Abstract
Background: Use of stents following angioplasty for infragenicular lesions appears to be superior to angioplasty alone. We investigated the safety and efficacy of MULTI-LINK VISION stent (Abbott Vascular, Brussels, Belgium) for the treatment of infragenicular lesions in patients with critical limb ischaemia (CLI).
Methods and results: During the period between February 2005 and October 2005, fifty patients with CLI (Rutherford 4 and 5) due to infragenicular disease were included in the study. The studied patient population included 28 males (56.0%) and 22 females (44.0%) with a mean age of 76 years (range 59-90 years). The medical history was significant for hypertension in 43 patients (86.0%), diabetes in 23 (46%) and hypercholesterolaemia in 37 (74%) patients. Fourteen patients (28%) admitted to the use of nicotine. Thirty-four (68%) belonged to Rutherford class 4 and 16 were class 5 (32%). All patients underwent clinical evaluation before and after the intervention. A pre-procedure Duplex ultrasound examination followed by angiography and intervention were performed on all patients included in the study. Sixty-two lesions were treated with angioplasty followed by insertion of 68 MULTI-LINK VISION stents. After intervention, patients were followed at one, six and 12 month intervals with clinical examination and arterial duplex study.
The survival of the studied population was 83.3%, the limb salvage was 89.3% and primary patency of treated vessel was 62.8% at 12 months.
Conclusions: Treatment of infragenicular lesions in CLI with MULTI-LINK VISION stent is safe and effective with satisfactory limb salvage. The primary patency was acceptable, but less compared to dedicated below the knee devices.
Introduction
Patients with critical limb ischaemia (CLI) present with ischaemic rest pain or with ischaemic skin lesions, either ulcers or gangrene and with either rest pain or non-healing wounds and are classified as Category 4, 5 and 6 according to the Rutherford Categorisation1, respectively. CLI patients have multi-segmental stenotic or occlusive lesions, often with involvement of the infragenicular vascular bed. Patients presenting with CLI are known to have high mortality due to cardiovascular events, and untreated CLI often leads to primary amputation1. Surgical revascularisation by bypass surgery is associated with a peri-operative mortality rate of 1.8-6% and a variable primary clinical success reported between 50%-77%2,3. The majority of patients with CLI have profound comorbid factors which preclude a major surgical intervention. In addition, absence of a suitable target vessel and/or infected soft tissues may preclude bypass surgery. Endovascular techniques, such as percutaneous transluminal angioplasty (PTA) or subintimal angioplasty, have shown promising results4,5. The BASIL trial has shown that PTA is an effective and cost-efficient alternative to traditional surgical approach in this elderly, fragile population6. The role of stents in the infragenicular lesions was limited because of lack of devices designed for this vascular bed. The stents were used selectively as a bailout following PTA for flow limiting dissections or residual stenosis7. However the results of routine stenting following an uncomplicated angioplasty were reported to be superior to PTA alone8-10. It is possible that stent implantation overcomes the early plaque remodelling and consequent loss of lumen after PTA alone.
The primary objective of this prospective, single-arm study was to evaluate the safety and clinical efficacy of MULTI-LINK VISION (Abbott Vascular) stent in the treatment of CLI due to infragenicular vessel involvement.
Methods
This prospective, non-randomised clinical trial using the MULTI-LINK VISION (Abbott Vascular) stent system for the treatment of CLI involving the infragenicular vessels was performed with institutional ethics committee approval between February 2005 and October 2005 at AZ-St Blasius hospital, Dendermonde and Imelda hospital, Bonheiden, Belgium. The inclusion and exclusion criteria are given in Table 1.
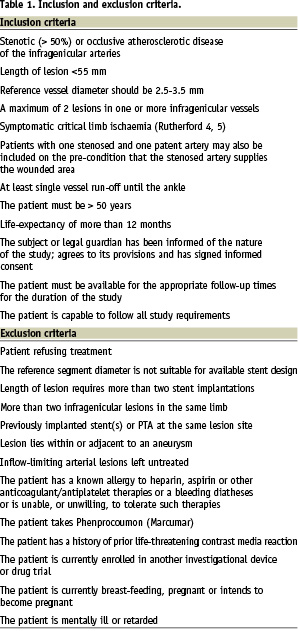
Fifty patients with CLI (Rutherford 4 and 5) and diagnosed with infragenicular occlusive arterial disease were included in the study. The studied population included 28 males (56.0%) and 22 females (44.0%) with a mean age of 76 years (range 59-90 years). The medical history was significant for hypertension in 43 patients (86.0%), diabetes in 23 (46%) and hypercholesterolaemia in 37 (74%) patients. Fourteen patients (28%) admitted to the use of nicotine. Based on the patients’ clinical description, 34 (68%) belonged to Rutherford class 4, and 16 were class 5 (32%). All patients underwent clinical evaluation, Duplex ultrasound examination and angiography. Sixty-two lesions were treated with angioplasty followed by insertion of the MULTI-LINK VISION stent.
Device description
The MULTI-LINK VISION is a pre-mounted L-605 cobalt chromium alloy (CoCr) coronary stent with radial strength and fluoroscopic visibility superior to stainless steel stents. The stents are available in 2.75, 3.00, 3.50 and 4.00 mm diameter and lengths of 8, 12, 15, 18, 23 and 28 mm.
Follow-up visits
Following intervention, according to the standard care of CLI, patients are followed at one, six and 12 months with clinical assessment, Rutherford categorisation and arterial duplex examination. Patients with clinical deterioration were referred for arteriography.
Endpoints
The primary endpoint was 12-month primary patency of the MULTI-LINK VISION stent (Abbott Vascular) in patients with stenotic or occlusive atherosclerotic disease involving the infragenicular vessels and CLI. Primary patency is defined as the absence of:
A. Any reintervention to restore the blood flow.
B. Major amputation.
C. Conversion to bypass surgery to restore the blood flow.
D. Untreated restenosis (>50%) or occlusion as determined by colour flow Duplex ultrasonography (CFDU), a haemodynamically significant restenosis (>50%) was defined as a Proximal Velocity Ratio (PVR) of > 2.4. PVR is the ratio of the Peak Systolic Velocity (PSV) at the lesion segment over the PSV at the proximal reference vessel.
The secondary endpoints of the study were:
A. Immediate angiographic procedural success, defined as maximal 30% residual stenosis on visual assessment of the treated lesion.
B. Limb salvage (defined as avoidance of a major amputation).
C. Survival of the patient.
Anticoagulation regime
Patients were given 100 mg /day of aspirin and clopidogrel 75 mg daily for four days, or one loading dose of 300 mg the day prior to the procedure. Unfractionated heparin (150 IU/Kg body weight) was given during the procedure. The post-procedure antithrombotic regimen consisted of clopidogrel 75 mg daily for at least one month and aspirin, 100 mg daily, indefinitely. Nadroparin was administered daily for three weeks.
Statistics
The statistical analysis on the follow-up data of the entire patient group was done by Kaplan-Meier estimation. All calculations were performed using the MEDCALC statistical software version 9.2.0.1.
Results
Contralateral access was the preferred approach at our institution, and this was obtained in 48 patients (96.0%). Ipsilateral access to the tibial vessels was obtained in two patients (4%) because of the presence of aortic endograft in one patient and a history of common femoral artery pseudo-aneurysm in the contralateral groin in the second. The mean procedural time was 52 min (range of 25-90 min), mean volume of contrast used was 115 ml (range of 40-250 ml) and the mean fluoroscopy time was 16 min (range of 2-47 min).
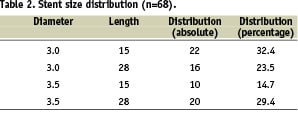
The 62 lesions treated had a mean stenosis of 92.7% (range of 50-100%). The mean lesion length was 21.1 mm (range of 5.0-52.0) and the reference diameter of the vessel was 3.1 mm (range of 2.5-3.5). Thirty-four lesions were calcified (54 .8%), seven were ulcerative (11.3%) and vessel dissection was noted in two (3.3%). Two below-the-knee popliteal (BTK P3) arteries (3.2%), 18 tibio-fibular trunks (29.0%), 10 anterior tibial (16.2%), 16 posterior tibial (25.8%) and 16 fibular arteries (25.8%) were treated successfully with a total of 68 MULTI-LINK VISION stents. The description of the stent sizes used is given in Table 2.
A predilation of the lesion was routinely performed. Twenty-three of the 62 lesions were occlusive and the remaining 39 were stenotic. The immediate procedural success was achieved in all patients (100%). As found by Kaplan Meier estimation (Figures 1-3), the survival of the studied population was 83.3%, the limb salvage was 89.3% and the primary patency of the treated vessel was 62.8% at 12 months.
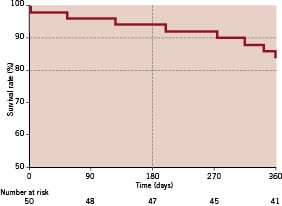
Figure 1. Kaplan-Meier estimation of survival
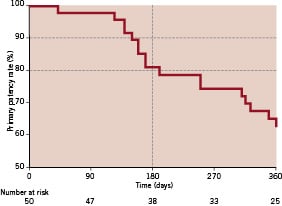
Figure 2. Kaplan-Meier estimation of primary patency
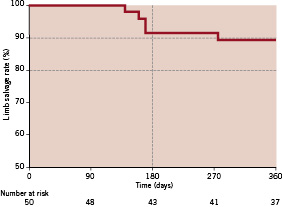
Figure 3. Kaplan-Meier estimation of limb salvage
Discussion
Critical limb ischaemia (CLI), the result of advanced, multi-segmental atherosclerotic lesions is one of the major causes of morbidity and mortality in the increasing elderly population. The increasing incidence of diabetes in the general population is also a major contributing factor for this epidemic of CLI. Despite the advances made in the treatment strategies of CLI, the management of this subset of patients is still a difficult task.
CLI manifests with rest pain, ulceration and gangrene of the lower extremity and affects 500-1000 individuals per million population every year with a significant economic impact on health care resources1. The mortality rate amongst these patients is 25% in one year5 and more than 50% in 3 years1,11. Untreated CLI often results in a primary major amputation, with markedly diminished quality-of-life and emotional stress to the patient and the family. Moreover, it translates into high costs to the society12,13. Many studies have shown significant improvement in the functional status and quality-of-life in patients with limb salvage by revascularisation rather than primary amputation14. Revascularisation is also more cost-effective than primary amputation in patients with critical ischaemia15. Improved survival rate is noted after revascularisation by distal bypass surgery as compared to primary amputation16,17 and current data unequivocally supports aggressive revascularisation of critically ischaemic limbs18.
Many investigators recommend that in patients with CLI and concomitant infragenicular lesions, the endovascular strategy should be considered first, prior to surgery10,19,20. The goal of any intervention is to achieve an in-line pulsatile flow of blood to the ischaemic region. The endovascular intervention has shown to be an effective tool10,19-21 for CLI with reduced mortality6,22, hospital stay22 and costs6,22 compared to bypass surgery. Moreover, a failed angioplasty does not preclude surgical revascularisation6,10,22 at a later time.
Although the reported high clinical and technical success23-25 of endovascular infragenicular strategies, the BASIL trial documented high immediate failure and re-intervention in a 12 month follow-up for angioplasty group compared to bypass surgery6. The infragenicular vessels are of smaller calibre and the atherosclerotic process involving these is often diffuse and multi-segmental9. Angioplasty and stenting may achieve superior outcome compared to angioplasty without stenting9,26 in this hostile vascular bed. However the restenosis rate following angioplasty and stenting may be more than 50% after 12 months1. To overcome this, and to improve the primary patency rate, drug eluting stents and stents of different material were studied by several investigators. Improved patency rates were reported for sirolimus-eluting stents27,28, absorbable metal stents29 and nitinol stents30.
In an earlier publication of our group10, we reported on our global experience using all the available, different endovascular tools, including the above mentioned newer generation devices, and found at 12 months a limb salvage rate of 96.6%. This result is comparable to the 89.3% limb salvage rate with the bare metal MULTI-LINK VISION stent as found in the present study. However, the MULTLINK VISION stent’s primary patency rate of 62.8% at 12 months is inferior to this in our earlier global publication (74.2%) and other published reports of dedicated last generation below the knee stents27-30, but is still better compared to PTA alone.
Endovascular management will become the primary modality of treatment in patients with CLI due to infragenicular disease. Development in the field of endovascular techniques and devices will certainly further improve the patency rates of the infragenicular interventions and achieve higher clinical success rates in this subset of fragile patients.
Study limitations
This is a prospective, non-randomised study limited to two centres and with a small number of patients. The other limitation was that the patency of the device was determined by Duplex ultrasound examination rather than the conventional angiography. Recently after the finalisation of the follow-up, Favaretta et al brought to light that Duplex ultrasound has only limited value for the investigation of infragenicular lesions31. Therefore, any future investigation into the efficacy of the MULIT-LINK VISION stent – or any other endovascular device for infragenicular revascularisation – should be controlled by means of an angiographic control rather than a Duplex ultrasound examination.
Conclusion
The MULTI-LINK VISION stent is a safe device for the management of CLI due to infragenicular lesions. The 12 month limb salvage rate was comparable to the published reports on dedicated below the knee devices. Although better then what was seen with PTA alone, the primary patency seems to be lower when compared to other dedicated below the knee stent types.
Acknowledgement
The authors take great pleasure in thanking the staff of Flanders Medical Research Program (www.fmrp.be), with special regards to Koen De Meester and Erwin Vinck, for performing the systematic review of the literature as well as providing substantial support for the data analysis and writing of this article.

