As you can imagine, there is a short delay between the moment I write this opening editorial and the moment it is published. The idea behind this intro is to present the Journal without too many preambles or complexities to give readers an immediate sense of what they will find in the following pages. At the same time, it is a means of highlighting the Journal’s key information and contextual elements. Now, if there is a problem that I had not foreseen in these first months of directing EuroIntervention, it is that at a certain point a pandemic would come to render obsolete any attempt to refer to “the present” in my opening editorials. In recent months, the COVID-19 infection has travelled so quickly that any effort to catch it with words on paper is in vain. The emotional and instantaneous grammar of Twitter probably gives a better idea of things happening on a daily basis, although it loses perspective. So, if I may offer you a suggestion which I learned recently – when you write an editorial that will be published some weeks after you write it, be careful not to mention the upcoming date of a large international congress because it could be cancelled. Or become digital, but that is another story.
Now, considering that this editorial will be published in June and I am writing it a few weeks in advance, I would like to write and predict that everything went well and that the nightmare of SARS-CoV-2 is behind us, but I know that it cannot be like this. And, if so, I would be happy for once to deliver something wrong and obsolete to the publisher, e.g., saying that we are still in the midst of the pandemic and that the pandemic continues to claim victims, while it is not. To date, we don’t know how long this disease will continue to monopolise attention. As I write, many countries have already started the coexistence phase; however, it is not known whether relaxing the containment measures has been an effective idea. Definitely better not to venture into forecasts and move on to the presentation of this issue which as always is full of opportunities to escape current events and remind us what our real job is when we are not improvised infectious disease specialists or epidemiologists.
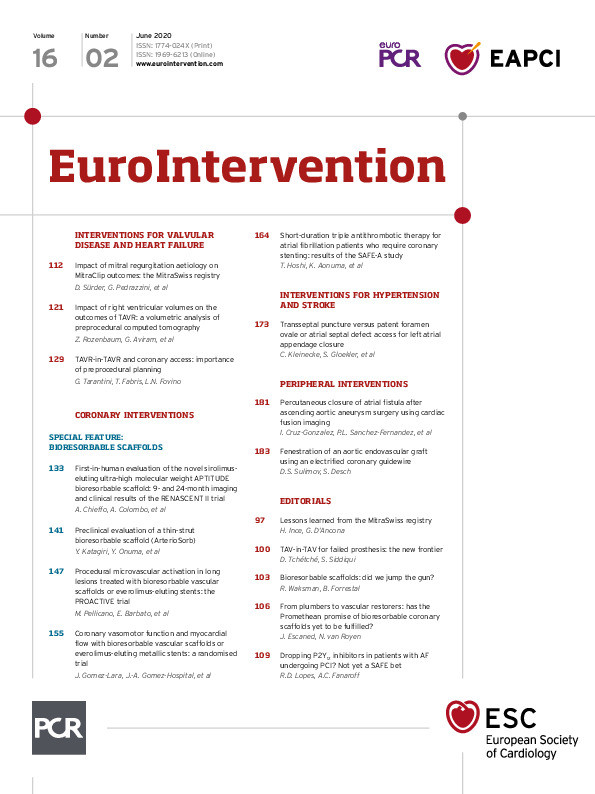
In the section on interventions for valvular disease and heart failure, this month we start with the MitraSwiss registry, as reported by Daniel Sürder, Giovanni Pedrazzini and colleagues. The authors looked at the midterm outcomes of 1,212 patients treated with transcatheter mitral valve repair with the MitraClip system and stratified such outcomes by aetiology (degenerative or functional). Interestingly, they explored independent predictors of mortality at 5 years and found that some of them (the usual suspects) overshadowed the impact of aetiology by itself. Indeed, in MitraSwiss, the rates of mortality were quite high in both cohorts of patients with degenerative and functional mitral regurgitation who were offered MitraClip therapy. So, once again, when you have to predict the outcomes of your patients, regardless of what procedure you are considering, three aspects carry a high prognostic significance – age, ejection fraction, and renal function. A fourth one – anaemia – is less consistently reported in the literature but may come as no surprise. The study is accompanied by an editorial by Hueseyin Ince.
Computed tomography is part of the diagnostic workup of the vast majority of patients undergoing transcatheter aortic valve implantation (TAVI). While this test provides important and useful information for procedural planning, the following study reminds us that there is even more to gain from it. A clinical research paper by Zach Rozenbaum, Galit Aviram and colleagues sought to assess the prognostic implications of having a large right ventricle volume in 323 TAVI candidates. A volume index was calculated by an automatic 4-chamber volumetric software and patients were stratified by quartile. Fourfold increased mortality at 1 year was noted in the highest quartile (>83 ml/m2), a difference that did not stand up to propensity score adjustment for clinical and echocardiographic characteristics. Yet, further exploring the first quartile, they discovered that the 5th percentile (>120 ml/m2) actually retained statistical significance after propensity score adjustment. It is of note that 68.7% of patients from this group would have been considered low to intermediate risk for surgery. This finding suggests that the implications of having a large right ventricle as assessed by computed tomography are not well captured by the available surgical risk calculators.
Finally, also on the subject of preprocedural planning, Giuseppe Tarantini, Tommaso Gabris and Luca Nai Fovino discuss the issue of coronary re-access in candidates to the TAVI-in-TAVI procedure, which is going to become a more and more important topic in the near future. With a richly illustrated study and perspective, they reach several important conclusions that may be full of practical implications at the time of selecting the bioprosthesis to implant in younger patients with longer life expectancy. The study is accompanied by an editorial by Didier Tchétché.
In the section on coronary interventions, this month we host a minifocus on the present and the future of scaffold technologies. It is difficult to foresee how these devices can have a comeback without positive data from large supportive randomised trials, but one has to start again from somewhere, right? In the RENASCENT II study from Alaide Chieffo, Antonio Colombo and colleagues, accompanied by an editorial by Ron Waksman, the focus is on 60 patients who received the 115-micron-thick APTITUDE scaffold, which features relatively high mechanical strength, expansion capabilities and resistance to fracture. With 77% of post-dilatation in their series, the authors achieved nearly perfect device success in the typical lesions you can expect in this kind of trial, and target vessel failure at 9 months in 3.4%. Interestingly, angiographic follow-up data are also reported at 9 and 24 months. From humans to experimental models, Yuki Katagiri, Yoshinobu Onuma and colleagues report on the preclinical evaluation of the acute-phase invasive imaging assessment and haemodynamic implication of another thin-strut (95-μm) bioresorbable scaffold (ArterioSorb) and compare it with metallic drug-eluting stents. The study includes sophisticated quantitative coronary angiography, optical coherence tomography and computational fluid dynamics analyses to provide readers with a full overview of the potential strengths and weaknesses of this device. Two more studies explore the putative advantages of first-generation coronary scaffolds. While these devices are no longer on the market, these investigations, accompanied by an insightful editorial by Javier Escaned, provide some mechanistic insights that may inform future directions in the field. In the PROACTIVE trial, Mariano Pellicano, Emanuele Barbato and colleagues randomised patients with long lesions to scaffolds or metallic stents, and compared them on the basis of procedure-related microvascular impairment and the relationship between platelet activation and microvascular function with related myonecrosis. Another randomised study of scaffolds or metallic stents from Josep Gomez-Lara, Joan-Antoni Gomez-Hospital and colleagues compared the two devices on the grounds of hyperaemic flow and vasomotor response to endothelium-dependent stimuli.
EuroIntervention is also a journal of interventional pharmacology. Therefore the readers should not be surprised by the publication of studies such as SAFE-A, a randomised controlled trial from Tomoya Hoshi, Kazutaka Aonuma and colleagues who compared 1-month and 6-month P2Y12 inhibitor therapy in combination with aspirin and apixaban for patients with atrial fibrillation who require coronary stenting. In a way, it is a trial of shorter versus longer dual antiplatelet therapy in anticoagulated patients, similar to the previous ISAR-TRIPLE trial which, however, used vitamin K antagonists instead of the direct oral anticoagulant apixaban. Unfortunately, the study was terminated prematurely because of slow enrolment and did not carry sufficient statistical power to assess the differences in the primary endpoint. However, we do not like publication bias here, and find that the exploratory findings of SAFE-A are worthy of reporting as a further piece of the mosaic. An authoritative editorial from the AUGUSTUS primary investigator Renato D. Lopes helps us to synthetise where we are with the topic of combined antiplatelet and anticoagulant treatment in patients with atrial fibrillation undergoing stenting.
This and more in the June issue of the Journal. Let’s hope that even the most pessimistic COVID-19 forecasts have been proved wrong next month. As always, please do not hesitate to let us know your opinions, suggestions and reactions, on the website or through social media, to what you read here.
Supplementary data
To read the full content of this article, please download the PDF.