Abstract
Aims: The European ImproveR registry aimed to characterise the patient population undergoing percutaneous coronary intervention (PCI) with bivalirudin treatment in a routine clinical setting and to evaluate associated ischaemic and bleeding events.
Methods and results: A total of 3,799 evaluable patients, aged > 18 years, were enrolled in 102 centres across 12 European countries from January 2005 to June 2006. The population was elderly (median age, 67.2 years; 24% > 75 years) and comprised 27.1% female patients, 27.9% with diabetes and 14.9% with renal impairment. Forty-nine percent of patients presented with acute coronary syndromes (ACS), 22% of these with ST-segment elevation myocardial infarction (STEMI). In-hospital and 30-day rates of major adverse cardiac events (death, myocardial infarction or urgent revascularisation) were 2.3% and 5.6%, respectively. In-hospital ischaemic complications were associated with a STEMI diagnosis and age > 65 years. In-hospital significant bleeding occurred in 1.7% of patients and was associated with renal impairment, female gender and glycoprotein IIb/IIIa inhibitor use.
Conclusion: The ImproveR registry population is characterised by a high proportion of elderly patients and patients with diabetes, renal impairment and ACS. In clinical practice, bivalirudin effectively suppresses ischaemic complications while maintaining a low rate of haemorrhagic consequences, as expected from randomised trials.
Introduction
Percutaneous coronary intervention (PCI) procedures have evolved considerably over the past 30 years with the advent of improved technologies and adjunct pharmacotherapies. Randomised clinical trials addressing these new developments have helped shape current PCI practice and lead to recommendations that are summarised in European guidelines1. Although data from randomised trials form the cornerstone for the evaluation of new treatment modalities, patients enrolled in such trials are carefully selected through the implementation of strict inclusion and exclusion criteria and, therefore, may not fully reflect patient populations in routine clinical practice2,3. Consequently, data from registries are an important addition to the body of evidence for any novel treatment4,5.
Antithrombotic treatments have previously been evaluated for their efficacy in reducing the risk of ischaemic complications in patients undergoing PCI. More recently, the importance of avoiding related bleeding complications has been firmly established and strong links between bleeding and mortality (both short- and long-term), other ischaemic events, prolonged in-hospital stay and higher treatment costs have been reported in the literature6-10. Bivalirudin is a thrombin-specific anticoagulant, indicated for PCI, that offers non-inferior ischaemic protection compared with heparin plus routine glycoprotein (GP) inhibitor use but with a significant reduction in bleeding complications in all patients, as shown in several randomised trials, including CACHET11, REPLACE-212 and ACUITY13. Bivalirudin has been available in Europe since late 2004/early 2005 and could be an attractive alternative to the conventional heparin-based anticoagulation regimen for PCI because of the significantly reduced risk of bleeding.
The aim of the ImproveR registry was to characterise a European patient population for whom bivalirudin was chosen as a baseline anticoagulant during PCI, and to investigate associated ischaemic and bleeding complications in this population.
Methods
Registry design and patient population
The ImproveR registry was a multicentre, non-interventional registry which included patients (aged > 18 years) undergoing planned or urgent PCI with bivalirudin treatment between January 2005 and June 2006.
Data collection
Data from patients chosen for bivalirudin treatment during PCI were prospectively entered into the ImproveR database. These data were collected for procedures and measurements in accordance with the routine activities of each institute using web-based, electronic data capture methods. Information was recorded at baseline, during angiography, PCI and at discharge. Follow-up event rates were collected at 30 days after PCI in sites where this was routine practice. Data were also collected from patients who consented to 30-day follow-up by telephone. Centres with a follow-up rate of <80% were excluded from the 30-day analyses. All therapeutic decisions, including the decision to perform PCI and use bivalirudin, were made by investigators on an individual case-by-case basis without any requirements defined by the registry protocol.
Registry events and definitions
The primary events recorded included ischaemic complications and the occurrence of clinically significant bleeding during the in-hospital period. Major adverse cardiac events (MACE), defined as death (any reason), non-fatal myocardial infarction (MI), or urgent revascularisation (PCI or coronary artery bypass graft [CABG]), were documented at discharge and at up to 30-day follow-up. As this was a non-interventional registry, occurrence of an MI post-PCI was based on the diagnosis of the investigator. In-hospital clinically significant bleeding was defined as any one of: intracranial, intraocular or retroperitoneal haemorrhage; clinically overt blood loss with a haemoglobin decrease of > 3 g/dl; any haemoglobin decrease of > 4 g/dl; transfusion of packed red blood cells, whole blood or other blood product (or a combination of these); haematoma at puncture site of > 5 cm. A haematoma < 5 cm with clinical consequences in the absence of any other significant bleeding criterion was also included in this definition. The duration of the PCI procedure was defined as the length of time the coronary wire was in the target vessel.
Statistical analysis
Percentages or medians with interquartile ranges were calculated for all major parameters to describe the patient population. To detect independent associations between patient characteristics and clinical events, logistic regression analyses were performed. Variables considered in the in-hospital ischaemic complication analysis were: age > 65 years; ST-segment elevation MI (STEMI); non-ST-segment elevation MI (NSTEMI) or unstable angina; phenprocoumon/warfarin before PCI; bivalirudin single bolus without infusion; bivalirudin double bolus without infusion; unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) < 24 hours after PCI; GP IIb/IIIa inhibitor use; PCI duration > 45 minutes. Factors entered into the in-hospital bleeding complication analysis were: female gender; abnormal creatinine at baseline; UFH/LMWH < 24 hours after PCI; GP IIb/IIIa inhibitor use; radial puncture site; sheath size > 7 Fr; use of closure device or haemostatic pad. Statistical analyses were performed using SAS, release 9.1.3 (SAS Institute Incorporated, Cary, NC, USA).
Ethical and legal aspects
The registry was conducted in accordance with the Declaration of Helsinki14 and followed the definitions of a non-interventional study as detailed in the European Clinical Trial Directive 2001/20/EC15 and the Data Protection Directive 95/46/EC16. Ethics committee approval was obtained where applicable. In most countries, patients were required to give written informed consent for their data to be included in the registry database according to local data protection regulations. In Germany, a random sample of 15% of all patients had their data verified against the medical records. In other countries, patient consent was verified prior to database lock.
Results
Patient demographics and characteristics
A total of 3,799 evaluable patients for whom bivalirudin treatment was chosen as anticoagulation during PCI were prospectively entered into the ImproveR registry database between January 2005 and June 2006 from 102 centres, covering 12 European countries. Table 1 details the number of patients and centres per country.
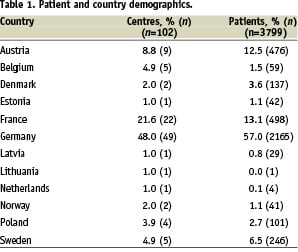
The majority of patients (57.0%) were enrolled in Germany.
Patient characteristics at baseline, including clinical presentation, are shown in Table 2.
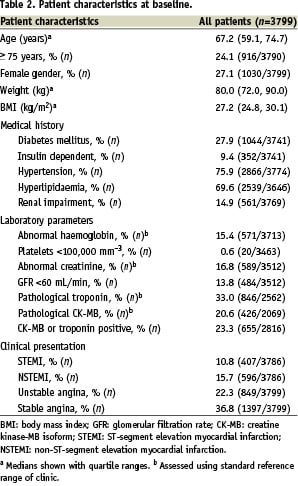
Almost a quarter of patients were older than 75 years. The percentage of female patients, patients with diabetes and those with hypertension was 27.1%, 27.9% and 75.9%, respectively, and 14.9% of patients had a diagnosis of renal impairment.
Laboratory tests at the time of enrolment indicated that 33.3% of patients had elevated levels of creatine kinase MB isoform (CK-MB) or troponin and 13.4% of patients had a left ventricular ejection fraction (LVEF) of < 40%.
Forty-nine percent of patients presented with a diagnosis of ACS. Of these, 22% were diagnosed with STEMI, 32% with NSTEMI and 46% with unstable angina. The remaining patients underwent PCI for an indication of stable angina (37%) or other indications (including proof on positive exercise stress test ischaemia, myocardial scintigraphy, arrhythmia, syncope or congestive heart failure).
Procedural characteristics and concomitant medication
Elective PCI represented 59.4% of procedures performed. In 88.0% of cases a femoral access site was used, with radial (11.5%) or other (0.5%) access being used in the remainder of cases. PCI was performed for single-vessel, two-vessel and three-vessel disease in 33.0%, 30.0% and 35.5% of patients, respectively. The median (quartiles) PCI duration was 30 (20, 45) minutes. Stents were implanted in 75.8% of cases and drug eluting stents were used in 22.1% of procedures. Stent use varied widely between participating countries, with Germany, Denmark and Sweden employing stents in over 80% of procedures (91%, 85% and 82%, respectively), while countries such as Latvia and Estonia used stents in less than 20% of cases (17% and 10%, respectively). A closure device was used in 39.9% of procedures; sheath removal took place directly after the procedure in half of all cases (50.1%), and within 2 hours of the procedure in a further 19% of patients.
The dosing of bivalirudin should comprise a bolus of 0.75 mg/kg followed immediately by an infusion of 1.75 mg/kg/h for the duration of the PCI procedure according to the label. Sixty-six percent of all patients in the registry received a bolus (median [quartiles] dose 0.75 [0.74, 0.76] mg/kg) plus infusion (median [quartiles] dose 1.75 [1.71, 1.77] mg/kg/h) of bivalirudin. A single bolus (median [quartiles] dose 0.75 [0.74, 0.76] mg/kg) was administered to 26.3% of patients and a double bolus (median [quartiles] dose of second bolus 0.74 [0.50, 0.76] mg/kg) to 7.1% of patients, without the following infusion. UFH was administered to 10.3% of patients <30 minutes before PCI, LMWH to 5.8% of patients <8 hours before PCI, and a GP IIb/IIIa inhibitor to 4.7% of patients during PCI (tirofiban 2.6%, eptifibatide 0.6%, abciximab 1.2% and unspecified in 0.3% of patients). Aspirin was used in most cases (91.6%), in line with European guidelines1, and clopidogrel was administered > 2 hours before PCI in 55.4% of patients and < 2 hours before PCI in 18.9% of patients.
In-hospital clinical events
The median (quartiles) hospital stay after PCI was two days (1, 4). In-hospital ischaemic and bleeding events are shown in Figure 1.
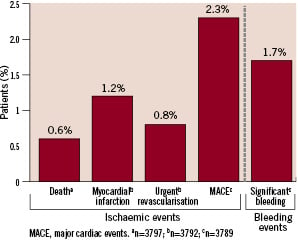
Figure 1. In-hospital ischaemic and bleeding events.
There were 23 in-hospital deaths, of which 12 were considered to be due to cardiac events, eight were considered not to be due to cardiac events, and three were of unknown cause in the opinion of the treating physician. Other ischaemic complications included new MIs in 46 patients and urgent revascularisation in 31 patients. In-hospital clinically significant bleeding events are shown in Table 3.
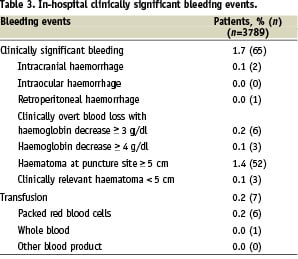
Clinically significant bleeding was experienced by 65 patients (1.7%); 52 patients had a haematoma > 5 cm and 7 patients underwent transfusion.
Ischaemic events at follow-up
Follow-up data at 30 days were available for 2,979 patients (94.4% of evaluable patients in centres where the follow-up rate was > 80%). The cumulative MACE rate at 30 days was 5.6%. The cumulative rates of death, MI and urgent revascularisation were 1.5%, 2.3% and 2.9%, respectively.
Factors associated with clinical events
Logistic regression analyses were performed to detect factors independently associated with in-hospital ischaemic or bleeding events (Figure 2a and b, respectively).
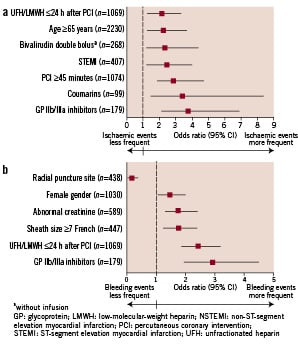
Figure 2. Results of the logistic regression analyses showing risk factors associated with in-hospital ischaemic complications (2a) or in-hospital significant bleeding events (2b).
An increased frequency of ischaemic events was significantly associated with: age > 65 years (p=0.002); a diagnosis of STEMI (p=0.004); a PCI procedure of > 45 minutes (p<0.001); treatment with heparin < 24 hours after PCI (p=0.002); a bivalirudin double bolus without infusion (p=0.009); coumarins before PCI (p=0.006); or GP IIb/IIIa inhibitor treatment during the procedure (p<0.001).
The factors significantly associated with an increase in bleeding events were: female gender (p=0.006); abnormal creatinine (p=0.001); a sheath size of 7 Fr or above (p=0.004); GP IIb/IIIa inhibitor treatment during PCI (p<0.001); and heparin treatment < 24 hours after the procedure (p<0.001). Bleeding also appeared to be associated with the use of a closure device or haemostatic pad (p=0.018; 95% CI 1.43, 43.66).
Discussion
The ImproveR registry characterises the patient population for which bivalirudin treatment during PCI is chosen in current European practice. Bivalirudin has been available in Europe for a relatively short time and has not yet achieved wide acceptance. As indicated by the ImproveR data, there is a tendency for physicians to choose bivalirudin for older patients than those documented in other European PCI registries4,17,18. Additionally, there were higher proportions of patients with diabetes, renal insufficiency and hypertension in the ImproveR population4,17-19.
The mortality and ischaemic complication rates observed in ImproveR are low, especially considering the number of ischaemic risk factors in the patient population. One possible explanation is that the cases were not reported consecutively and thus a selection bias could have been introduced in the registry. Investigators may have had a tendency to include cases reflecting successful PCI procedures or patient consent may not have been given until after the procedure, both of which would lead to a lower incidence of ischaemic complications.
MI rates tend to be higher in routine practice compared with clinical trials20 but this was not seen in ImproveR. As the ImproveR registry was non-interventional, no constraints were imposed upon clinicians in their routine practice, including their method of diagnosing a post-procedural MI, a complication for which there is also no fixed definition in other similar registries4,18. The proportion of MIs described in the literature as clinically ‘silent’ is variable and ranges from 33% to 50%21,22, with the highest silent MI rates reported in patients with diabetes or hypertension, elderly patients and women23,24. Because of this, it must be concluded that the ImproveR MI rate, calculated from routine clinical diagnosis, is underestimated. If we assume that 50% of MIs in the ImproveR study were clinically silent, this would increase the in-hospital MI rate to 2.4% and the 30-day rate to 4.6%. Due to the different methods of defining ischaemic complications in registries and clinical trials, the validity of comparing rates with other studies is questionable. However, the low complication rates observed, even when adjusted to include ‘silent’ MIs, suggest that bivalirudin delivers effective ischaemic protection in clinical practice.
The ImproveR registry allowed the evaluation of bleeding in a ‘real-life’ patient population undergoing PCI with bivalirudin. The in-hospital significant bleeding rate in ACS patients from the ImproveR registry (2.1%) is lower than those reported in ACS registries evaluating PCI with GP IIb/IIIa inhibitor treatment (2.6% in ACOS25 and 5.5% in GRACE26). Moreover, the definition of major bleeding in these registries covered a greatly reduced range of events compared with the ImproveR significant bleeding definition, making the ImproveR results all the more striking. For example, ACOS major bleeding reflected only patients who received transfusions25.
The low use of GP IIb/IIIa inhibitors in the ImproveR registry (4.7%) compared with other studies4,5,27 highlights that bivalirudin is most often administered without this medication. The rate of GP IIb/IIIa inhibitor use with bivalirudin in ImproveR is consistent with data from randomised clinical trials12,13.
Several studies analysing bleeding incidence have reported that an increased rate of major bleeding is associated with factors including advanced age, female gender, renal insufficiency and diabetes7,9,10,17. The high proportion of patients with diabetes or renal insufficiency, and those aged over 75 years in ImproveR suggests that physicians are currently choosing to use bivalirudin in these patient groups due to its favourable bleeding profile. It is noteworthy that despite this population and the broad bleeding definition used, bleeding rates were low.
The logistic regression analyses performed in the ImproveR registry described factors associated with ischaemic or bleeding events but were not designed to distinguish between relationships which were causal/direct or consequential/indirect. As expected, more ischaemic complications occurred in high-risk patients (presenting with STEMI and aged > 65 years)28,29. The associations observed between increased ischaemic events and use of UFH/LMWH < 24 hours after PCI, prior coumarin treatment or a PCI procedure > 45 minutes may be indicative of more severe disease and/or a complex PCI procedure. The significant association of abnormal creatinine levels, female gender, sheath size and the addition of a GP IIb/IIIa inhibitor with increased bleeding events is in accordance with previous study results7,10,12,30,31, indicating that bivalirudin does not pose new bleeding problems.
Limitations
As with all observational studies, there are limitations associated with the ImproveR registry. It is probable that the participating centres are not necessarily a representative sample of all centres in each particular country. Additionally, as 48% of all centres were in Germany, it is likely that the ImproveR registry may predominantly reflect German clinical practice. As there was no central reference laboratory for ECG or laboratory test evaluation, and as adjudication of clinical events was not performed, it is difficult to say to what extent diagnoses and procedures varied between centres. However, these differences will be present in routine clinical practice and thus reflect what would happen in a ‘real-life’ situation. Follow-up data were analysed only for patients in centres with a follow-up rate of > 80% in order to avoid a possible selection bias in those centres with a low follow-up success rate. To investigate whether patients excluded from the protocol-specified follow-up analysis had higher incidences of death and ischaemic complications, we calculated the complication rates for all patients with 30-day follow-up data (n=3214). The rate of death after hospital discharge in the total follow-up population was slightly higher than in the protocol-specified population (1.1% versus 0.9%) but there were no differences between the MI or urgent revascularisation rates. Finally, as with many other registries without a comparator arm, we cannot directly compare the efficacy or safety of bivalirudin with other anticoagulants. However, as different treatments are chosen depending on the risk and profile of patients, comparisons in clinical practice would be indirect and of limited value.
Conclusion
The ImproveR registry has shown that ischaemic complication and bleeding rates were low in patients treated with bivalirudin as a baseline anticoagulant during PCI. Bivalirudin was chosen particularly for elderly patients and patients with diabetes, hypertension and renal impairment. The promising ischaemic efficacy and bleeding rates observed in the clinical setting underline the relevance of results from controlled, randomised bivalirudin trials, thus allowing clinicians to make clearer, informed treatment choices for all their patients.
Acknowledgements
The ImproveR registry was supported by the Nycomed Group, Denmark. Institut für Herzinfarktforschung Ludwigshafen received funding for statistical support of the ImproveR registry. The ImproveR steering committee would like to thank all participating centres and investigators who took part in the registry. The authors would like to thank Laura McMahon for medical writing support during the preparation of this manuscript.