Abstract
Aims: An increasing number of patients are referred for percutaneous aortic valve replacement (PAVR). Although case studies are available on outcome of selected patients, little is known about the demographics, treatment assignment and survival of the total referred population.
Methods and results: This was a prospective observational cohort study. From September 2005 to September 2007, 100 patients were referred for PAVR of whom 39 underwent PAVR, 14 surgical valve replacement (AVR) and three balloon valvuloplasty (PABV). Another 16 refused treatment and 28 were no candidate (non severe aortic stenosis [n=11], asymptomatic and normal ventricular function[n=3], comorbidity[n=12], technically PAVR not feasible[n=2].) The logistic EuroSCORE (Mean, sd) was:15±6%(PAVR), 9±11%(AVR), 22±15%(PABV), 25±14%(refusals) and 17±12%(no-candidate). The mean follow-up was 13 months (range 0-30 months). Cumulative survival at six months was 97%, 85% and 70%, for PAVR, AVR and refusals, respectively. At 12 months, it was 87%, 62% and 40% respectively.
Conclusions: Not all patients referred for PAVR finally receive it. Approximately 15% of the patients received AVR and 30% were considered not eligible. This may reflect the lack of sufficient data and need for an improvement in the technology in order to offer PAVR to both lower and higher risk patients. Considering risk and outcome, it is conceivable that patients who refused treatment could have benefited the most from it.
Abbreviations
AVR: Surgical Aortic Valve Replacement
CABG: Coronary Artery Bypass Grafting
CVA/TIA: Cerebrovascular Accident/Transient Ischaemic Attack
NYHA: New York Heart Association
LV: Left Ventricular or Left Ventricle
PABV: Percutaneous Aortic Balloon Valvuloplasty
PAVR: Percutaneous Aortic Valve Replacement
PCI: Percutaneous Coronary Intervention
PVD: Peripheral Vascular Disease
Introduction
Stenosis of the aortic valve is the most common valvular lesion affecting the adult population of which the prevalence increases with age.1-3 If symptomatic, or in case of impaired ventricular function, the prognosis is poor, especially when valve replacement is or is not – or cannot be – performed. In such instances, the annual mortality amounts to 25%.4 To address this problem, percutaneous balloon valvuloplasty (PABV) has been introduced in the mid-eighties but abandoned because of lack of efficacy and risks.5 Recently, percutaneous aortic valve replacement (PAVR) has entered the clinical field.6-8 Although still in an early phase of development and experience, it holds firm promise for a vast number of patients who are not referred to surgery or are denied surgery itself. A number of studies discloses that 30 to 60% of patients with aortic stenosis are not referred for further treatment.1,9-13 PAVR may uncover this hidden population. Although case studies are available on patients who received PAVR, little is known about the demographics of the total population referred for PAVR in addition to treatment assignment and survival of this population.14 We sought to determine this by means of a single centre, prospective observational cohort study.
Methods
At the initiation of PAVR in our institution (September 2005), a dedicated out-patient clinic was set up to which patients with aortic stenosis who were considered poor surgical candidates or ineligible for surgery could be referred. The referring cardiologists were informed about this service during a special seminar in which the developments in both surgical and percutaneous valve replacement were presented by a surgeon and an interventional cardiologist.
Patients
The patients referred to the outpatient cardiology clinic were seen by one senior cardiologist. They underwent a planned clinical examination, ECG, laboratory assessment and an echo Doppler study. If there was an indication for valve replacement (based upon the severity of aortic stenosis in combination with the presence of symptoms and/or reduced ventricular function) coronary angiography and angiography of the peripheral vascular tree was proposed.15,16 The specific patient-by-patient case was then discussed in a dedicated cardiology-cardiothoracic meeting during which the final treatment decision (surgical valve replacement [AVR], PAVR, PABV or medical therapy) was decided based upon the consensus of a multidisciplinary team consisting of a senior interventional cardiologist, cardiothoracic surgeon and general cardiologists. The treatment decision was then carefully noted on a surgical chart. All patients treated by PAVR received the CRS™, CoreValve, (CoreValve, Irvine, CA, USA).7,17 PAVR was offered to patients who were considered poor surgical candidates. This was defined by age > 80 years or initially a logistic EuroScore of > 20 and subsequently by age > 75 or a logistic EuroScore > 15. Irrespective of age and EuroScore, PAVR was proposed in the case of severe comorbidity (e.g. respiratory failure [FEV1 < 1 l], pulmonary hypertension [systolic pressure > 60 mmHg], liver cirrhosis, cachexia [BMI < 18 kg/m2], previous cardiac surgery or thoracic wall deformities, porcelain aortas, etc.).
All baseline data (demographic, clinical, laboratory and technical) were prospectively entered into a devoted database. The preselected variables were: age, gender, body length, body weight, diabetes (treated), chronic obstructive pulmonary disease (treated) history of cerebrovascular accident / transient ischaemic attack, peripheral vascular disease, myocardial infarction, coronary artery bypass grafting and percutaneous coronary intervention.
For the assessment of the severity of aortic stenosis the following variables were collected: peak velocity (continuous wave Doppler) over the aortic valve and aortic valve area.18 In addition, regurgitation of the aortic, mitral and tricuspid valve was determined by colour Doppler and grade into mild (I-II), moderate (III) and severe (IV). Left ventricular function was defined by visual assessment and graded into the following three categories: normal, moderate or poor. On the basis of the information derived from these clinical and technical assessments, the logistic EuroSCORE was calculated using the web based system (http://www.euroscore. org/calc.html).
In order to verify whether the patients referred for PAVR differed from the patients who were directly referred for AVR and actually treated by AVR (with or without concomitant CABG) within the department of cardiac surgery of our institution, the same variables mentioned above were collected in these patients over the same time period, except for antecedent myocardial infarction and PCI. In those patients referred for AVR, only the infarctions within 90 days were collected, while in the PAVR referred patients, antecedent infarction was defined irrespective of its timing. Antecedent PCI was not registered in patients directly referred for AVR.
Follow-up
Follow-up of vital status (mortality) was obtained by contacting the civil registries and by reviewing the hospital records. If necessary, the general practitioner was contacted. Follow-up was complete in all patients.
Statistical methods
Continuous variables are presented as mean ±standard deviation. To compare the different groups analysis of variance was used for the continuous variables and the chi square test for categorical variables. Cumulative survival are presented as Kaplan-Meier curves.
The group of patients referred for PAVR were compared with those patients directly referred for AVR using student’s t-test for continuous variables and the chi square test for categorical variables.
Results
From September 2005 until September 2007, 100 patients with aortic stenosis were referred to the outpatient cardiology clinic for the assessment of eligibility for PAVR. Their baseline demographics and final treatment are depicted in Table 1.
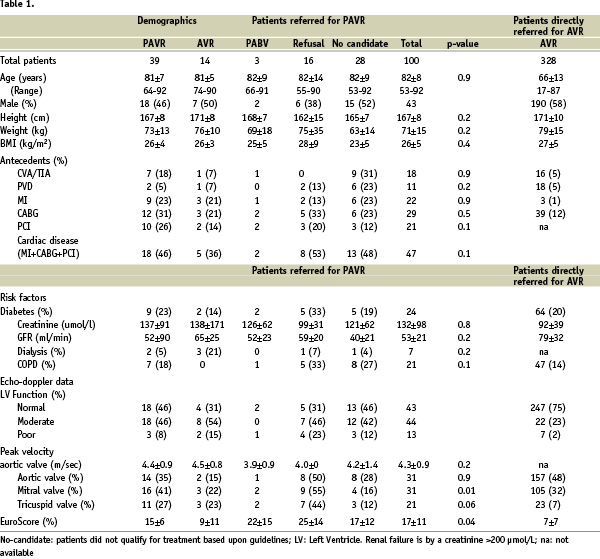
The mean age of the total population was 82± 8 years and 57% were female.
Fifty-six patients received treatment, with PAVR being used in 39 patients, AVR in 14 and PABV in another three patients (Figure 1).
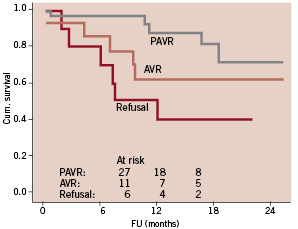
Figure 1. Patients referred for percutaneous valve replacement.
PABV was performed ahead of PAVR because of overt heart failure. Another 28 patients were not considered as candidates for PAVR because of insignificant stenosis (11 patients), absence of symptoms in the presence of significant aortic stenosis, but normal LV function (three patients), severe co-morbidity (12 patients) or aortic annulus size that does not allow for CRS implantation (two patients).
A further 16 patients refused treatment despite indication for valve treatment. They refused treatment because of personal reasons (reluctance to undergo a major procedure) except for one. This last patient was a 55 years female who withdrew consent for treatment after the correction of a coarctation aorta (stent) complicated by an occlusion of the external iliac artery for which she received urokinase in combination with stent implantation.
With respect to the baseline characteristics, average age of the patients treated with PAVR and AVR was 81 years. Furthermore, the antecedent neurological diseases present in the PAVR and AVR group was 18% and 7%, respectively, cardiac disease 46% and 36%, diabetes 23% and 14%, COPD 18% and 0% and renal impairment (GFR 52±90 and 65±25 ml/min). The logistic EuroSCORE was the highest in those patients who refused treatment (25%). It was 15% in patients treated by PAVR and lowest in the AVR group (9%).
During the same time period, 328 patients were directly referred for AVR to the department of cardiac surgery. They were younger than the 100 patients referred for PAVR (66 vs 82 years, p-value < 0.0001), they were more often male (58 vs 43%, p-value < 0.0001), had less antecedent neurologic (p-value <0.0001) and AMI and CABG (p-value <0.0001) (Table 1). They had a similar prevalence of diabetes (20 vs 24%, p-value: 0.36), but patients referred directly for AVR had more frequently preserved renal function (GFR: 74 ml/l vs 53 l/min, p-value<0.0001) and ventricular function (75 vs 43%, p-value<0.0001). The logistic EuroSCORE was 7 and 17% respectively. This difference in demographics, antecedents, comorbid conditions and risk as opposed to the patients referred for PAVR, was also seen when the patients were directly referred for AVR.
The observed mortality and follow-up (months, mean with sd) of the patients referred for PAVR are summarised in Table 2.
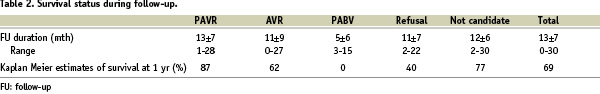
The mean follow-up of the cohort of 100 patients was 13±7 months. The cumulative survival percentages at six months were 97%, 85% and 70%, for PAVR, AVR and refusals, respectively. At 12 months, it was 87%, 62% and 40% respectively (Figure 1).
Discussion
By means of a prospective cohort study, we identified the characteristics and treatment assignment of 100 patients with aortic stenosis referred for PAVR because they were deemed ineligible for surgical valve replacement. Previous studies disclosed that 30% to 60% of patients with severe aortic stenosis are not referred because of the perceived risk of the operation.1,9-13 This especially holds true for the very elderly, patients with impaired ventricular function and/or associated co-morbidity.9 The advent of PAVR has opened a new referral pattern focussing on this population.
In a period of two years, 100 patients were referred to the outpatient clinic after the initiation of PAVR and our informing referring physicians about this service. These patients were beyond the 328 patients who were directly referred to the department of cardiac surgery of our institution for AVR during the same period. In other words, since the initiation of PAVR in our institution the referrals increased 30%. It is conceivable that even more patients could have been seen at the outpatient clinic since PAVR is still in an early phase with limited experience and with few studies describing early and midterm outcome.19-21 At this stage of the technology and service offered, patient, general physician and treating cardiologist related factors involving awareness, personal preferences and opinion must have played an important role in the referral process.
This also holds true for the distribution of treatment. The present study is not only limited to a single centre that had initiated a PAVR program in 2005, but also is observational in nature and not a randomised comparison. Taking into account these issues, approximately half of the patients underwent aortic valve treatment (PAVR, AVR, PABV) and half received or were assigned to medical therapy (refusal, no-candidate). With increasing experience and improvements in the technology it is expected that more patients will be treated by PAVR and that treatment allocation will also be made more swiftly. A premise that we believe will also hold for other institutions and practice. On the other hand, we also observed that 14 patients initially referred for PAVR underwent AVR. This may reflect that the referring physician does not always appreciate precisely the surgical risk and, hence, may unjustifiably withhold patients from treatment and/or that the surgeons are prepared to operate upon higher risk patients as a result of the availability of PAVR. Patients referred for PAVR but treated with AVR had an intermediate risk in comparison to patients referred for PAVR and treated by PAVR and those who were directly referred for AVR (EuroSCORE 9, 15 and 7%, respectively).
Patients treated by PAVR were older and more often female, had a higher prevalence of antecedent cardiovascular disease, diabetes, renal impairment and pulmonary disease than patients treated by AVR – irrespective of the initial referral. This fits with surgical practice in which, in general, patients with these characteristics are more likely to be declined surgery. This is seen in the EuroSCORE which was 15% and 9% in the patients referred for PAVR and treated by PAVR and AVR, respectively. It was only 7% in the patients directly referred for AVR and treated by AVR. As mentioned in the paragraph above, the availability of PAVR may push the surgical envelope as reflected by the 14 patients with a median EuroSCORE of 9% who underwent AVR although initially referred for PAVR.
Although it is unknown whether the present cohort of 100 patients deemed ineligible or too high-risk for AVR represents the 30 to 60% of patients who until now are not referred, it is reasonable to assume they do. Medical professionals and authorities defining the need and content of future medical programs can use both the quantitative and qualitative aspects of these patients. This is particularly important considering the relation between disease prevalence and age on one hand and an ageing society on the other, as well as in view of the relation between age and co-morbidity.3,14 Given the predicted burden of the disease and the demographics of the future patients in relation to the projected role here of PAVR, it is imperative to enhance the safety and applicability of PAVR by improving the technology itself.3,17,22 At present the technology is quite bulky and cumbersome to apply. Miniaturisation is essential to offer PAVR to patients with advanced peripheral atherosclerosis. It will also improve safety by reducing access site complications and make the procedure more straightforward and shorter. This is not a trivial issue in complex cardiac interventions, especially in the elderly with diffuse atherosclerotic disease. Perceptibly, the application of PAVR will move to less ill and younger patients, as well as also moving towards the referral of patients with more advanced age as technology improves, experience increases and as more outcome data becomes available. Demand from society as well will play a role, since a less invasive procedure is usually preferred when it provides equal or superior safety and efficacy in comparison to AVR. The latter can only be documented by randomised clinical studies on the basis of which treatment proposals and eventually decisions could be made.
With respect to the outcome, the most striking observation was that patients who refused treatment had the highest mortality (excluding the three patients treated by PABV). This study was not designed to assess the natural history of untreated aortic stenosis, it confirms the observations made four decades ago when treatment was less available and addresses the demand for information about contemporary history.4,23 Not unexpectedly, the outcome in patients treated with PAVR and AVR was better than those who refused treatment.
Limitations
The present study reports patients referred for PAVR seen at the outpatient cardiology clinic. We have no information of the total number of patients who potentially could have been referred. Therefore, we lack the complete picture of this population in terms of demographics, characteristics, medical history and co-morbidity. In addition to the completeness of referral and, thus, referral bias, generalisations may be limited by the fact that the present population stems form a tertiary academic centre.
The observations of treatment assignment and outcome must be interpreted with caution since it concerns an observational and not a randomised study. Patients were assigned to treatment following a multidisciplinary discussion. Treatment assignment will change depending on experience, ongoing clinical-scientific protocols, further improvements in technology and the acceptance and demand of PAVR by the medical community and society.
Treatment assignment was based upon a multidisciplinary discussion in which the euroSCORE was used. Yet, the total picture of the patient played a more important role in the treatment decision than the euroSCORE given the fact that this score does not really capture the preoperative risk in this cohort, pathology and treatment.23
With respect to the findings on outcome, the observational nature of the study precludes the definition of the role of PAVR in relation to AVR. This also holds for the role of PAVR on survival, since in this cohort of elderly patients, the presence of comorbid conditions may heavily affect survival.
Conclusions
As a result of the initiation of PAVR, 100 new patients deemed ineligible or at too high-risk for surgical valve replacement were seen. Thirty-nine (39) of these received PAVR and 14 AVR although referred for PAVR. Another 28 patients were considered as no eligible for valve replacement. The AVR treated group had the lowest risk, but a higher mortality than patients who underwent PAVR. Patients who refused treatment had the highest risk and mortality.

