Abstract
Aims: To test the hypothesis that intracoronary infusion of pre-oxygenated HBOC-201 during brief, total coronary artery occlusion would preserve left ventricular function.
Methods: Immediately following a successful PCI, the target coronary artery was occluded without (“dry occlusion”) –or with– infusion of pre-oxygenated HBOC-201 distal to the stent via the guidewire shaft of an over-the-wire balloon for up to three minutes at an infusion rate of 48 ml/min. A cross-over design was applied. Early signs of myocardial ischaemia were evaluated by left ventricular pressure-volume loops and intracoronary ECG. A 12-lead Holter ECG was activated before the PCI and deactivated four hours after the study period. Primary endpoints were change in left ventricular relaxation indices and in the sum of ST segment deviations.
Results: None of the measured parameters differed significantly from their respective baseline values during HBOC-201 infusion. By contrast, ejection fraction (EF), cardiac output (CO) and minimal rate of LV pressure change (dP/dTMIN) decreased significantly and the end diastolic pressure (EDP) and time constant of relaxation increased significantly during dry occlusions (P < 0.05). The end diastolic pressure-volume relationship (EDPVR) at the fixed pressure level of 30 mmHg (V30), an index of myocardial compliance, reflected greater myocardial stiffness during dry occlusions compared to occlusions with HBOC-201 infusion.
Conclusions: Intracoronary infusion of oxygenated HBOC-201 is capable of preserving left ventricular function, likely through maintenance of myocardial oxygenation. It is hypothesised, that in an acute setting, HBOC-201could serve as an oxygen bridge to reperfusion by PCI extending the “golden” time period during which permanent myocardial damage is unlikely.
Introduction
HBOC-201 is a cell-free, endotoxin-free, glutaraldehyde-polymerised haemoglobin solution produced by chemical modification of bovine haemoglobin. Initially developed as an alternative to red blood cells for anaemic surgical patients, HBOC-201 has the ability to restore tissue oxygenation in persistently ischaemic tissue. By facilitating oxygen diffusion and convective oxygen delivery, HBOC-201 may act as a direct oxygen donor and increase oxygen transfer between red blood cells and between RBCs and tissues1,2. These mechanisms could improve tissue oxygenation3, especially in post-stenotic areas that free plasma, but not RBCs, is capable of reaching. HBOC-201 can be stored at room temperature for a period of up to three years and does not require cross-matching.
Because HBOCs can deliver oxygen, they have been considered as an adjunct treatment in ACS. Studies conducted in animal models demonstrated that both the prophylactic (before induction of ischaemia) and late (after ischaemia onset) HBOC infusion are well tolerated and effective4-8.
The safety and tolerability of HBOC up to 230 ml in low to moderate risk cardiac patients scheduled for elective PCI has recently been investigated in the COR-001 trial9. This study showed that intravenous HBOC-201 administration did not compromise autoregulation of coronary blood flow, despite the known vasoconstrictive properties of this drug, or myocardial function as assessed by the left ventricular stroke work. A transient increase in the mean arterial blood pressure (MAP) and systemic vascular resistance was observed, consistent with the purported nitric-oxide scavenging activity of the drug.
The present study is a first step towards establishing the efficacy and safety of oxygenated HBOC-201 in preserving myocardial function using PCI techniques to induce brief coronary artery occlusion in humans. Additional safety information regarding intra-coronary delivery of oxygenated HBOC-201 has also been collected.
Methods
Study design
The COR-0002 pilot trial is a single-centre, phase II, placebo-controlled, crossover, single-blind study conceived to test the hypothesis that HBOC-201 administration improves myocardial “oxygenation” and myocardial function during brief coronary occlusion. Enrolled subjects underwent coronary balloon occlusion, with and without oxygenated HBOC-201 intracoronary infusion (11-12 g/dl at 48 ml/min up to 3 min). The study was approved by the Medical Ethics Committee of the Erasmus Medical Centre (Rotterdam, The Netherlands) and was performed in accordance with the International Conference on Harmonisation of Good Clinical Practice (ICP/GCP) guidelines.
Patients
Patient inclusion and exclusion criteria are summarised in Table 1.
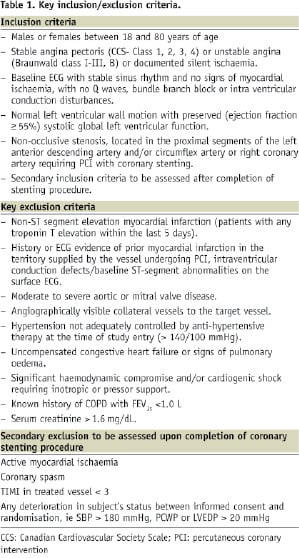
In brief, patients were eligible for the study if they were admitted for either documented silent ischaemia, stable angina or unstable angina (Braunwald class I-IIIB)10. To optimise safety and size of the area at risk, eligibility was further constrained to patients with a target lesion in the proximal part of the left anterior descending coronary artery, in the absence of associated angiographically visible collateral vessels. Further, a successful index PCI, with focal stenting of the target lesion during the same cath lab session, was required prior to initiating the study period.
The pre-PCI standard 12-lead ECG recording corresponds to the baseline for quantitative dynamic analysis of ST changes over time during the study period. Written informed consent was obtained from all patients before the initiation of any study-specific procedures, including pre-treatment sedation.
Study procedures
Data collection points and study design are depicted in Figure 1.
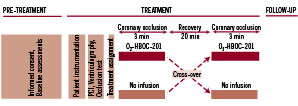
Figure 1. The COR-0002 trial was divided into three phases: a preparation period (pre-treatment phase), a treatment phase and a follow-up phase. The study period began after the lesion was successfully treated (PCI and stenting). Continuous 12-lead HOLTER ECG was recorded from pre-PCI to four hours after the study period ended (follow-up). PCI: percutaneous coronary intervention.
All subjects were followed from study inclusion to hospital discharge. An independent physician was appointed to monitor safety and welfare of the study subjects and review the clinical events during the study period.
Concomitant treatment
Standard medications used in the management of subjects with ischaemic heart disease were not withheld per study protocol with the exception of analgesics. Use of analgesics was restricted as much as possible and were not administered immediately before study drug infusion.
PREPTREATMENT PHASE
Laboratory testing, including haematology (haemoglobin, haematocrit, platelets and INR) and blood chemistry (creatinine, LDL, AST, ALT, amylase, troponin T, CK total and CK-mb), was performed at pretreatment baseline (within 24 hours of the study period) and eight hours post PCI. HBOC-201 was pre-oxygenated within 24 hours of the study period using a proprietary system designed and validated for this purpose (Figure 2).
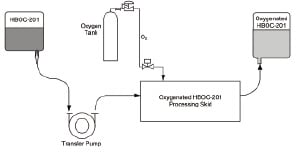
Figure 2. In vitro oxygenation system. In this closed circuit system, HBOC-201 is pumped across a liquid-gas exchange apparatus in which the gas side is supplied with a continuous stream of medical-grade oxygen. The exiting oxygenated HBOC-201 is collected into pre-sterilised bags at a concentration of 11-13 g/dl.
Continuous 12-lead Holter monitoring. On arrival in the cath lab, the patient was connected to a continuous 12-lead Holter ECG recording device which was activated before the PCI and deactivated four hours after the study period. The Holter data were sent to an independent ECG core laboratory (Cardialysis, Rotterdam, The Netherlands) where ST segment changes over time were analysed by an experienced, independent analyst who has no knowledge of the order of study treatments. ST-segment shift compared to baseline was analysed in the lead that demonstrated the most severe alterations as well as in all leads showing ST-segment changes > 1 mm (at 60 ms after the J-point).
Patient instrumentation. Vascular access was obtained using the femoral approach with a standard Seldinger technique. Usually, a 6 or 7 Fr arterial sheath was selected. Prior to starting the PCI procedure, a conductance catheter was inserted into the left ventricle by an additional 8 Fr arterial sheath (details concerning the haemodynamic data acquisition are provided below in “Left ventricular haemodynamics”). A Swan-Ganz catheter was placed in the pulmonary artery via the femoral vein for cardiac output determinations by thermal and hypertonic saline (NaCl 10%) dilution methods.
INDEX PCI PROCEDURE PHASE
An index PCI procedure was performed according to standard institutional practices. All patients were pretreated with aspirin and clopidogrel (300 mg) 2-8 hours prior to the intervention. PCI procedural success was defined as successful stent deployment in the target lesion with a residual percent in-stent diameter stenosis of < 15% and TIMI 3 flow of the target vessel without the need for bypass surgery and in the absence of death.
THE STUDY PHASE
Upon successful completion of the index PCI procedure, a short over-the-wire (OTW) balloon (Helios 1.5, Goodman, Japan) was positioned inside the stent using a conventional 0.014 inch guidewire (Balance Middle Weight, Guidant, Indianapolis, IN, USA). The OTW balloon was used to temporarily re-occlude the stented segment and to perform the study-specific, selective intracoronary infusion. Before any study drug infusion, an occlusion test was performed with contrast injection through the guiding catheter to confirm that complete occlusion could be achieved. A conventional 0.014-inch guidewire (Balance Middle Weight, Guidant, Indianapolis, IN, USA) was inserted outside the OTW balloon, distal to the stent (in the “region of interest”) to allow for continuous “online” intracoronary ECG monitoring (Figure 3).
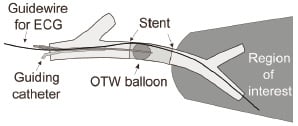
Figure 3. A short over-the-wire balloon was positioned inside the stented segment using a long conventional 0.014 inch guidewire (Balance Middle Weight, Guidant, Indianapolis, IN, USA). ECG signs of myocardial ischaemia were assessed by an intracoronary lead positioned in the guidewire shaft of the over-the-wire balloon catheter and placed distal to the stent in the region of interest. OTW: over-the-wire.
Printouts of these ECG recordings were collected and sent to the independent ECG core laboratory (Cardialysis, Rotterdam, The Netherlands).
Study occlusion and fluid infusion: All subjects underwent two intra-stent balloon occlusions (balloon inflation pressure=0.5 atm). During one occlusion, a continuous intracoronary infusion of pre-oxygenated HBOC-201, warmed to 37°C, was administered through the OTW lumen at a rate of 48 ml/min (maximum volume infused is 144 ml). HBOC-201 was warmed via an in-line clinical fluid warmer (Astotherm®plus, Model AP220S, Futuremed America, Inc., Granada Hills, CA, USA) positioned immediately proximal to the intracoronary OTW helios balloon catheter. HBOC-201 was contained within the sterile, high-pressure infusion line wrapped around the heating coil of the clinical fluid warmer. The infusion rate of 48 ml per minute was selected, based on the efficacy of intracoronary oxygenated HBOC-201 in swine subjected to simultaneous coronary occlusion. The infusion rate employed in this preclinical study was extrapolated to a corresponding rate in man after adjustment for differences in the average body weights of the animals and subjects of the COR-0002 trial.
The control occlusion period was performed similarly, but without infusion (termed “dry occlusion”). Subjects were assigned to receive pre-oxygenated HBOC-201 during the first occlusion period and no-infusion during the second period or vice versa. Each occlusion and infusion period lasted for up to three minutes. Three patients received oxygenated HBOC-201 during the first coronary occlusion and two patients received a dry occlusion as the first experimental intervention. Pre-determined criteria for premature interruption of the balloon occlusions were:
– > 100% increase of left ventricular end-diastolic pressure (LVEDP) from baseline
– Sustained ventricular arrhythmias (ventricular tachycardia or ventricular fibrillation)
– Intolerable chest pain (angina)
– Significant hypertension (systemic blood pressure rise to > 180 mmHg)
– Significant LV dysfunction (EF decrease to less than 35%)
Once the balloon had been deflated and the infusion stopped, a “resting period” of 20 minutes followed for all recorded parameters to return to baseline (in particular LVEDP). The treatment period concluded after the second deflation, once all parameters had returned to their baseline values. A control angiogram was performed immediately after each balloon deflation to allow off-line quantitative coronary angiography (QCA)11 of the region of interest.
Left ventricular haemodynamics
Left ventricular haemodynamic data were recorded before, during and after the procedure by online left ventricular pressure-volume signals obtained by a 7 Fr combined pressure-conductance catheter (CD Leycom, Zoetermeer, The Netherlands) introduced into the left ventricle via the femoral artery. The catheter was connected to a Cardiac Function Lab (CFL-512, CD Leycom, Zoetermeer, The Netherlands) for display and acquisition of pressure-volume loops. Parallel conductance and cardiac output were determined by multiple injections of hypertonic saline solution and thermodilution, respectively, in order to calibrate the volume signals of the conductance catheter. Data analysis was performed off-line by custom-made software. Cardiac function was quantified by cardiac output and stroke volume, stroke work, end-diastolic and end-systolic volume, LV ejection fraction, end systolic and end diastolic pressure, maximal and minimal rate of LV pressure change (dP/dtMAX and dP/dtMIN). The isovolumic relaxation period (defined as the period between the time point of dP/dtMIN and the time point where dP/dT reached 10% of the dP/dtMAX value) was analysed using phase-plot analysis and the time constant of relaxation (Tau) was then determined. The end diastolic pressure-volume relationship (EDPVR) was estimated using the method adopted by Klotz et al12. The change in diastolic distensibility was calculated by the relative left and rightward shifts of the EDPVR at the fixed pressure level of 30 mmHg (V30). Systemic haemodynamics were quantified by systolic, diastolic and mean systemic arterial pressure recorded every three minutes through the guiding catheter for the duration of the study period to investigate any possible hypertensive effects of HBOC-201 infusion.
Objectives
The main objectives of this study (Table 2) were early signs of myocardial ischaemia during intrastent balloon inflation defined as changes in left ventricular relaxation (Tau and dP/dTMIN) and changes in the sum of ST segment deviations (assessed by continuous 12-lead Holter ECG monitoring) compared to baseline.
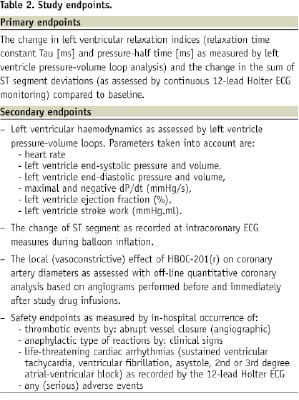
Secondary objectives included changes in the cardiac performance measured by LV pressure volume loop analysis, clinical signs of myocardial ischemia and changes in coronary vascular tone measured by QCA.
Because of the crossover study design, it is not possible to make a direct comparison between treatment modalities (HBOC-201 vs. dry occlusion). However, it was possible to assess treatment safety from the haemodynamic responses, intracoronary and Holter 12-lead ECG monitoring and QCA measurements during the treatment period. Holter 12-lead ECG monitoring continued for four hours after conclusion of the study period and a 12-lead ECG was recorded at discharge or four days post treatment, whichever was earlier. Blood chemistry (LDH, ALT, AST, amylase, CK, CK-MB, troponin T) was collected 6-8 hours post-treatment for comparison to pre-index PCI baseline values. Additional safety endpoints included the in-hospital occurrence of adverse events.
Statistical analysis
Variables with normal distribution were analysed using parametric tests while variables with a non-normal distribution were analysed with non-parametric tests. Continuous variables are expressed as mean±SD or median ± inter-quartile range (IQR) and differences were compared using Student t test or Mann Whitney test. Categorical variables are expressed as counts and percentages.
All values were normalised in order to account for baseline variability. Normalisation was done by dividing each response to treatment (HBOC-infusion or dry occlusion) by the respective baseline. This method of normalisation was selected because it was an appropriate strategy to minimise the variability associated with differences in baselines between subjects. Differences were assessed by T- test or chi-square test. All statistical tests were two-tailed. All analyses were performed using SPSS version 12 statistical software (SPSS Inc., Chicago, IL, USA). A P value <0.05 was considered significant. Due to the descriptive nature of this study, no sample estimation was utilised.
Results
Subject baseline characteristics are described in Table 3.
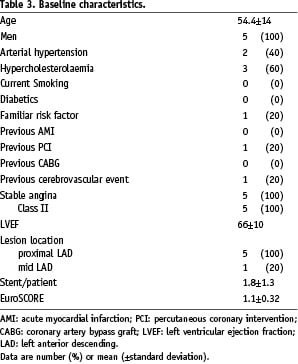
Patients (n=5) of mean age of 54.4±14 years underwent stent implantation for proximal (n=5) and/or mid LAD lesion (n=1) and were enrolled in the present study. Stent per patient ratio was 1.8±1.3. Diagnosis at admission was class II stable angina for all five patients. Hypertension was present in two patients, hypercholesterolaemia in three and familiar risk factor in one patient. No patient was diabetic. The mean ejection fraction (EF) was 66±10% and the mean EuroSCORE was 1.1±0.32%. Procedural and haemodynamic results are illustrated in Figures 4, 5 and 6.
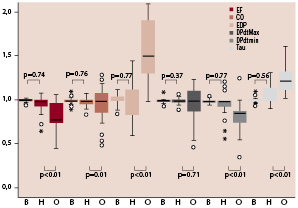
Figure 4. Box plot illustrating the changes in haemodynamics that occurred during HBOC infusion (H) and dry occlusion (O) compared to baseline values (B). Solid lines inside the boxes: median; box ends: IQR. Stars and circles: outsiders.
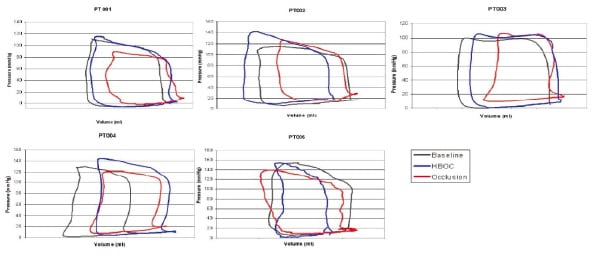
Figure 5. Pressure-volume loops derived from the five patients at baseline, during HBOC-201 infusion and dry occlusion. An important rightward shift of the PV loop occurred in all patients except PT005 during dry occlusion. By contrast, HBOC-201 infusion increased ESV and EDV in only one patient (PT004).
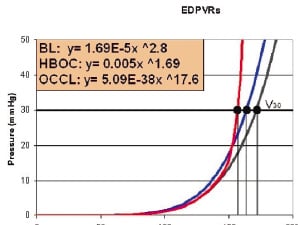
Figure 6. Mean EDPVR and V30 at baseline, during HBOC-201 infusion and dry occlusion.
None of the measured haemodynamic parameters differed significantly from their respective baseline values during HBOC infusion. When data obtained during HBOC infusion and dry occlusion phases were compared, a statistical difference was shown for all systolic and diastolic performance indexes evaluated except dP/dTMAX. EF, CO and dP/dTMIN decreased significantly during dry occlusions from median values of 0.98 (IQR 0.09), 1 (0.06) and 0.99 (0.08) to 0.78 (0.22), 0.9 (0.16) and 0.85 (0.16), respectively. EDP and Tau increased significantly during dry occlusions from median values of 1 (0.39) and 1 (0.16) to 1.5 (0.71) and 1.21 (0.23), respectively. The change in dP/dTMAX was not statistically significant (from 1 (0.04) to 1 (0.28), p=0.71). During dry occlusion, an important rightward shift of the PV loop occurred in all patients but PT005, while during HBOC infusion, ESV and EDV did not increase with the exception of PT004. V30 decreased from 172 ml at baseline to 164 ml and 156 ml during HBOC infusion and dry occlusion, respectively (p=0.21).
Intrastent occlusions performed with infusion of pre-oxygenated HBOC-210 all lasted the intended three minutes duration; specifically, criteria for premature interruption of the inflation were never met. However, mean duration for dry occlusions was 2.13 ± 0.12 min and premature termination of the occlusion was necessary in all subjects. Table 4 identifies the reason(s) for terminating the dry occlusion in each patient.
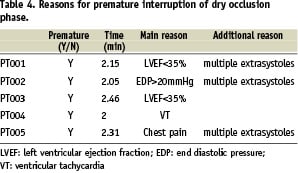
Intracoronary ECG data were available in four out of five patients. Data from patient two (PT002) were considered not analysable by the independent core laboratory. ST segment changes are shown in Figure 7.
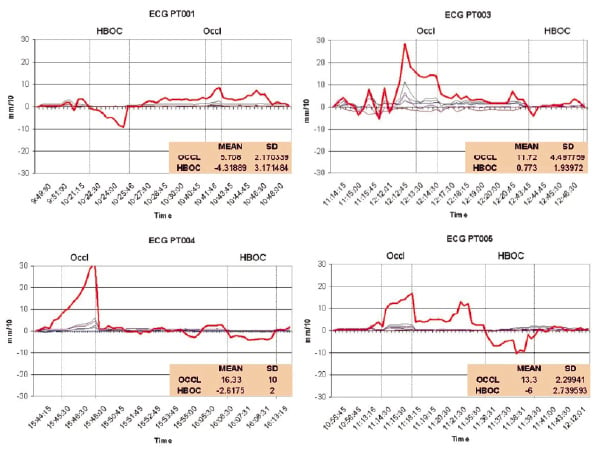
Figure 7. Intracoronary (red line) and surface (grey lines) lead changes in ST segments during the dry occlusion and HBOC-201 infusion interventions. During HBOC infusion, ST segment showed no significant changes from baseline while it was found to be significantly elevated during the dry occlusion phase in patients three, four and five.
During HBOC infusion, ST segment showed no significant changes from baseline while it was found to be significantly elevated during the dry occlusion phase in patients three, four and five. Of note, transthoracic ECG did not show any significant change both during the study phase and during the occlusion period.
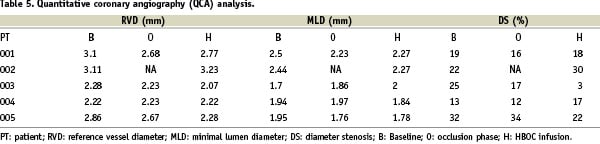
QCA of the arterial segment distal to the stent (Table 5) did not show major differences in reference vessel diameter (RVD), minimal lumen diameter (MLD) and diameter stenosis (DS) during infusion of HBOC compared to baseline values.
From a safety point of view, mean systolic blood pressure (SBP) increase during the HBOC infusion was 10.8±10.5 mmHg. SBP never reached the critical values defined prospectively for protocol-specified pharmacological intervention with nitrates and/or nifedipine.
There were no noteworthy findings in the clinical chemistry parameters and no serious adverse events in any patient through the 4-day follow-up phase occurred.
Discussion
The main results of this study are: 1) Intracoronary infusion of oxygenated HBOC-201 maintained left ventricular haemodynamic status during total proximal LAD occlusion; 2) LV systolic and diastolic properties were not affected during HBOC-201 infusion while they significantly deteriorated during the dry occlusion; 3) intracoronary ECG showed no significant ST segment changes during HBOC infusion; 4) QCA indicated no conduit coronary vasoconstriction by the study drug; 5) HBOC-201 did not cause any adverse event or significantly alter blood chemistry parameters through the follow-up period.
The COR-0002 study was designed to test the hypothesis that pre-oxygenated HBOC-201 is capable of supporting myocardial metabolism and preserving function during total coronary occlusion in humans. The experimental design selected is a sequential intrastent angioplasty balloon inflation model with intracoronary infusion of pre-oxygenated HBOC-201 compared to the same occlusion with no infusion. Parameters of systolic and diastolic function and ST segment changes were measured to determine whether intracoronary delivery of oxygenated HBOC-201 to myocardium at risk mitigates ischaemia. Local delivery of oxygenated autologous blood to the myocardium at risk through the central lumen of a dilated balloon catheter has previously proven to be safe, feasible and effective in patients in the setting of routine coronary angioplasty13. A one minute coronary occlusion and simultaneous infusion of blood at 60 ml/min reduced, but did not eliminate, arrhythmias and angina associated with control occlusions performed in the absence of infusion. Higher infusion rates tested only in vitro resulted in concerning levels of haemolysis and potassium release, events that are obviated with infusion of HBOC-201. As in this prior study, we selected a comparable, low-risk CAD patient population scheduled for elective PCI to assess the impact of intracoronary pre-oxygenated HBOC-201.
Percutaneous coronary angioplasty provides a unique opportunity to study the response of the human myocardium to brief periods of controlled ischaemia and reperfusion and the potential impact of study drugs. The present study involved repeated intracoronary balloon inflations with an intervening period of normal perfusion following successful deployment of a stent in an isolated proximal LAD stenosis. Acute recruitment of collateral vessels and ischaemic preconditioning may be a major confounding factor during successive balloon inflations in PTCA studies5,14-16. Previous studies have shown that if the duration of the first balloon inflation is longer than a “threshold” of ~ 60 to 90 seconds, indicators of myocardial ischaemia including chest pain severity, abnormalities of left ventricular regional wall motion and ST-segment elevation are attenuated during subsequent balloon inflations. These observations provide evidence of myocardial adaptation induced by the first period of ischaemia17-19. We anticipated this potential interference by using an alternating crossover clinical trial design. Furthermore, patients with angiographically evident collateral vessels supplying the area of interest were excluded20.
The evaluation of early signs of myocardial ischaemia in this trial relied on continuous, invasive recording of PV loops, a technique able to provide detailed, reliable data on ventricular and myocardial performance21 throughout the entire cardiac cycle. isovolumic relaxation was evaluated by the peak rate of pressure decline (dP/dTMIN) and by the ventricular relaxation time constant Tau (τ). During the dry occlusion phase, early after balloon inflation, dP/dTMIN significantly decreased while τ significantly increased, both early indicators of myocardial ischaemia. During HBOC infusion, neither dP/dT nor Tau changed significantly from baseline values, suggesting HBOC substantially mollified the ischaemia otherwise induced by balloon inflation. Alterations of the isovolumic relaxation phase are the earliest and most sensitive signs of ischaemia-induced left ventricular dysfunction. Early asynchronous segment re-extension and regional non-uniformity also contribute to early onset and slower rate of ventricular pressure fall and might contribute to these diastolic disturbances22. Passive ventricular characteristics are well described by the end-diastolic pressure-volume relationship (EDPVR). Myocardial ischaemia often results in elevated left ventricular end diastolic pressures and in changes of the slope and position of the entire EDPVR23-25. Such shifts, when they occur, reflect a volume-independent increase in chamber stiffness.
In this series of subjects, LVEDP did not significantly increase during HBOC infusion, but increased continually in all subjects during the dry occlusion. Consistent with these results, V30 decreased more evidently during dry occlusion than during HBOC infusion, indicating greater myocardial stiffness during dry occlusion. It is interesting to note that the slope of the EDPVR remained unchanged during coronary occlusion with HBOC infusion compared to the dry occlusion phase, suggesting worsening of diastolic properties predominantly due to a reduction of myocardial distensibility. The pathophysiological mechanisms of this shift are not completely understood but it is thought to be due to an increased level of intracellular Ca++ during diastole26 and to impaired myosin-actin cross-bridge inactivation secondary to elevated ADP concentrations27-29. Ventricular interactions and pericardial constraints may also contribute to these shifts.
Akin to diastolic function, systolic functions are importantly influenced by ischaemia. HBOC largely averted systolic dysfunction. Ejection fraction (EF) and stroke volume (SV), major indexes of the ejection phase properties, did not show significant variations from baseline during coronary occlusions with HBOC infusion while they were significantly reduced during the dry occlusion phase. These results were achievable despite the fact that the occlusions were performed in the proximal part of the LAD coronary artery which supplies a large “area at risk.” Consistent with these results, dP/dTMAX, commonly used as an isovolumic phase index of cardiac contractility, did not vary significantly from baseline during HBOC infusion suggesting preservation of systolic myocardial performance. It is also noteworthy, however, that the dP/dTMAX values did not differ from baseline even after the onset of ischaemic conditions during dry occlusions, notwithstanding a wide IQR and outliers. It is likely that the shortness of the ischaemic period (criteria for premature interruption of the ischemic period were met in all subjects) and the load-dependence of dP/dTMAX mitigated the real effect of ischaemia on the myocardium.
Early electrical signs of ischaemia in the area of interest were detected by using intracoronary ECG, a technique able to detect early signs of ischaemia with high sensitivity30. In this series of patients, HBOC infusion did not cause any significant alteration of the ST segment. The non-significant changes that occurred during the infusion phase, moreover, were only negative alterations (ST depression), suggesting that the myocardial wall was efficiently and protected by the drug. On the contrary, a significant ST elevation, a sign of transmural ischaemia, was detected in three out of four patients during dry occlusion phase. In PT001, the ST elevation did not reach significant levels most likely because the occlusion was interrupted relatively early, due to severe EF impairment (EF<35%) and the presence of multiple extra-systolic beats. In all patients, ST tended to remain elevated even after the balloon deflation while no ST alterations occurred during the resting periods following HBOC infusion.
In the COR-0001 clinical trial9 the major side effect of the study drug was an increase of systemic vascular resistance, a mechanism not completely understood but possibly related to putative NO scavenging by HBOCs. Importantly, however, intravenously administered HBOC-201 had no effect on conduit or microvascular coronary tone in COR-0001 subjects. In the present study, QCA analysis demonstrated that the intracoronary infusion of HBOC also failed to alter conduit coronary artery tone, as indicated by a lack of effect on RVD, MLD and DS. The absence of coronary vasoconstriction, despite exposure to undiluted HBOC-201, further supports the potential utility of HBOC-201 in complicated patient subsets such as those with coronary artery disease.
Limitations
The present pilot study reports the results from a small series of five patients. Therefore, caution must be exercised in the interpretation of these data.
Although oxygenated HBOC-201 substantially preserved LV function, ameliorated or prevented cardiac arrhythmia and sharply reduced or eliminated coronary angina, treatment with study drug in this clinical trial was not fully optimised. In swine studies, intracoronary infusion of oxygenated HBOC-201 at 30 ml/min preserved approximately 80% of LV regional wall motion during coronary artery occlusion (unpublished data). Lower infusion rates yield proportionately less protection against coronary occlusion and higher infusion rates achieved full preservation of regional wall motion in swine. Extrapolating the 30 ml/min infusion rate in pigs to the average patient weight in the current clinical trial yields an infusion rate of 48 ml/min, the rate administered to subjects in this trial. Hence, higher intracoronary infusion rates based on individual body weights or coronary flows may have provided even greater LV protection against interruptions in coronary blood flow.
In summary, intracoronary oxygenated HBOC-201 represents a new category of pharmacologic strategies that may have utility in patients undergoing PCI. The results of this exploratory trial provide preliminary evidence that HBOC-201 can effectively preserve myocardial mechanical and electrical properties in the face of total coronary occlusion. This represents an important next step in the clinical development program for this product as a treatment for acute myocardial ischaemic syndromes. Future studies will be required
to determine if intracoronary and/or intravenous oxygenated HBOC-201 can enhance treatment efficacy in more complicated patient populations including STEMI and in cases where lesion access is difficult or when microvascular pathology contributes to low TIMI flow.

