.
Statistical analysis
Continuous variables are presented as mean (SD) or median with interquartile ranges and categorical variables as frequencies (%).
Results
Baseline and procedural characteristics
A total of 100 consecutive patients with suitable bifurcation lesions were treated between November 2004 and December 2005. Baseline lesion characteristics are shown in table 2.
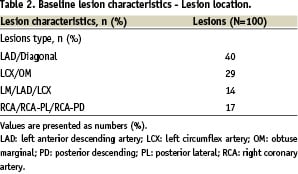
Baseline bifurcation anatomy was classified according to MEDINA classification (Table 3).

Of the lesions, 14% were located at the distal left main bifurcation. There was involvement of the main branch in every case that was treated, while the side-branch was diseased in 85% of cases. Quantitative coronary angiography analysis results before and after the procedure are shown in Table 4.

Angiographic follow-up was not routinely performed in our patients. IVUS was used in a minority of our cases, according to operator’s judgement and in order to assess only the deployment of the main branch stent. Due to a local restrictive policy on the use of DES, the majority of patients were treated with a non-DES stent. As a result only 18 patients received sirolimus-eluting stents (Cypher®, Cordis J&J) in both branches, seven patients received a Cypher® stent at the main vessel and a bare-metal stent at the side-branch and three patients received a BMS in the main vessel and a Cypher stent in the side-branch. Direct stenting was performed in 68% of the side-branch lesions.
Clinical outcomes
Procedural success was noted in all of the cases. Clinical follow-up at 6 months was available in the whole patient population. Clinical outcomes are summarised in Table 5.
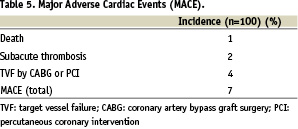
One 85-year old patient who was treated with two BMS in Left Main/LAD/LCX bifurcation, was found dead four days after the procedure while at home. Two patients who were treated with two BMS suffered a subacute stent thrombosis in the SB and were treated with a repeat PCI without having further complications. The rate of TVR at six months was 4%. In detail, there were two cases of TVR at the main branch, one in a patient with BMS and one in a patient with Cypher® stent. There were also two cases of TVR at the side-branch again equally distributed in a patient with a BMS and in a patient with a Cypher® stent. There were no TVRs in the group that received a Cypher® stent in the main vessel and a bare-metal stent in the side-branch. There was a TVR at the side-branch in one out of the three patients who received a bare-metal stent in the main vessel and a Cypher® stent in the side-branch.
Discussion
Even in the current era of drug-eluting stents (DES) and of special dedicated bifurcation stents, the most appropriate method for treating lesions at bifurcations remains to be defined. Follow-up data demonstrates a rather poor clinical outcome, due to recoil and plaque shift at the origin of the side-branch. Thus with conventional bifurcation stent techniques restenosis rates higher than 30% have been reported. In part, all these alternate strategies have developed as no single technique has been found to be superior to the rest.
Dedicated bifurcation stent designs are being developed (Invatec Twin rail, Devaxx Acces, Frontier stent™, SLK-View™)6-8. Their main advantage is that the second lumen of their delivery system is always open and protects the ostium of the side-branch during stent deployment, so that additional treatment of the side-branch can be performed optimally. In addition, less metal component and no stent overlap may lead to favourable long-term outcome. Furthermore, there is no destruction of stent struts in the parent vessel. These stents seem offer more promising treatment for treating bifurcation lesions, but there are also some limitations: i) the deliverability of the currently used dedicated stents is rather limited, especially in cases of difficult anatomy; ii) the use of most of these stents increases the duration of the procedure considerably; and iii) a great amount of expertise is required to ensure their optimal deployment. As technology proceeds and the experience of the operators grows, these problems are likely to be surpassed in the near future.
The emergence of drug-eluting stents offered considerable hope in improvement of outcomes in bifurcations treatment, showing reduction of the incidence of main vessel restenosis and their usage seems to result in lower event rates9-12. Until recently though, most of the currently available data regarding the use of DES in bifurcation lesions, are in the form of single centre case reports or series, so further evidence-based evaluation is required before a routine use of DES in bifurcation lesions can be finally recommended13-15. A recent randomised trial that compared BMS with sirolimus eluting stents showed a better clinical outcome with Cypher®.16 It is noteworthy that the results regarding side-branch restenosis are not encouraging, as the occurrence of restenosis at the ostium of side-branch remains as high as 21%12,17-19. Furthermore, according to a recently published registry that examined the outcomes of DES usage in treating distal left main bifurcation disease, the cumulative incidence of MACE was 30% in an 18 month-period20. A rising problem, while using DES in bifurcations with current techniques, is the relatively high incidence of stent thrombosis (about 3,5%)3,5-6,17. A recent study using crush technique and DES in bifurcations reported an intraprocedural stent thrombosis of 1.7%, and a subacute stent thrombosis rate of 2.8% (2% in sirolimus-eluting stents and 4% in paclitaxel-eluting stents).12 “Crush” techniques may lead to an increased local drug delivery at the proximal part of the parent vessel, with subsequent intense impairment of endothelial function, therefore increasing the risk of thrombosis 21. Indeed, bifurcation lesions were found to be an independent predictor of DES thrombosis3. Prolonged antiplatelet treatment in cases of bifurcations treated with DES seems therefore absolutely necessary, while its optimal duration is not yet known14. To reduce the risk of thrombotic events with these techniques, also a more liberal usage of glycoprotein IIb/IIIa inhibitors should be considered17. Therefore, because of these unresolved issues regarding the use of DES in bifurcation lesions, as well as a local restrictive policy, we decided to implant BMS (always using the new generation chromium-cobalt stents!) in the majority of our patients and not DES. The use of DES was limited to the diabetic subpopulation and/or a vessel diameter less than 2.5 mm in the SB.
Multiple stenting techniques, each with their own advantages, indications and problems, have been used to treat bifurcation lesions22-24. Stenting of the main vessel only is currently thought to be the best option even in those lesions in which the diameter of the side-branch is > 2.5 mm19,24-26. Although stenting of the main vessel with provisional stenting of the side-branch is the predominant current technique, in many of these procedures the suboptimal final result at the side-branch, when this is a large vessel with a sufficient area of distribution, necessitates the positioning of a second stent27. Also a single-stent strategy should not be applied in most of distal left main bifurcations, or in cases of depressed left ventricular function where achievement of complete angiographic outcome is desirable, as well as when the side-branch lesion is too long, calcified and tortuous, making it unlikely that an acceptable result will be obtained with balloon angioplasty only28.
In a randomised trial using bare metal stents in bifurcation lesions, comparing single stent with two stents technique, 57% of these cases initially planned to be treated with one stent crossed over to the double-stent group due to unsatisfactory angiographic results.27 According to our experience, the provisional side-branch stenting technique still takes the lead in more than 50% of cases to the final placement of a side-branch stent because of suboptimal angiographic results (e.g., dissection, plaque shift and occlusion of a large side-branch may occur, resulting in risk of ischaemia – and thus persistent angina – of a large area of the myocardium). When the one-stent technique fails to provide a satisfactory result at the side-branch, a “reverse crush” technique follows, that leads to the positioning of a second stent in the side-branch, through the struts of the first one. It is obvious that this technique is laborious and can not be recommended as the preferred technique for positioning of two stents in a bifurcation lesion. Furthermore, all techniques that include stenting first of the main branch and a “jailed” wire in the side-branch have the potential danger of rupture of the “jailed” wire, especially when using hydrophilic wires.24,28 Therefore, the need for a successful and simplified two-stent bifurcation technique remains, and this is what led us to this new approach.
After an overview of all the current techniques for treating bifurcation lesions, some important issues should be pointed out:
First, the side-branch is the weak link of the chain in terms of higher risk of restenosis. Suboptimal coverage by struts and drugs (in the case of DES) that results in uncovered gaps at the ostium of the side-branch, is the major contributing factor to side-branch restenosis. In addition to this, plaque shifting from the main branch, as well as extended crushing of the proximal segment of the side-branch stent which may result in malapposition and inefficiency of the drug eluting stent (crush technique), also contribute to side-branch restenosis.
Second, stent thrombosis is a question when using techniques with a lot of stent overlap at the proximal part of the main branch (crush, culotte), not only in earlier studies but also during the DES era5,6,24,29-30.
Third, recrossing the side-branch after stent implantation in the main branch either for the positioning of the side-branch stent or for final kissing balloon dilatation, is a technically demanding and laborious stage of all the current techniques. It causes an increase of radiation time and of the amount of contrast being used, which are of high importance when treating complex lesions in high risk patients (diabetics, renal impairment). Although use of a final kissing balloon dilatation has shown a favourable effect in the clinical and angiographic outcome when used in crush technique,12,17 the evidence in favour of a final kissing balloon dilatation is not necessarily applied in our technique where the “crushing” of stents is minimal. Furthermore, in a bench study that evaluated DES platforms while using the provisional stenting technique, the internal crush and the culotte techniques, kissing balloon inflations in crush technique were found to be a cause of stent distortion. It was found that while these inflations expanded the stents well, the stent struts at the distal margin of the ostium were pushed into the main branch. This distortion was not found to be due to the sequence of balloon deflation30.
We believe that our “T”-approach gives adequate answers to these issues, as it provides – theoretically – full coverage of the ostium of the side-branch, leaving no gaps at the side-branch vessel ostium. Overlap of stents and crushing at the main branch is minimal, because a very limited portion of the main branch only distally to the bifurcation is being scaffolded with a triple layer of stent. There is no stent overlap elsewhere in the bifurcation, diminishing the risk of thrombosis.
Bifurcation lesions carry a risk of side-branch occlusion because of plaque redistribution, the so-called plaque shift across the carina of the bifurcation. Side-branch recrossing for final kissing balloon dilatation is not required in our approach, so that the stretching and deforming of the main stent cells is avoided, thus preserving the geometry of the stent at the main branch. Avoiding final kissing balloon dilatation also makes this technique less technically demanding and time-consuming as was previously explained.
The clinical follow-up of the patients in our study reaffirms the theoretical advantages of this technique, as noted, a rather low incidence of clinical events after a six months period. In 18% of our patients, a drug-eluting stent (Cypher®) was placed and it was a promising finding that both bare-metal as well as sirolimus-eluting stents were rather safe when used according to our approach, although a direct comparison between these two platforms was not the purpose of our registry. Older studies using BMS in bifurcation lesions have shown a rather high incidence of restenosis with TLR rates of about 30%.26,32 In our study though, the new generation of cobalt-chromium bare metal stents were used (Driver® -Medtronic, Skylor® -Invatec) in which efficacy data, especially in bifurcation lesions, is lacking. One prospective, multicentre study that evaluated the clinical safety and efficacy of the Driver cobalt-chromium alloy stent in 298 patients with non-bifurcation lesions showed quite similar results as our registry, the cumulative incidence of major adverse cardiac events was 5.7% at six months and target lesion revascularisation was 3.4% at 180 days33. Given the fact that no angiographic follow-up was performed, this might explain the low rate of TLR, besides the choice and description of this less traumatic procedural technique.
Limitations
The main drawback of our technique is that it can not be applied in angles less than 40°-50°, due to potential excessive protrusion of the stent struts of the SB stent into the lumen of the MB. Even in wider angles, though, the possibility of protrusion of the side-branch stent struts toward the side-branch lumen cannot be fully excluded even when using the “cushion technique” against the MB balloon. A final kissing balloon dilatation may have a favourable role in these cases, mainly regarding the issue of stent thrombosis. Although we describe a low rate of (sub-) acute stent thrombosis, a final kissing balloon technique might have reduced this number even further. Our reasons for not performing this have been extensively described above.
The major clinical limitation of this registry is the lack of angiographic follow-up in the majority of our patients. Follow up also did not include systematic stress testing. This could eventually have underestimated the incidence of silent ischaemia, especially in the diabetic population.
Conclusions
This study shows that in a preselected population of patients with severe bifurcation lesions that this new approach of modified T stenting with “minimal crush” was technically feasible, with a low incidence of procedural complications and clinical events after a six months follow-up period. A practical advantage is that the technique is quite safe and relatively simple to execute. It is therefore a promising strategy that should be added to the current techniques that are being used and evaluated for this purpose, with either bare-metal or drug-eluting-stents. Further evaluation of this technique is required in trials with angiographic follow-up, comparing it with other techniques that are currently being used for the treatment of bifurcation lesions.
Online data supplement
Video 1. Bifurcation RCX / MO1
Video 2. “Cushioning” SB stent against MB balloon
Video 3. Inflation SB stent 12 atm, MB balloon at 4 atm
Video 4. Inflation ostium SB stent at 18 atm
Video 5. MB balloon at 14 atm.
Video 6. MB stent at 14 atm, after retrieval of SB wire.
Video 7. No post dilatation (1) final result
Video 8. Final result (2)
Video 9. IVUS Pull back through MB stent, showing good flow towards SB and small area of crush at 4-6 o’clock

