Abstract
Aims: There is conflicting data regarding the prevalence and characteristics of coronary artery anomalies (CAAs). We sought to explore the prevalence and characteristics of major and minor CAAs using computed tomography coronary angiography (CCTA).
Methods and results: We prospectively studied 577 patients in sinus rhythm referred for control of stents or for screening due to the presence of multiple risk factors (53%), or due to chest pain, equivalent symptoms or inconclusive stress tests (47%). 40 and 64 slice CT scanners were used. The mean age was 61±11 years and 81% were male. We identified CAAs in 121 (21.0%) patients. Anomalous origination of a coronary artery from the opposite sinus (ACAOS) were identified in 6/577 (1%) patients. Coronary ectasia or aneurysm was present in 10/577 (1.7%) patients. One-hundred and nine intramuscular segments (MB) were found in 100/577 (17.3%) patients. Coronary hypoplasia was identified in 3/577 (0.5%) patients, all involving the RCA, and 3/577 (0.5%) patients had an absent left main coronary artery. None of the segments with ACAOS (proximal segment) or MB had atherosclerotic plaque.
Conclusions: CAAs were highly prevalent along the coronary tree and anatomical characteristics that might help stratify the risk and guide therapy of CAAs could be easily identified with CCTA.
Introduction
During the past few years, several studies have explored the prevalence and characteristics of coronary artery anomalies (CAAs) by means of multiple diagnostic methods. Originally, CAAs have been reported in pathological studies, with its inherent limitations since its population is obviously biased1,2. Subsequently, echocardiographic and conventional selective angiographic studies have reported the prevalence of CAAs non-invasively and invasively, respectively, in in vivo settings3,4. Echocardiographic investigation though, is limited for this purpose since it can only identify the anomalous origin of a coronary artery from the opposite sinus of Valsalva (ACAOS), without being able to describe the course of the coronary arteries or the territory involved, as well as other more frequent types of CAAs5. Moreover, echocardiography, even in children with a good acoustic window, can fail to detect some cases of ACAOS3. In an echocardiographic study of patients with inter-arterial ACAOS and surgical repair, ostial stenosis was not identified by either echo or preoperative catheterisation in five out of eight patients6.
Conventional angiography, in addition to its invasive nature, is restricted for the detection of CAAs for numerous reasons. Angiography lacks the ability to differentiate between high (i.e. inter-arterial) and low (i.e. retro-aortic) risk ACAOS, as well as the myocardial territory involved. Besides, myocardial bridging (MB) is largely under-reported by conventional angiography7, probably owed to the ability of the technique to identify only MB that produce the typical “milking” phenomenon.
Several additional CAAs with different and heterogeneous presentations can be found, including coronary artery ectasia or aneurysms (CEA), which may induce myocardial ischaemia even without concomitant atherosclerotic disease8. The global prevalence of major and minor CAAs remains a matter of debate since populations between studies are widely different. In addition, methodological aspects and limitations natural to most techniques further influence the results. Although it has been advocated that major and minor CAAs should be reported as a whole9, few studies have reported the global incidence of these findings.
The purpose of the present study was therefore to explore the prevalence and characteristics of CAA using high resolution computed tomography coronary angiography (CCTA) in a consecutive series of 599 patients.
Methods
Between October 2005 and December 2007, consecutive patients in sinus rhythm, who were able to hold breath for ≥ 15 seconds, without history of contrast related allergy, renal failure, arrhythmia, or haemodynamic instability, and who were referred for evaluation by computed tomography coronary angiography (CCTA) in our institution, were prospectively studied for the presence of CAAs. Patients with a heart rate >70 bpm received beta-blockers either as a single oral dose (atenolol 50 mg) one hour before the scan, or intravenously (propranolol 1 mg/min) immediately before the scan.
CCTA acquisition and analysis
Scans were performed using 40-channel (324 patients) and 64-channel (253 patients) multidetector CT scanners (Brilliance 40 and Brilliance 64, Philips Healthcare, Cleveland, OH, USA). A bolus of 80-125 ml of iodinated contrast material (Optiray®, Ioversol 350 mg/ml, Mallinckrodt, St. Louis, MO, USA) was injected through an arm vein at 5-6 ml/s. The scan parameters were a collimation either 40∞0.625 mm or 64∞0.625 mm, rotation time 0.4 seconds, tube voltage 120 kV, and mAs 600-1000. A bolus tracking technique was used to synchronise the arrival of contrast at the level of the coronary arteries with the start of acquisition.
Reconstructions were assessed using axial planes, multiplanar reconstructions, volume rendering techniques, curved multiplanar reconstructions, and maximum intensity projections. In all patients, images were reconstructed in end diastole (75% of the R-R interval) and image quality was evaluated on a per segment basis. Where images were judged to be suboptimal, additional reconstruction windows (30%, 40%, 70% and 80%) were explored in order to achieve optimal quality images. All analyses were performed on a dedicated workstation (Brilliance Workspace, Philips Healthcare, Cleveland, OH, USA). Two experienced observers (GARG and MAR) evaluated all scans.
Definition of CAA
The classification scheme of Angelini et al was used in order to identify and categorise CAAs10. ACAOS were identified and the type, path, and the presence of ostial stenosis and atherosclerosis were reported as previously described10. Myocardial bridging (MB) was identified as an intramuscular segment of a coronary artery. As previously reported, segments covered by a thin layer of muscle were included since they may be compressed during systole11. The location (mid-left anterior descending [LAD], distal LAD, diagonal, obtuse marginal, intermediate branch), path (deep septal, superficial, right ventricle), length, and the presence of atherosclerosis within the host vessel and intramural segment were evaluated.
Coronary ectasia or aneurysms (CEA) were defined as non-obstructive lesions of the epicardial coronary arteries with a dilation exceeding the 1.5- to 2.0-fold of normal diameters, and a coronary aneurysm was defined as a dilation ≥ 2.0-fold of normal diameters12. CEA were classified as saccular when the transverse diameter was greater than the length, and fusiform when the longitudinal dilation was larger than the transverse diameter. Dilated coronaropathy was defined as bilateral fusiform CEA involving both the right and left coronary arteries8.
Statistical analysis
Discrete variables are presented as counts and percentages. Continuous variables are presented as mean ± SD. Comparisons among groups were performed using χ2 tests. A two-sided p value of less than 0.05 indicated statistical significance. Statistical analyses were performed with use of SPSS software, version 13.0 (Chicago, Ill, USA).
Results
Five hundred and ninety-nine consecutive patients referred for evaluation by CCTA were prospectively studied for the presence of CAAs. Twenty-two patients (3.7%) were excluded due to poor image quality and one (0.2%) due to contrast extravasation, leading to a final study population of 577 patients. Patients were studied as control of stents or for screening due to the presence of multiple risk factors 307/577 (53%), or due to chest pain, equivalent symptoms or inconclusive stress tests 270/577 (47%). The mean age was 60.8±11.3 years and 466/577 (81%) were male. The mean heart rate immediately before the scan was 61.1±7.4 bpm. The right coronary artery was dominant in 503/577 (87%) of cases, the left circumflex in 45/577 (8%) and there was co-dominance in 29/577 (5%) of cases.
Following the classification proposed by Angelini et al10, CAAs were identified in 121/577 (21.0%) patients (Table 1).
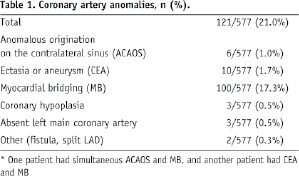
Twenty three percent (107/406) of male patients had CAAs, whereas 12.6% (14/111) of female patients had CAAs (p=0.02).
Six ACAOS (1.0%) were detected, 3 right ACAOS (Figure 1) and 3 left ACAOS (Figure 2).
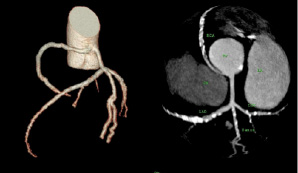
Figure 1. Right coronary artery arising from the left sinus of Valsalva, with a inter-arterial (between the aorta and the pulmonary artery) course, an acute angle take-off, and ostial stenosis without evidence of atherosclerosis at the proximal segment.
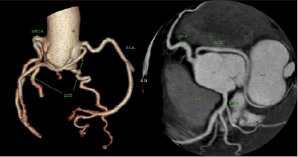
Figure 2. Left circumflex arising from the right sinus of Valsalva, with a retro-aortic course, ostial stenosis, and no evidence of coronary atherosclerosis along the coronary tree. This patient had a previous angiogram deemed as normal, where a prominent diagonal was probably mistaken with the left circumflex.
Clinical and anatomical features of these patients are depicted in Table 2.
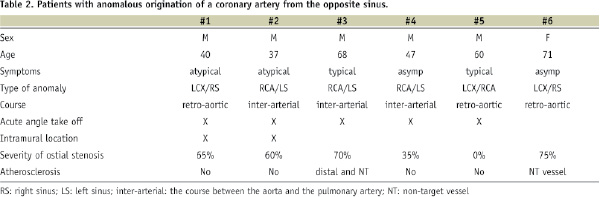
The mean age of patients with ACAOS was 57±13 years. Most patients were male, clinical presentations were diverse, and concomitant atherosclerotic disease was rare. Half of the ACAOS had a retro-aortic course and half an inter-arterial course (between the aorta and the pulmonary trunk). No patients had atherosclerotic disease at the proximal segment. A 40 year-old patient with no cardiovascular risk factors, atypical chest pain and positive thallium scan, who underwent a conventional angiogram in another centre that was reported as normal, had the left circumflex ostium at the right sinus of Valsalva, with a retro-aortic course and ostial stenosis without evidence of atherosclerosis. During the angiogram, a prominent diagonal had been taken as a normal LCX, since the latter had its ostium 1.5 mm caudal from ostium of the RCA (Figure 2) and was therefore never engaged during the angiogram.
Coronary ectasia or aneurysm (CEA) was identified in 10/577 (1.7%) patients. Characteristics of patients with CEA are shown in Table 3.
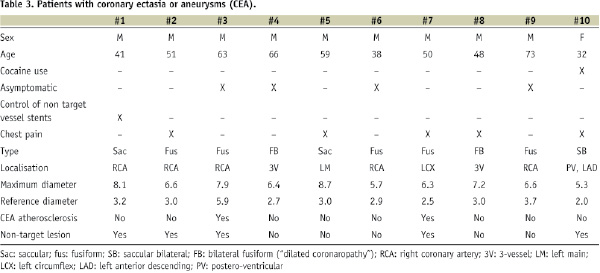
Ninety percent were male. In 2 patients, CEA was saccular, in 5 patients was fusiform, in one patient was saccular bilateral, and in other 2 was fusiform bilateral (“dilated coronaropathy”) (Figure 3).
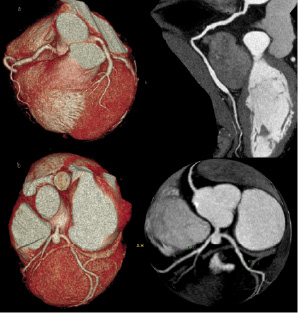
Figure 3. Coronary ectasia or aneurysms: a) Bilateral fusiform coronary ectasia (“dilated coronaropathy”). On the right panel, a curved multiplanar reconstruction shows diffuse ectasia of the distal right coronary artery. b) Saccular aneurysm of the distal left main coronary artery with ostial stenosis of the left anterior descending.
One patient had a history of cocaine use and bilateral aneurysms. Another patient was admitted to our hospital for surgical intervention of a retroperitoneal tumour and suffered a hypertensive crisis with signs of acute heart failure during surgery. A saccular aneurysm of 8.5 mm∞8.0 mm in the distal left main trunk affecting the ostium of the LAD, with no evidence of coronary atherosclerosis was detected by CCTA (Figure 3 b). Another patient suffered an acute myocardial infarction due to occlusion of a fusiform coronary artery aneurysm in the proximal LCX.
One hundred and nine intramuscular segments were identified in 100 (17.3%) patients. Characteristics of the MB are displayed on Table 4.
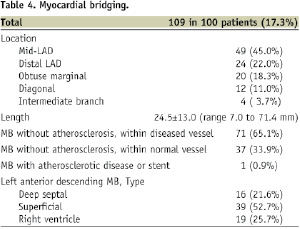
MB was found in 88/466 (18.9%) of male patients and in 12/111 (10.8%) of female patients (p=0.04). Most intramuscular segments were located in the LAD (67.0%), whereas no MB was located at the right coronary artery. Although 71 (65.1%) patients had atherosclerotic disease in the “host” vessel, there was no evidence of atherosclerosis within any intramuscular segment. Nevertheless, one patient had a previous stent in such segment due to ischaemia. Figures 4 shows examples of MB.
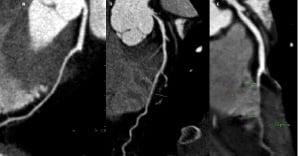
Figure 4. Myocardial bridging: a) deep septal type, b) superficial type, c) right ventricular type. On panel b, a severe, non-calcified lesion, can be seen on the left main coronary artery.
Coronary hypoplasia was identified in 3 patients, all involving the RCA, with a large, dominant LCX (Figure 5).
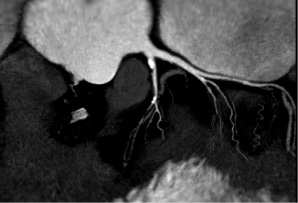
Figure 5. Coronary hypoplasia of the right coronary artery. A very large left circumflex is dominant. Note a severe lesion at the distal left anterior descending coronary artery.
Three patients had an absent left main coronary artery (separate origin of the LAD and the LCX, Figure 6).

Figure 6. Absence of left main coronary artery. The left anterior descending and the the left circumflex clearly arise from independent ostiums at the left sinus of Valsalva.
Discussion
Although the medical community has been aware of the presence of CAAs for a long time1,2, the random nature of the reports, the lack of prospective natural history studies, and the conflicting data regarding the prevalence of CAAs, have created confusion about the true prevalence as well as the clinical and haemodynamic implications of CAAs. More recently, the ischaemic mechanisms of CAAs have been explored with more detail on angiographic and post-mortem patients10. With the advent of novel technologies such as magnetic resonance coronary angiography and CCTA, non-invasive detection of all CAAs can be accomplished with high precision. CCTA is an emerging technology that has a high sensitivity and specificity for the detection of significant epicardial coronary atherosclerosis, as well as an effective method to evaluate the extent and distribution of non-significant lesions in the coronary tree13-15. Importantly, CCTA provides superior anatomical information and can accurately visualise the sinus of Valsalva, the distal coronary tree, and the myocardium itself16. Although a previous study has reported the prevalence and anatomical features of MB by means of CCTA11, the present study reports for the first time the prevalence and characteristics of all (major and minor) CAAs in consecutive series of 599 adults using CCTA. Identification of CAAs was feasible and straightforward using CCTA. We found a high prevalence of CAAs (21%), being MB the most frequent finding as expected.
Anomalous origination of a coronary artery from the opposite sinus (ACAOS)
With a prevalence ranging from 0.2 to 1.0%17, the anomalous origination of a coronary artery from the opposite sinus of Valsalva (ACAOS), represent a common cause of sudden cardiac death in the young population, particularly in individuals that undergo strenuous exercise18. Unfortunately, since most patients with ACAOS are asymptomatic (less than one third of patients develop chest pain, syncope, palpitations, dyspnea), diagnosis is usually made post-mortem19-21. In our series, similar to previous reports10, the prevalence of ACAOS was 1%, and 5 out of 6 patients were male. Of note, one patient had previously undergone a coronary angiography which was erroneously deemed as normal. Most segments with ACAOS displayed ostial stenosis. Nevertheless, none of the proximal segments of ACAOS had atherosclerosis. As proposed by Angelini et al9, such discordance might be explained by the coronary hypoplasia commonly seen in proximal segments of ACAOS. This has implications regarding eventual interventions in the host vessel, since percutaneous intervention of non-atherosclerotic stenosis could potentially be hazardous and not effective.
CCTA evaluation allowed the identification of the ostium of the anomalous coronary arteries, the presence of atherosclerosis, intramural segments, ostial stenosis and/or acute angle take-off. In addition, we were able to differentiate between high (i.e. inter-arterial) and low (i.e. retro-aortic) risk ACAOS.
The choice of therapy (medical, stent implantation or surgical repair) depends on the ACAOS type (right or left), symptoms, presence of ostial stenosis, course, myocardial territory involved, and the presence of reversible ischaemia9. Accordingly, since CCTA can provide valuable information regarding the type, origin, stenosis, course and territory involved of ACAOS, this technique might be a useful tool to guide therapy in such patients.
Myocardial bridging (MB)
MB have been recognised as minor CAAs10. Pathological and clinical studies are largely discordant regarding the prevalence of MB, ranging from 15% to 85% in post-mortem series22-24 and from 0.5% to 2.5% in angiographic series7,25,26. Despite in most cases MB are incidental findings during coronary angiography, several authors have reported an association between MB and ischaemic events, including myocardial infarction and sudden death27.
In our study, MB was predominantly found in males, and the mid-LAD was the site of preference (45%), although location at secondary branches was not uncommon. In line with previous reports, the right coronary artery was protected from MB11,27. Of note, deep septal MB were the least common type. This might partially explain the underestimation of MB by conventional angiography, since the prevalence of MB in our series, if we would have taken into account only deep septal MB, would have been of 2.7%, similar to the prevalence reported in angiographic studies7,25,26. Experimental studies have shown that the length of a coronary narrowing has an impact on the haemodynamics28. In our study, the mean length of the intramuscular segments was 24.5 mm. Awareness of the type, length, depth, and location of intramuscular segments has implications for eventual bypass surgery, enabling the guidance for a more accurate and safe location of the distal anastomosis.
It is noteworthy that out of 109 intramuscular segments, none of them had atherosclerotic disease within the tunnelled segment. Recently, a number of studies demonstrated that the average and maximal peak velocity measured by intracoronary Doppler within the tunnelled segment was more than twice as high as the velocity at the proximal and distal segments27. Accordingly, the lack of atherosclerosis might be potentially attributed to the high shear stress and, hence, laminar flow present within the tunnelled segments. Conversely, atherosclerosis has a tendency to arise more frequently in low-oscillatory shear stress regions, where there is a loss of the physiological flow-oriented alignment of the endothelial cells29-31.
Coronary ectasia or aneurysms (CEA)
Even in angiographically normal coronary arteries, patients with CEA can develop myocardial ischaemia and/or myocardial infarction. This has been shown by Kruger et al, who demonstrated exercise-induced ischaemia and inappropriate vasoconstriction in patients with non-atherosclerotic dilated coronaropathy, thus enforcing the concept of endothelial dysfunction associated with CEA8. The angiographic incidence of CEA in diagnostic cardiac catheterisations has been found to vary between 0.3% and 4.9%32-35. CEA are caused by atherosclerosis in 50% of the cases, whereas 30% are usually congenital and only 10% to 20% of CEA are related to inflammatory or connective tissue disorders12,35. In our series, we identified 10 (1.7%) patients with CEA, and only 20% had evidence of atherosclerotic plaque by CCTA, although 50% of the patients had atherosclerosis elsewhere along the coronary tree. In agreement to early reports, CEA were largely (90%) more frequent in males than females2. Of note, the only female with CEA, with bilateral aneurysms, had a history of cocaine use. The association between cocaine use and CEA has been described recently by Satran et al, who found that 30% of cocaine users had coronary artery aneurysms, typically bilateral2.
Clinical implications
To our knowledge, the present study reports for the first time the prevalence and characteristics of all CAAs in a consecutive series of patients using CCTA. Identification of CAAs by CCTA was feasible and allowed a clear distinction between benign and potentially hazardous CAAs. In addition, anatomical characteristics that might help stratify the risk and guide therapy of CAAs could be easily identified. We found a high prevalence of CAAs along the coronary tree. With the growing use of CCTA for the detection of coronary artery stenosis, and since identification of CCAs does not require any modification from standard scan protocols, the findings of the present study should encourage CCTA specialists to routinely explore for the presence of CAAs. Furthermore, tube current modulation is currently available for use in all cardiac CT scans, and has shown to reduce radiation dose to levels comparable to conventional angiography36. It is noteworthy that none of the segments with ACAOS (n=6) or MB (n=109) had proximal atherosclerosis. As aforementioned, this might potentially be due to the smaller reference diameter at such segments and hence increased shear stress, leading to protection from atherosclerosis. Given the scarcity of data regarding the natural history of CAAs, large multicentre CCTA registries that provide unique prognostic information of CAAs are warranted.
Limitations
The present was an observational study and the findings were not systematically confirmed by conventional angiography. However, CCTA has been validated as an accurate diagnostic tool to evaluate the coronary tree13. Since the study population was mainly constituted by adult patients referred for cardiovascular study, we cannot consider the sample as normal or unselected. Due to the observational nature of the study, we lack cause effect mechanisms to explain the aetiology of coronary ectasia. Similarly, we did not systematically perform functional tests in order to evaluate the haemodynamic significance of the findings. Finally, despite CAAs seem to be more prevalent among males, we cannot completely rule out a possible influence of the under-representation of women in cardiovascular populations. A similar trend was however shown also in paediatric populations3.

