Abstract
Aims: Elderly patients are increasingly being referred for percutaneous coronary intervention (PCI), but there is a paucity of current data on the long-term outcome of elective PCI in elderly patients. We sought to define the risks facing elderly patients undergoing contemporary PCIs.
Methods and results: Retrospectively, in a single-centre registry, we studied the mortality and the outcome of 512 consecutive patients > 75 years old who underwent PCI, between January 1st 2000 and December 31st 2001. Clinical endpoints included in-hospital mortality; major adverse cardiovascular and cerebro-vascular events (MACCE) defined by the components of death, myocardial infarction, stroke, and repeat coronary revascularisation (target vessel revascularisation or not) by surgery or PCI, within the hospitalisation period and at long-term follow up. We compared 315 patients 75-79 years old (group I) with 197 patients > 80 years old (group II).
In-hospital mortality and MACCE rates were not different between the two groups. Independent predictors of in-hospital major events found by multivariate analysis were: ST-segment elevation myocardial infarction or STEMI (Odds Ratio [OR]=2.58, 95% CI=1.15-5.78), left ventricular ejection fraction or LVEF <40% (OR=4.98, 95% CI=2.19-11.36) and prior coronary artery bypass grafting or CABG (OR=3.13, 95% CI=1.06-9.26). Mean long-term follow-up was 51.3 months. Death was significantly more frequent in the older group (42% vs 26%, p<0.0001). Independent predictors of long-term mortality found by multivariate analysis were: LVEF < 40% (Hazard Ratio=4.12, 95% CI=2.69-6.32), creatinine rate (HR=1.00, 95% CI=1.00-1.006) use cut-off see table and prior carotid surgery or stroke (HR=2.2, 95% CI=1.19-4.14).
Conclusions: Although age is not an independent predictive factor of morbidity or mortality, co-morbidities in the elderly strongly influence long-term clinical outcomes after PCI.
Introduction
Cardiovascular disease is a leading cause of morbidity and mortality in the elderly and these patients are increasingly referred for percutaneous coronary intervention (PCI). Demographic changes in the population of western countries has resulted in an increase in the number of elderly patients hospitalised for cardiovascular disease. Patients enrolled in coronary intervention trials or in randomised controlled trials for acute coronary syndromes (ACS) are not representative of patients in clinical practice1,2. The most common cut-off in trials with an explicit age exclusion is 75 years. Although some trials did not have protocol-based age exclusions, they still failed to enrol any elderly patients. There is a wide gap between the proportion of myocardial infarction patients aged 75 years or older in western countries and their enrolment in all randomised controlled trials on ACS1.
Older patients show more severe, complex, multiple and calcified coronary artery lesions than younger patients3-5. The majority of previous studies of outcomes in elderly patients undergoing PCI and CABG surgery report less successful revascularisation and more adverse outcomes6,7. Advances in coronary angioplasty and greater operator experience have led to a decrease in the rate of complications related to PCI. There is a paucity of current data on the long-term outcome of elective PCI in elderly patients.
The present study assesses retrospectively, in a single-centre registry, the long-term clinical outcome after PCI in patients aged over 75.
Methods
Study population
We performed a retrospective analysis using the Rangueil University Hospital Interventional Cardiology database for patients enrolled between January 1st 2000 and December 31st 2001. The outcomes of 315 consecutive patients between 75 and 79 years old undergoing PCI were compared to those of 197 consecutive patients aged > 80 years.
Medication and PCI
PCI and intracoronary stent implantations were performed using standard percutaneous techniques. Each operator relied on his own judgement or on objective measurements, such as online QCA, to assess stent expansion. All patients were on aspirin and received heparin bolus per-procedure. Patients received either clopidogrel (75 mg daily) or ticlopidine (250 mg twice daily), continued for at least four weeks. Other cardiovascular medications (β-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, amiodarone) were administered at the discretion of the physician, with no difference between the two groups.
In-hospital outcome, long-term follow-up and clinical endpoints
Clinical characteristics and procedural information, including angiographic data and complications, were recorded prospectively during the in-hospital period and at follow-up. Long-term follow-up was achieved in December, 2005. The mean length of follow-up was 51.3 [0.1-69] months. Endpoints were mortality, major cardiovascular and cerebrovascular events (MACCE). In-hospital MACCE included death, re-PCI in the target lesion, CABG, stroke, MI and cardiogenic pulmonary oedema. Long-term MACCE included: death, re-PCI in the target lesion or in others lesions, CABG, stroke, and MI.
Statistical analysis
Statistical analyses were performed with Systats® and Statview® software packages. The data are presented as the mean±standard deviation. Differences in baseline characteristics were evaluated with a Student t test for continuous variables and with a χ2 test for categoric variables, or a Fischer exact test if appropriate, and a P value of <0.05 was considered significant. In-hospital outcome was treated by logistic regression. Results are expressed by Odds Ratios. Differences in survival and event-free survival rates between the groups were evaluated with the Kaplan-Meier method. Comparisons were made with a log-rank test. For the clinical variables, multivariate analyses were performed with the Cox proportional hazards model to assess any association with combined events. Backward stepwise regression analysis was performed to assess which factor was independently associated with the endpoint.
Results
Patients’ characteristics
In a single-centre registry, a total of 2,857 catheterisations for ischaemic heart disease with 1,943 PCIs were performed between January 1st, 2000 and December 31st, 2001. Of the 1,943 PCIs, 512 (26%) patients > 75 years underwent angioplasty of at least one coronary vessel. This cohort was divided into two groups 315 patients aged 75 to 79 years formed group I and 197 patients aged 80 and over made up group II. Few differences were observed between the two groups. Patients over 80 years and older had significantly less dyslipidaemia or history of smoking and less prior CABG (Table 1).
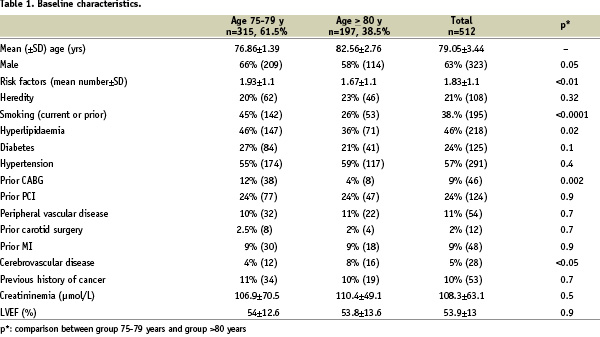
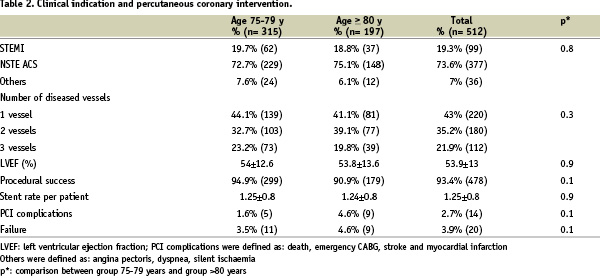
For 476 (93%) patients, the indication for performing PCI was an acute coronary syndrome (STEMI or NSTE ACS) without significant difference between the two groups. The number of diseased vessels was not different between groups I and II. Only 22O (43%) patients had one diseased vessel (Table 2).
The mean left ventricular ejection fraction was 53.9±13. Fifty-three (10.4%) patients had previous history of cancer.
In-hospital management, percutaneous coronary intervention
Procedural success rate was 93.4% (n=478). All PCIs were performed with bare metal stents, and the number of stents per patient was 1.25±0.8. Complications during PCI were defined as: death, emergency CABG, stroke and myocardial infarction. Procedural outcome was similar between the two groups (Table 2).
In-hospital outcomes and predictors of in-hospital MACCE
In-hospital major cerebrovascular and cardiovascular events (MACCE) were defined as: death, re-PCI in the target lesion, CABG, stroke, MI and cardiogenic pulmonary oedema. In-hospital outcomes were not different between the two groups (Table 3).
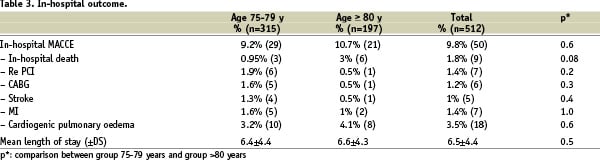
In-hospital MACCE rate was 9.8% (n=50) and the mean length of stay was 6.5±4.4 days. Elective PCI in non-infarct-related arteries was subsequently performed for six (1.9%) patients. After STEMI (n=99, for the two groups combined), in-hospital MACCE were significantly higher (19.2% vs 7.5%, p <0.0001).
Multivariate logistic regression analysis revealed the following independent predictors of in-hospital MACCE: STEMI, LVEF < 40% and prior CABG (Table 4).
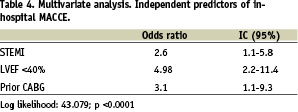
In our selected cohort, age did not appear as an independent predictor.
Long-term clinical outcome
The mean long-term follow-up was 51 months (range 0.1 to 69 months). Twenty patients (3.9%) were lost, with no follow-up after they had left the hospital.
At the end of the study, 164 (32%) patients had died. Long-term mortality was higher in the older group: 42% (82) vs 26% (82), χ2=17.058; p < 0.0001. Figure 1 shows the cumulative Kaplan-Meier event-free survival rate curves. Cardiac death was significantly higher in the group II: 25% (49) vs 14% (43); p=0.0003.
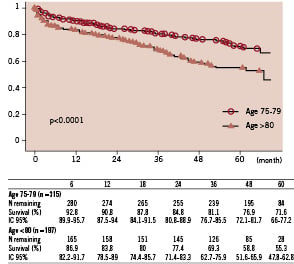
Figure 1. Long-term Kaplan-Meier survival curves of each group. Long-term mortality was higher in the older group: 41.6% (82) vs 26% (82), χ2=17.058; p < 0.0001.
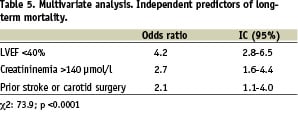
Multivariate logistic regression analysis revealed the following independent predictors of long-term mortality: LVEF < 40%, creatininemia and prior cerebrovascular event or carotid surgery (Table 5).
Long-term MACCE were not significantly different between the two groups: 48% for group I and 56% for group II. Long term MACCE affected 251 (49%) patients of the total cohort. Multivariate logistic regression analysis revealed the following independent predictors of long-term mortality: LVEF < 40% (HR 2.7, 95% CI = 1.85-3.82, p < 0.0001) and three-vessels diseased patients (HR 1.7, 95% CI=1.16-2.41, p=0.006); χ2=47.404, p < 0.0001. Moreover, for both groups the diagnosis of neoplasia was confirmed in 33 (6.7%) patients during follow-up.
Discussion
As life expectancy continues to rise, elderly patients are increasingly referred for PCI. They show more severe, complex, multiple and calcified coronary artery lesions than young patients3-6,8,9. In this contemporary, single-centre, retrospective study, we retrieved long-term clinical outcomes for 512 consecutive elderly patients treated by PCI. Except for the age, the two groups of our study were quite similar. In a recent retrospective study by Peterson et al10, the in-hospital death of 48,439 patients aged > 75 years undergoing PCI ranged from 1.5% to 5.2% across databases, with an average of 3%. In-hospital mortality after PCI in elderly patients, aged > 75 years or > 80 years, usually ranges between 1.2 and 3.8%3,4,9,11-14.
In-hospital mortality and morbidity rates after acute coronary syndrome (ACS) are usually higher in elderly patients. And increasing age is inversely associated with the use of coronary angiography and revascularisation15-17. In the 56,963 patients with NSTE ACS of the CRUSADE study16, the risk of in-hospital death increased continuously with patient age from 7.3% for age 75-84 to 11.5% for age > 85 years. In this study, past the age of 75 years, only 40% underwent early invasive care, and past the age of 85 that number was < 20%. In the GRACE observational registry of patients admitted to hospital with ACS, hospital mortality rate also increased with age.
In the late ACC/AHA/SCAI 2005 guideline update for PCI7, age greater than 75 years is one of the major clinical variables associated with an increased risk of complications. In octogenarians, although feasibility has been established for most interventional procedures, the risks associated with both percutaneous and non-percutaneous revascularisation are increased. We report that, with appropriate case selection, these interventions can be performed with high rates of procedural success and acceptably low mortality and morbidity. In accordance with the late 2005 guideline for PCI7, we found acceptable in-hospital complication rates for elderly patients treated by angioplasty after acute coronary syndrome.
In-hospital mortality after PCI was low (1.76%) in our selected population.
In our study, age was not found to be an independent predictor of in-hospital MACCE for patients older than 75 years old. Procedural risks, in-hospital mortality and morbidity for elderly patients are strongly influenced by clinical presentation, such as STEMI, or comorbidities such as heart failure or previous CABG. The two largest contemporary studies analysing in-hospital outcomes of elderly patients are those of Batchelor et al12 and Klein et al3. The first used data from the National Cardiovascular Network (NCN) to evaluate in-hospital outcomes on 7,472 octogenarians undergoing PCI. The second used the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR) to evaluate in-hospital outcomes in 8,828 octogenarians undergoing PCI. In-hospital mortality of patients > 80 years of age reached almost 4% in the both studies, and age was found to be an independent predictor of in-hospital mortality.
At long-term follow-up, the study by Graham et al6, using the APPROACH clinical data collection initiative capturing all patients undergoing cardiac catheterisation in Alberta, Canada, the 4-year survival rate for patients > 80 years of age was 77.4% in the PCI group. And revascularisation was associated with better risk-adjusted survival rates compared with medical therapy, especially in patients > 80 years old. Coronary revascularisation is usually associated with significantly better survival in the elderly than medical therapy alone.
Death rate at five years for patients > 80 increased to 35%, in the study by Taddei et al18. This rate is lower than in our study but, in that study, patients undergoing PCI for acute myocardial infarction were excluded, unlike in our cohort which included 93% of ACS.
Despite a significantly higher long-term mortality rate of patients > 80 years old, age does not appear as an independent predictor of morbidity or mortality. Long-term clinical outcomes after PCI in the elderly were strongly influenced by their co-morbidities, such as LVEF <40%, creatininemia and prior stroke or carotid surgery.
Taddei et al18 revealed that age was independently correlated with mortality, and the strongest predictor of death at follow-up, although older patients were sicker with a higher rate of the following co-morbidities: diabetes mellitus, systemic hypertension, heart failure, prior myocardial infarction and multivessel disease. In this study, advanced age, lower ejection fraction, diabetes mellitus, heart failure, systemic hypertension, PTCA in a graft vessel and the number of diseased vessels were all independently associated with decreased survival at long-term follow-up.
Hasdai et al19, at an evaluation with follow-up > 10 years after PCI, concluded that long-term mortality was independently predicted by age > 70, extent of coronary artery disease, diabetes mellitus, and prior or recent myocardial infarction
Although age is not a predictive factor for long-term mortality and MACCE in our selected population of patients older than 75 years old treated by coronary angioplasty, long-term mortality of patients > 80 years of age was significantly higher (41.62%) than for those aged between 75 and 79 years (26.03%).
Study limitations
This study has several limitations. It was retrospective and single-centre. The sample size was small, so it tends to be underpowered to address statistical conclusions. PCI were performed in patients with an acceptable “physiologic” age. Patients not undergoing revascularisation (PCI or CABG), but receiving medical treatment alone were not studied. The results do not reflect outcomes of patients who were not referred for angiography. Moreover, PCIs were performed by experienced operators at a high-volume academic centre. It may not be wise to generalise our results to outcomes of patients in other settings.
Conclusion
Although greater age is associated with a higher rate of mortality, age alone is not an independent predictor of long-term survival in our selected population of patients older than 75 years old. Therefore, age alone should not be a deterrent to performing percutaneous transluminal coronary angioplasty in the elderly. PCI is safe in patients older than 75 years old, and even in selected patients over 80. Patient selection for PCI should not be based on age alone, but other comorbidities should be considered as these are associated with a poorer outcome.

