Abstract
Purpose: Failure to recanalize chronic superficial femoral artery occlusions is frequently caused by subintimal passage of the occlusion with inability to re-enter the true lumen with the guide-wire. The present study details our initial experience with the Pioneer crossing device (Medtronic, Menlo Park, CA) to facilitate recanalization of total femoral artery occlusions.
Material and methods: 25 consecutive patients (18 male, mean age 63 years) whose failed recanalization attempts of chronic superficial femoral artery occlusions (mean occlusion length 12.7 cm) with standard techniques were re-scheduled for a secondary recanalization procedure. The Pioneer crossing device is a 6.2F rapid exchange catheter, which tracks over a 0.014”-wire. A 20MHz phased array IVUS transducer is integrated into the tip of the catheter allowing visualization of the vessel morphology. Using the guidance of the IVUS cross-sectional image supported by colour-flow imaging, the true lumen is punctured with an integrated 24G needle allowing delivery of a second 0.014”-wire.
Results: Re-entry into the true lumen was successfully accomplished in all cases without complications. In 8 cases with severe calcification predilatation of the false channel was necessary to allow advancement of the Pioneer crossing device. Furthermore, in 7 patients with severe calcification multiple puncture attempts were necessary to penetrate the dissection membrane. A procedural success (<25% residual stenosis) could be achieved in all cases after predilatation and stenting of the occlusion with self-expanding nitinol stents.
Conclusion: The Pioneer crossing device is an effective and save tool to facilitate true lumen re-entry during recanalization of total superficial femoral artery occlusions.
Introduction
Percutaneous recanalization of chronic superficial femoral artery occlusions is a technically challenging procedure, which is associated with a relevant technical failure rate of up to 25% depending on the lesion length1-3. Inability to re-enter the true lumen after accidental or intentional subintimal passage of the occluded segment is the most frequent condition leading to an unsuccessful procedure.
The present study details our initial clinical experience with a newly developed device allowing an intravascular ultrasound (IVUS) guided penetration of the intimal membrane to facilitate guide-wire re-entry into the true lumen.
Methods
This study was performed within the guidelines of the institutional review board and written informed consent was provided by each patient prior to the procedure. During a six months period in our institution recanalization of chronic superficial femoral artery occlusions was attempted in 96 patients with a total of 104 treated limbs. In 25 cases (24.0%) the recanalization procedure could not be successfully completed due to subintimal passage of the guide-wire with inability to re-enter the true lumen of the patent distal superficial femoral artery.
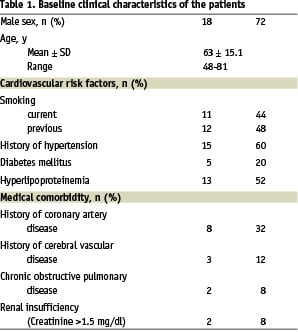
These 25 patients who failed a recanalization attempt with conventional guide-wire technique represent the study cohort and underwent an additional recanalization procedure using a newly developed crossing device. The baseline clinical characteristics of the patients are illustrated in table 1. The mean length of the femoral occlusion was 12.7 ± 5.3 cm with a reference vessel diameter ranging between 5 and 6 mm.
Device description
The Pioneer crossing device (Medtronic, Menlo Park, CA), formerly Crosspoint TransAccess catheter (TransVascular Inc.), is a device designed to facilitate wire re-entry into the true lumen by IVUS guided penetration of the intimal membrane (Figure 1). The device is CE-marked and intended for single use.
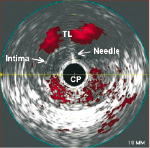
Fig. 1: Pioneer crossing device TransAccess double lumen catheter with puncture needle and integrated phased array 20 MHz IVUS transducer.
It consists of a 6.2 F double lumen monorail catheter which tracks over a 0.014” guide-wire. The tip of the catheter contains an integrated 64 elements phased array 20 MHz IVUS transducer, which works in combination with the Jomed/ Vulcano IVUS console (Josonic In-vision Gold). Based on this technology, the device allows visualization of the vessel morphology as B-mode IVUS cross-sections. Furthermore, a colour-flow mode is available, which helps to identify blood flow in the true vessel lumen. The second lumen of the catheter contains a curved puncture needle for penetration of the intimal membrane, which allows advancement of a 0.014”-guide-wire into the true vessel lumen. The penetration depth of the needle can be selected and controlled at the handle bar of the catheter.
Interventional procedure
All recanalization procedures were carried out using a contra-lateral approach with a 7F cross-over sheath (William Cook Europe, Bjaeverskov, Denmark). After navigation of a 0.035” hydrophilic guide-wire into the subintimal space, a 4 F straight hydrophilic diagnostic catheter (Glidecath, Terumo, Tokyo, Japan) was advanced with the tip in the area of the reconstitution segment of the superficial femoral artery (Figure 2). After exchange for a long 0.014” guide-wire the catheter was removed. In patients with severe calcification, predilatations of the subintimal space with an undersized low profile balloon (Submarine, balloon diameter 4 mm, length 80 mm, Invatec, Roncadelle, Italy) were carried out to facilitate the following introduction of the Pioneer crossing device to the reconstitution segment of the vessel. After identification of the true vessel lumen by IVUS and colour-flow imaging, the catheter was rotated to bring the vessel lumen to a 12 o´clock position on the IVUS image (Figure 3). After selection of the introduction depth of the puncture needle at the handle bar of the device (usually 5 mm), the true lumen was punctured and a second long 0.014” guide-wire was advanced through the needle into the true lumen. After pulling back the needle, the catheter was retrieved. To obtain an optimal support for the rest of the procedure the 0.014” guide-wire in the true lumen was exchanged for a 0.018” guide-wire using a support catheter (3,5F Diver catheter, Invatec, Roncadelle, Italy). The final steps of the procedure included dilatation of the occluded vessel segment with an appropriately sized low-profile balloon catheter (Submarine, balloon diameter 4 to 6 mm, balloon length 80 mm) followed by implantation of self-expanding nitinol stents to stabilize the recanalized vessel segment.

Fig. 2: Preinterventional angiography showing a short chronic occlusion of the right superficial femoral artery (a). Conventional recanalization with a hydrophilic guide wire supported by a 5F multipurpose catheter failed due to subintimal passage of the wire (b). After exchange for a long 0.014” guidewire the Pioneer crossing device TransAccess catheter was introduced (c). After identification of the true vessel lumen by IVUS and colour-flow imaging, the true lumen was punctured and a second long 0.014” guide-wire was advanced through the needle into the true lumen (d). After exchange for a long 0.018” guide-wire, dilatation of the target lesion with a low profile balloon was performed (e). To stabilize the recanalized vessel segment (f), a self-expanding nitinol stent was implanted achieving an optimal procedural result (g).

Fig. 3: IVUS image showing the Pioneer crossing device TransAccess catheter (CP) in the subintimal space. Colour-flow imaging is used to identify the true vessel lumen (TL). For puncturing through the intimal membrane, the true lumen is brought to a 12 o´clock position by rotation of the catheter.
Postprocedural treatment
During intervention, all patients received 5000 units of heparin intra-arterially. Furthermore, all patients received a loading dose of clopidogrel (300 mg) immediately after stent implantation followed by a combination of clopidogrel (75 mg OD for 4 weeks) and acetylsalicylic acid (100mg OD).
Follow-up protocol
All patients underwent a clinical follow-up investigation at 1 month including colour-coded ultrasound, standardised treadmill test and recordings of ankle pressure and ankle-brachial-index (ABI) before and after exercise.
Definitions
Device success was defined as successful application of the device achieving a re-entry into the true lumen.
Procedural success was defined as successful reconstruction of the target lesion with <30% residual stenosis.
Results
In all 25 cases the Pioneer crossing device could be successfully applied to redirect the guide-wire into the true lumen by means of transmembrane puncture. In 8 cases with severe calcification of the occlusion a predilatation of the subintimal space became necessary to allow delivery of the 6.2 F catheter across the target lesion. Furthermore, there were 7 cases were multiple transmembrane puncture attempts after repositioning of the catheter were performed before finally the membrane could be penetrated. Again, this became necessary in patients with extreme calcifications of the vessel wall. There were no peri-procedural complications including perforations, embolisation or bleeding.
A procedural success could be achieved in 24 of the 25 patients (96.0%). In one case with severe calcification a residual stenosis of >50% persisted even after stent implantation and postdilatation.
Post-interventional, one patient developed a false aneurysm, which could be successfully treated by ultrasound guided thrombin injection. There were no other in hospital complications.
After 30 days, 23 of 25 patients (92.0%) were available for clinical follow up investigations. According to colour-coded ultrasound all recanalized arteries were patent without signs of recurrent stenosis. The relative walking capacity improved from 87 m to 223 m and the absolute walking capacity from 123 m to 288 m. Similarly, the mean resting ABI improved from 0.72 to 0.93 and the ABI after exercise showed an increase from 0.43 to 0.89. There were no further complications or acute re-occlusions within the 30-day period.
Discussion
Inability to achieve re-entry in the patent arterial segment distal to a superficial femoral occlusion is a frequent cause of technical failure during femoral recanalization attempts1-3. This problem can occur independently from the operator´s decision, whether he prefers an intentional subintimal or intraluminal recanalization attempt1-6. Furthermore, the potential for a subintimal passage of the occlusion with inability to re-enter the true lumen is largely independent from the occlusion length and can also complicate recanalization attempts of very short superficial femoral artery occlusions3,5-7. According to our own experience, the only independent predictor of failure to cross chronic femoral occlusions is the degree of calcification3.
So far there have been no effective strategies to facilitate re-entry into the true lumen after subintimal passage of the occlusion. Typically, extensive, time-consuming attempts with angled diagnostic catheters (e.g. vertebral shape) and stiff hydrophilic guide-wires are performed, which in a certain subset of patients will not be successful to achieve the distal re-entry8. Furthermore, these attempts may lead to a distal extension of the dissection with involvement of the first popliteal segment, which could complicate future surgical revascularization procedures.
Another option is to consider alternative interventional approaches for femoral artery recanalization. The transpopliteal approach has been described as a potentially effective salvage technique after failed cross-over or antegrade recanalization attempts3,9-11. Nevertheless, this technique requires a high patient compliance during the procedure. Furthermore, a sufficient patency of the popliteal artery and the infrapopliteal circulation is an important precondition to avoid ischemic complications related to the popliteal sheath.
The technique described in this paper offers a novel, very effective salvage technique, which in our initial experience was universally effective to redirect the guide-wire into the patent vessel segment distal to the superficial femoral artery occlusion. This way, in 25 patients, who represent 24% of all femoral recanalization attempts during this time period, a technical failure could be converted into a successful procedure. Due to the IVUS guidance, the transmembrane puncture could be reliably performed in a very controlled setting without any device-related complications.
Another important aspect is, that the application of the device allows to re-enter the true lumen immediately distal to the occluded vessel segment. This way, distal extension of the dissection into the patent vessel segment can be avoided. Furthermore, beside the time, which is required to set-up the device, there is no relevant prolongation of the procedure, which is reflected, in the average procedural time of 47 minutes.
In general, implementation of this technique into our routine cross-over recanalization technique was uncomplicated. With the use of a 7 F cross-over sheath, in all cases there was sufficient pushability and steerability of the device. Nevertheless, in case of severe calcification predilatation of the subintimal space is very helpful to facilitate advancement of the Pioneer crossing device. After redirection of the guide-wire and PTA in all cases the entire recanalized arterial segment was stabilised by implantation of self-expanding nitinol stents. This stenting strategy is based on our own observation, that recurrent stenosis seems to occur less frequently if full coverage of the lesion is achieved as compared to spot stenting. Although long-term data is not yet available for our study cohort, recent studies demonstrated favourable results for self-expanding nitinol stents12-14.
In conclusion, the Pioneer crossing device is an effective and save tool to facilitate true lumen re-entry during recanalization of total superficial femoral artery occlusions. Implementation of this device into the interventional armamentarium allows a relevant improvement of the recanalization rate of chronic superficial femoral artery occlusions.