Abstract
Aim: The clinical outcome of patients with severe renal dysfunction undergoing percutaneous coronary intervention (PCI) is poor. However little is known concerning the impact of mild renal insufficiency on long-term clinical outcomes after successful coronary stenting. The present prospective observational study was designed to evaluate long-term clinical outcomes in relation to renal insufficiency after successful coronary stenting.
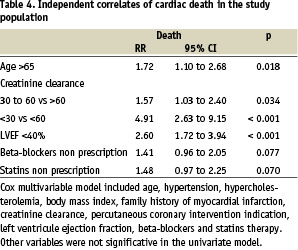
Methods and results: A consecutive series of 1454 patients were enrolled between January 4th 1997 and January 4th 1999 Demographic and clinical characteristics and long term clinical outcome were compared for patients with normal creatinine clearance (>60 ml/mn), mild renal dysfunction (creatinine clearance rates 30-60 ml/mn) and severe renal dysfunction (creatinine clearance rates <30 ml/mn). Patients with moderate or severe renal dysfunction were older and with more severe coronary artery disease. Beyond conventional risk factors like age (RR = 1.72 [1.10-2.68] 95% CI ; p<0.018), or low left ventricular ejection fraction (RR = 2.60 [1.72-3.94] 95% CI ; p<0.001), severe (creatinine clearance rates < 30 ml/min) and mild (creatinine clearance 30-60 ml/min) renal dysfunction were also identified as strong independent predictors of death after successful coronary stenting (RR = 4.91 [2.63-9.15] 95% CI, p<0.001 and RR = 1.57 [1.03-2.40] 95% CI, p<0.034, respectively).
Conclusions: In patients with successful coronary stenting, preprocedural creatinine clearance remains an important independent predictor of long term death. These data reinforce the importance of widespread application of prevention strategies especially in patients with coronary artery disease complicated by renal dysfunction.
Introduction
The negative impact of severe renal dysfunction on long-term outcomes of patients after percutaneous coronary intervention has been recognized these last years1,2. However little is known concerning the relationship between mild renal dysfunction and long-term survival after coronary stenting. The high prevalence of cardiovascular diseases among patients starting dialysis suggests that accelerated atherogenesis begins earlier in the spectrum of chronic renal insufficiency3. Given the greater insight of the importance of even mild renal dysfunction on the occurrence of cardiovascular complications, we have conducted a prospective observational study to evaluate the long-term clinical outcomes in relation to renal insufficiency after successful coronary stenting.
Methods
Patients
This prospective observational study was designed to examine the relationship between the preprocedural creatinine clearance and the risk of major adverse cardiovascular events after successful coronary stenting. A consecutive series of 1454 patients with successful coronary stenting was enrolled after informed consent obtained between January 4th 1997 and January 4th 1999. Follow-up was obtained by mailed questionnaires and scripted telephone interviews performed by a physician. Events were verified by contacting the patients’ primary physician and reviewing medical records and death certificates.
Assessment of renal function
Using the creatinine level obtained before the angiogram renal function was assessed by the estimated creatinine clearance using the Cockroft-Gault formula: creatinine clearance (ml/min) = [([140 - age] X weight [kg])/72 X serum creatinine (mg/dl)] (X 0.85 for women). This equation has a close correlation with measured creatinine clearances (correlation coefficient 0.83) and gives a more accurate assessment of renal function than serum creatinine alone (4). Patients were categorized according to the level of creatinine clearance (< 30 ml/ min (n= 42, of those 4 were on dialysis on a regular basis), 30-60 ml/min (n=395), > 60 ml/min (n=1007).
End-points and definitions
The pre-specified primary end-point of the study was the mortality and secondary end-points included cardiovascular mortality and other major adverse cardiovascular events (myocardial infarction, percutaneous coronary interventions [PCI], and coronary artery bypass graft surgery [CABG]). Except for those of proven non cardiac origin, cardiac death was recorded if death occurred suddently or if death was associated with documented MI or other cardiac causes as congestive heart failure and arythmia.
The severity of coronary stenosis was determined by visual assessment by means of orthogonal view by the operator not awared about the study design. Dual antiplatelet agents using aspirin and either ticlopidin or clopidogrel were systematically used at least one month following coronary stenting.
Statistical analysis
Base-line characteristics of the study population are presented as counts and percents for categorical variables and as mean(SD for continuous variables. Differences in percents were evaluated by the Chi-square test, and means by ANOVA. Validity conditions were checked for each comparisons. An univariate analysis with the Kaplan-Meier product-limit method and the log rank or Breslow tests was used to compare the different groups of patients.
For the identification of independent prognostic factors related to cardiovascular death Cox’s proportional hazards models were used after adjustment for variables proved to be significant with univariate statistical analysis (P<0.20). The relative risks were given with a 95 percent confidence interval (95% CI). All calculations were performed with SPSS Professional Statistics™ 10.0.7 (SPSS Inc., Chicago, Illinois). P values <0.05 were considered significant.
Results
Baseline characteristics of the study population
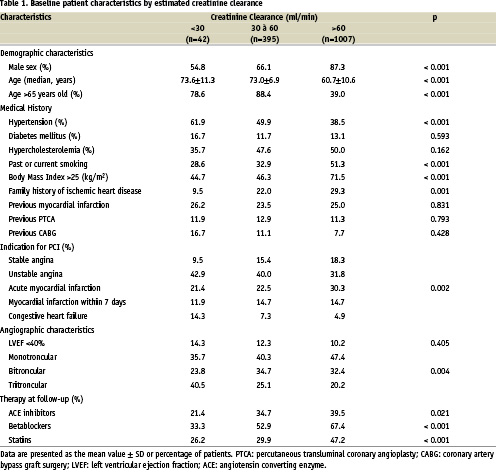
The baseline characteristics of the 1454 patients who underwent successful coronary stenting grouped by estimated creatinine clearance are shown in Table 1. Patients with severe and mild renal dysfunction were more likely to be older (73.6±11.3 and 73.0±6.9 respectively vs 60.7±10.6 in patients with normal creatinine clearance, p<0.001), women (45.2% and 33.9% respectively vs 12.7% in patients with normal creatinine clearance, p<0.001), hypertensive (61.9% and 49.9% respectively vs 38.5% in patients with normal creatinine clearance, p<0.001) and with more severe coronary artery disease (tritroncular lesions found in 40.5% and 25.1% of patients respectively vs 20.2% in patients with normal creatinine clearance, p=0.004). Such patients more commonly had heart failure and the most common indication for PCI was unstable angina. Furthermore patients with the lowest creatinine clearances received less frequently ACE inhibitors (21.4% and 34.7% in patients with severe and mild renal dysfunction respectively vs 39.5% in patients with normal renal function, p=0.021), beta-blockers (33.3% and 52.9% respectively vs 67.4%, p<0.001) and statins (26.2% and 29.9% respectively vs 47.2%, p<0.001).
Long term clinical outcome
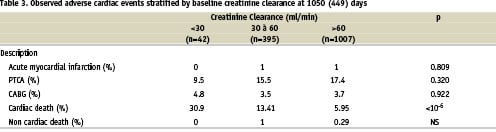
Clinical follow-up information concerning the mortality was obtained for 1444 patients (99.8%). A mean follow-up period of 1050.9±449 days was ensured for the whole study population. Among the 133 (9.21%) deaths observed during the follow-up period, 126 (94.74%) were related to a cardiovascular cause and 7 (5.26%) not related to heart disease. According to the creatinine clearance, the cardiovascular mortality rates were 5.95%, 13.41% and 30.95% for normal renal function, mild renal dysfunction and severe renal dysfunction respectively.
Patients with creatinine clearance <30 ml/min had a high intra-hospital mortality 14.3% within the first 10 days after intervention. After the index procedure, 3 deaths were related ventricular fibrillation, 2 to refractory cardiogenic shock and 1 related to mesenteric infarction.
The pre-specified primary end-point of the study (cardiovascular death) was related to the presence of impaired renal function as shown by the Kaplan-Meier analysis (Table 2 and Figure 1). The frequency of other major adverse cardiovascular events (myocardial infarction, revascularization [PCI or CABG]) at 2.8 years follow-up is shown in Table 3. Patients with severe and moderate renal insufficiency had an increased risk of mortality related to cardiovascular death (30.9% and 13.41% respectively vs 5.95% in patients with normal renal function, p<10-6). Of note, there is no difference regarding the ischemic driven revascularization rates in the different groups of patients.
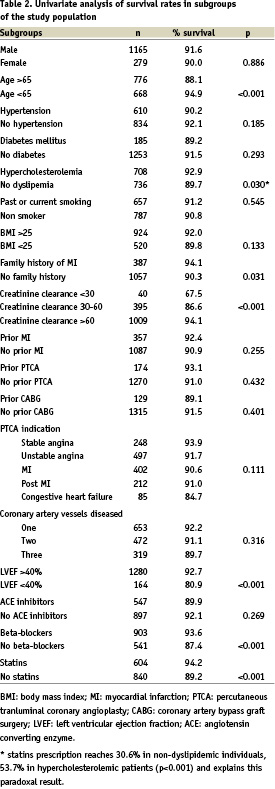
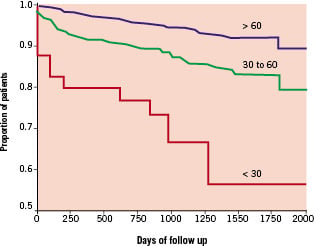
Figure 1. Cardiovascular mortality after successful coronary stenting in the study population based on their estimated creatinine clearance.
The relative risks and 95 percent confidence intervals (95% CI) derived from the Cox regression analysis are given for independent predictors of death in Table 4. Beyond conventional risk factors like age (RR = 1.72 [1.10-2.68] 95% CI ; p<0.018), or low left ventricular ejection fraction (RR = 2.60 [1.72-3.94] 95% CI ; p<0.001), severe (creatinine clearance < 30 ml/min) and mild (creatinine clearance between 30 and 60 ml/min) renal dysfunction were also identified as strong independent predictors of death after successful coronary stenting (RR = 4.91 [2.63-9.15] 95% CI, p<0.001 and RR = 1.57 [1.03-2.40] 95% CI, p<0.034, respectively). These results demonstrate that clearance creatinine was significantly associated with cardiovascular mortality in patients after successful coronary stenting.
Discussion
The main finding of the present study, in a large consecutive series of patients who underwent PCI in the modern era with systematic coronary stenting, is that renal dysfunction significantly increased the risk of cardiac death after successful coronary stenting in a dose dependent manner.
Increased creatinine concentrations are common in older patients and are independently associated with an increased risk of death, cardiovascular disease and congestive heart failure5. Of interest was the finding that the increased risk of death began at low creatinine concentrations. Although stenting in the general population has been extensively studied6,7, there are very little data examining the use of coronary stenting in patients with renal dysfunction1,8, primarily because these patients are usually excluded from clinical trials or have not been considered as specific subgroups. Some data are available providing evidence that even mild renal dysfunction is an independent predictor of increased short and mid-term mortality after PCI9-12. However in these series the patients were not systematically treated by coronary stenting and conventional balloon angioplasty used in 22.8% to 68.5% of patients has been recognized as a negative prognosis factor of ischaemic events especially in patients with renal dysfunction12.
Indeed patients with renal dysfunction have been shown to have high angiographic restenosis rates1,13. In the present study, the lack of association between renal impairement and clinically driven revascularization rates (clinical restenosis) may reflect silent ischaemia associated with angiographic restenosis, resulting in an increased risk of cardiac death in patients with renal dysfunction while maintaining equivalent rates of clinical restenosis. The continued divergence of death after 6 months when restenosis would no longer be expected to occur, argues for an additional effect of renal dysfunction on the progression of coronary artery disease. The cardiovascular system is profoundly affected by renal insufficiency by numerous factors that contribute to the development of ischaemic heart disease, including hyperlipidemia, secondary hyperparathyroidism, high rates of hypercalcemia episodes, hyperphosphatemia and increased platelet aggregability. The effects of renal insufficiency on oxidative stress, homocysteine and fibrinogen levels are also well documented14-17. Although the deleterious effects of renal dysfunction on coronary artery disease are well established, the precise mechanisms of this interaction are not clearly understood. With regard to mild renal insufficiency, little is known about the role of coronary stenting on long term clinical outcome in these patients. Increased silent restenosis after coronary stenting may account in part of the increased mortality rate in this population as previously mentioned9.
Medical management in patients with renal dysfunction has been based on therapy shown to be beneficial in other populations. Currently these medications in patients with documented coronary artery disease include aspirin18, beta-blockers19, statins20 and ACE inhibitors21. However management of coronary artery disease in patients with renal insufficiency is more difficult than in patients with normal renal function22. In our study population all patients were treated by PCI and stent implantation, but patients with severe or mild renal dysfunction were less frequently treated with medications recognized to improve outcomes like beta-blockers, ACE inhibitors and statins. After adjusting for a higher frequency of co-morbidities and for differences in medical management, renal insufficiency remains a strong and independent predictor of increased long-term mortality and is additive to other clinical markers of worse outcome.
Limitations
Creatinine clearance was estimated from preprocedural creatinine measurements and not measured directly. Moreover we have only a single measurement of creatinine which may have changed over time. Other limitations of the present study are inherent to all prospective but non-randomized study registries including the influence on results of referrral and selection bias that may be incompletely corrected despite adjustment for recognized risk factors. However the study has included a large series of consecutive patients and the results are robust and consistent.
Conclusion
In patients with successful coronary stenting, creatinine clearance remains an important independent predictor of long term death. These data reinforce the importance of widespread application of prevention strategies after coronary revascularization especially in patients with coronary artery disease complicated by renal dysfunction.

