Nobody can speak on behalf of Andreas Grüntzig, certainly not me. Yet if he was to come back, for sure, he would be entitled to be immensely proud of his achievements. His legacy has translated into several new chapters in the history of medicine, pushing every other discipline, not just cardiovascular care, towards less invasive forms of treatment, by launching a new era of device-based therapies.
Our field has blossomed at an incredibly fast pace, through relentless imaginative research and daring innovation, all of which only became possible thanks to the billions of entrepreneurial investment that went into the cycle of inventing, developing, studying, validating and eventually marketing new devices.
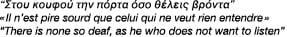
Take for instance percutaneous coronary intervention (PCI). The technique has matured through successive quantum leaps of technological improvements, from plain old balloon angioplasty to the currently available sophisticated drug-device combinations. Indeed drug-eluting stents (DES) have reduced drastically restenosis rates, at last. Since – and because of the increased durability of its results – indications for PCI have expanded and many of the previous standards of care have been disrupted or made obsolete.
Paradoxically, now that the technique has reached adulthood at the advanced age of 30 and has become more efficacious than ever before, its value is being strongly challenged, if not questioned. The late recognition of the rare safety issues that are associated with DES1 has triggered a period of intense scrutiny, scepticism and sometimes animosity on behalf of non-invasive cardiologists, cardiac surgeons, journalists or lawyers. The publication of randomised trials that do not favour indiscriminate use of PCI such as OAT2 or COURAGE3 fuelled the opposition even further. Allegedly, too many patients are submitted to device-based therapies, some of which are either insufficiently validated or poorly indicated. Above all, PCI specifically is not cost-effective and the value for money of DES is limited. Third parties are increasingly often inclined to divert resources from PCI into other life-saving therapies.
The reaction of the colleagues in the field has often been emotional, particularly in the United States. Attitudes have included paranoia, denial, mud wrestling or autism, all being obviously inappropriate. Others colleagues kept exposing the wealth of trial-based evidence that supports the use of PCI and other device-based therapies; yet, the magic is gone. The scientific validity of the evidence that we have accumulated is shaken. The robustness, the relevance, if not the honesty of the reported data are questioned altogether. In the eyes of many, we, interventional doctors, seem to have lost a great deal of our credibility.
Perhaps it is time to reflect upon ourselves. Did we indeed go wrong and if we did, when and why?
The present editorial is an analytical (at times psychoanalytical) exercise that attempts to understand why we got in trouble, what should perhaps be done differently and how we can possibly restore professional leadership. These thoughts have matured over several months and some of the arguments were presented in London on January 23, 2008 at the annual conference of the British Cardiovascular Interventional Society (BCIS).
The present editorial is outspoken and not politically correct. The risk does exist that malevolent readers will use statements out of context, to serve their own interest. My only hope is to stimulate your thinking and perhaps, contribute at least in part to triggering the big change that is needed, urgently, or else we may soon lose our freedom to operate.
Too much focus on the technical
Today, PCI and other device-based interventions are mostly perceived as stand-alone, technically-driven procedures. Unfortunately, they are seldom considered as an additional mode of therapy that is complementary to already existing ones.
Because of the very nature of the daily activity of the interventional cardiologist working in the catheterisation laboratory, much of her/his attention has been focused on instrumental, technical issues. Our field has remained very much a “work in progress” from the onset. As a result, evaluating the latest device iteration, keeping up with the most recently released tool-kit and learning how to adequately use the more complex technologies (typical examples are rotary ablation or vascular brachytherapy), has consumed a lot of energy. Less attention was given to equally relevant clinical matters. The situation is very different with surgical procedures. Surgeons undergo extensive and long-lasting periods of training during which technical matters are dealt with in great detail. Once fully trained, the surgeon reproduces the painfully acquired know-how during immovable “operating” procedures. Instead, we seem to be continuously running after the latest innovation and eager to test the newest approach, a perceived “must” since the field is constantly making progress. There are however major drawbacks. All that is new is not necessarily worth the change. Many novelties do not portend a significant incremental improvement, sometimes the opposite. Resources and energy are wasted on trivia and the more global perspective is easily lost given the excessively narrow focus on the technical.
Device-oriented instead of patient-oriented evidence
Our key opinion leaders are often stressing the fact that progress in interventional cardiology is supported by numerous studies and trials, unsurpassed by any other medical discipline. Correct. However, the overwhelming majority of these trials are addressing technical matters, use surrogate endpoints, mostly derived from mandated repeat angiography, and did initially not require follow-up beyond one year after device implantation. This is candidly acknowledged by the consensus publication of the Academic Research Consortium which stated the following:
“The optimal basis for DES evaluation should be overall cardiovascular outcomes from the patient’s perspective...These outcomes reflect the complex interplay between device performance, revascularisation strategy, secondary prevention, and key patient descriptors.”
Instead, the vast majority if not all published stent trials have addressed device-oriented endpoints. Consequences are far-reaching: device-oriented randomised studies are financed, designed, powered, conducted, analysed and reported under tight control by the industry. The questions asked pertain to superiority or equivalence of one device versus the other, leaving essential clinically-oriented questions unanswered. Hoping to provide the data that would justify the replacement of the old (cheap) by the new (expensive) device, trials failed to ask which patient or lesion subset would benefit most from treatment with the new and more effective device. Physicians did extrapolate the outstanding results obtained in selected populations to all-comers. At the end of the day, much was known about the results of DES in those who needed them the least (on label use). Limited randomised data or observational data of lesser quality derived from post-marketing surveillance registries only provided weak evidence to support the use of DES in patients and lesions subsets needing them the most (the so-called off label use). Very disturbing to regulatory authorities was the observation that the reduction in restenosis seemed to be smaller (by half!) in real life practice than in low-risk, selected trial populations5,6. This is because protocol mandated repeat angiography artificially inflates (doubles) re-intervention rates. Not surprisingly, independently performed health technology assessment studies turned out to be unfavourable. When the interrogations regarding the long term safety of DES exploded, both the profession and the industry were initially unable to provide definitive answers. The matter is indeed complex since death and myocardial infarction, the most frequent clinical presentations of stent thrombosis, are at the same time part of the natural history of coronary disease itself7. However it soon appeared that stent thrombosis rates had been initially underestimated due to the restrictive definitions applied in the trials. In addition, one has to admit that none of the randomised trials on DES are adequately powered to address without ambiguity clinical outcome and hard event rates. Diametrically opposite conclusions were drawn from two different meta-analyses of the same randomised dataset. In this Journal8, Daemen and Serruys were blaming regulatory bodies in Sweden for overreacting to the SCAAR I results. I am afraid that the regulatory yo-yo only mirrors the data yo-yo. Still today, one set of registry data is claimed to show mortality benefit, another set shows the opposite, while none of such data can reliably make this type of statement. Perception by the outside world is dreadful: we do not know what we are talking about, and in any case, as a group, we can barely be trusted...
Patterns of interventional behaviour
It appears that the frustration accumulated during decades of failed attempts at fighting in-stent restenosis was released at once with the emergence of DES. Irrational behaviours were liberated leading to enthusiastic application of PCI in the absence of evidence to virtually all possible subsets, including unprotected left main stenosis in good surgical candidates or patients with multivessel disease and diabetes. Soon, the catharsis was somewhat tempered by concerns of escalating costs for multiple stenting and late stent thrombosis. Unfortunately, some of us seem not to realise to which extent skewed behaviours may potentially degrade the credibility of our profession: self-referral, conflict of interest issues, intervention driven by oculo-stenotic reaction, poor or incomplete patient information. Still today, demonstrations of arrogance, show-off or silly humour remain all too frequent during live courses or lectures. What is the purpose of projecting these damaging slides presenting begging surgeons queuing in the unemployment line? In reality, we all know that adequate problem-solving requires a team approach. In this edition of EuroIntervention Journal, we discuss the power of consensus-based decision making, to the best interest of patients9. Together, we achieve more...
Repairing professional credibility and leadership
Restoring professional leadership will be necessary to balance short-term demands with long-term needs, the continued drive for technological innovation with the legitimate right of patients for improved long term outcome. The current general attitude of interventional cardiologists towards innovation is characterised by enthusiastic, immediate endorsement. A healthy dose of scepticism needs to be re-introduced. Physicians should refrain from compromising with the agenda of the industry. In the long-term, confusion of interest is potentially damaging for everybody, including our industrial partners, as demonstrated by the current situation. In their thoughtful editorial, Harrington and Califf10 are advocating a different partnership with industry as well as with regulatory bodies and payers, involving self-control and respect of each others’ prerogatives and expertise. Clearly, the strength and duty of practising doctors, even invasive cardiologists, is to speak on behalf of their patients and to concentrate on patient-centred issues. Of course, the burden of the proof for technical matters belongs to the industry. However once the new product has been sufficiently validated to enter the clinical scene, independent modes of investigation as well as alternative funding should be secured, particularly when it comes to studying strategic issues regarding the respective role of different modes of therapy.
Percutaneous cardiovascular intervention: overrated as a technology, undervalued as a therapy
The excessive focus on technicality and the never ending public controversies on the respective merits of discrete products, often held on the market place (literally), have contributed to devaluate percutaneous cardiovascular intervention as a therapy and those who practice it, as a professional group. We ourselves have allowed the scope of our field to shrink down to material trivia, while failing to promote the life-saving indications of these procedures. When applied to patients with acute presentations of the disease, PCI is indeed reducing mortality, non-fatal infarction and stroke, with treatment effects superior to any other strategy. Providing this service to the community, improving procedural outcome through innovation and promoting implementation and proper funding with regulatory bodies and payers shall be the principal focus of our action. Taking the lessons from a recent past will hopefully prevent similar mistakes to be repeated, as we engage in the percutaneous treatment of structural and valvular heart disease.