Abstract
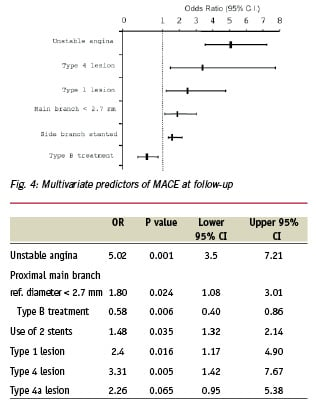
Objectives: The purpose of this study was to analyze from a large prospective database started in 1996, the immediate and mid term results of coronary bifurcation stenting using bare metal stents. Background: Stenting of bifurcation lesions remains a challenging subset. Various approaches have been advocated and no large prospective studies are available on this subject. Methods: Between 1996 and 2002, data were prospectively collected on all patients with bifurcation lesions treated with coronary stenting in our institution. Seven-month follow-up data were obtained in 96.7% of patients and coronary angiogram was performed in the presence of clinical or stress test ischemia. The database was analyzed to extract uni-variate and multivariate predictors of acute and 7 months adverse events. Results: A total of 1,149 patients were included, median age 65 years, 19% diabetic patients, unstable angina in 37.3% of cases and acute MI 10.5%. The target was the LAD-diagonal bifurcation in 53.2% of cases. Angiographic success (residual stenosis < 30%) was obtained in 96.3% of cases for the main branch (MB) and side branch (SB) 92.9 % (residual stenosis < 50%). The in-hospital MACE rate was 4.6 %. At seven months follow-up, a total MACE rate of 18.1% was observed including a target vessel revascularization rate of 13.2% and death rate of 1.6%. By multivariate analysis, independent predictors of MACE at seven month follow-up were unstable angina (OR 5.02 , p = 0.001, 95 % CI : 3.5 - 7.2), type 4 lesion (OR 3.31, p = 0.005, 95 % CI : 1.4 - 7.7), a MB < 2.7 mm (OR 1.8, p = 0.024, 95 % CI : 1.08 - 3.01), non use of a provisional T stenting strategy for the SB (OR 0.48, p = 0.006, 95 % CI : 0.40 - 0.86), and SB stenting (OR 1.48, p = 0.035, 95 % CI : 1.32 - 2.14). Conclusion: Provisional T stenting strategy applied to the SB is a predictor of favourable outcome after coronary bifurcation stenting using bare metal stents. It significantly reduces the rate of MACE as well as the need for repeat TVR at 7-month follow-up.
ABBREVIATIONS AND ACRONYMS
ACS: acute coronary syndrome
DES: drug-eluting-stents
CABG: coronary artery bypass grafting
MACE: major adverse cardiovascular events
MI: myocardial infarction
MLD: minimum luminal diameter
NQMI: non-Q wave myocardial infarction
QCA: quantitative coronary angiography
Treatment of patients presenting with lesions located in large bifurcation lesions remained for a long time the domain of cardiac bypass surgery. However, the numerous improvements in catheter-based interventions coupled with enhanced operator expertise has led to a widening of indications to increasingly complex settings. Nevertheless, lesions at coronary bifurcations pose a real challenge to the interventional cardiologist. Plain old balloon angioplasty was associated with low procedural success and high restenosis rates1-10 compared to non bifurcation lesions. Stenting has dramatically reduced the restenosis rate for standard lesions11-12, but the treatment of coronary bifurcations using stents has remained difficult with controversial approaches and less favourable outcomes13-17.
When starting this prospective registry in 1996, we proposed a classification of bifurcation lesion types and treatments in an attempt to render comparison and inter-observer discussion easier18. In parallel, we undertook an evaluation of various bifurcation techniques and of all the stents that were being developed and marketed, by means of a bench test. Both classifications are summarized in Figures 1 and 2.
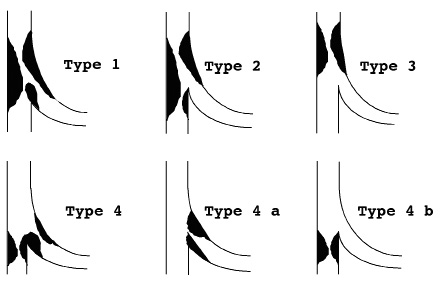
Fig. 1: Classification of coronary bifurcation lesions
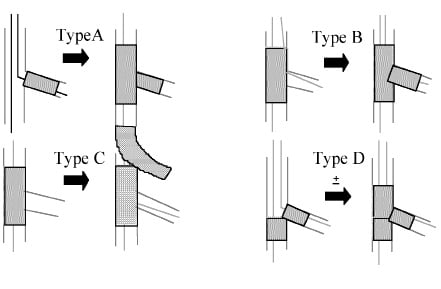
Fig. 2: Classification of coronary bifurcation treatment
This assessment enabled us to discover that certain approaches such as ‘Culotte stenting’ or “modified T stenting” techniques resulted in an excess of metal in the main branch and that the accumulated layers of metal thus created were not completely smoothed out by kissing balloon inflation (Kissing). In addition, we observed that opening a strut of the main branch stent towards the side branch ostium resulted in simultaneous deformation and displacement of the stent by causing it to stretch out, and that Kissing was required in order to re-apposition the stent against the main branch wall. Analysis of our bench test results confirmed that stents used in bifurcation lesions must allow good scaffolding of the main branch and adequate opening of the struts towards the side branch whilst providing sufficient coverage of the ostium. In this respect, tubular stents seemed particularly adapted. This registry includes procedural, in-hospital clinical outcomes, systematic seven month clinical follow-up and angiographic follow up in patients with symptomatic or documented ischemia.
Methods
Study population
A total of 1,149 consecutive patients with de-novo coronary bifurcation lesions, defined in the ICPS classification as types 1, 2, 3, 4, 4a and 4b18 and treated by coronary stenting were included in the registry. Patient demographics as well as procedural data were collected. Using the General Electric software for quantitative coronary angiography (QCA), reference vessel diameter, minimum luminal diameter (MLD) and percentage diameter stenosis were measured pre and post angioplasty for the main vessel and the side branch. Cardiogenic shock was the only exclusion criterion.
Interventional procedure
All patients had a bolus of 80 units/Kg of heparin with a target ACT of 300 seconds 5 minutes later and an additional bolus of heparin when necessary. In case of Gp2b3a inhibitors usage, the target ACT was 250 sec. The strategy of bifurcation lesion stenting18 was left to the operator’s choice. However, during the period when the registry was conducted, type B treatment progressively became the most frequently implemented strategy in view of the results achieved. It consisted of wiring both branches, stenting the parent vessel while leaving a wire ‘jailed’ in the side branch, then performing guide wire exchange and final Kissing balloon inflation with provisional T stenting of the side branch. Side branch stenting decision was also left to the operator’s discretion. However, in most instances the side branch was systematically stented when the length of the SB lesion was >3-5 mm or in the presence of a significant residual lesion (> 30% by visual assessment) and / or significant dissection associated with a risk of residual ischemia or occlusion. Other treatment strategies employed were type A: T stenting with initial side branch stenting followed by main branch stenting and kissing balloon inflation
This treatment was widely used during the early years of the registry, especially in instances when access to the side branch was difficult, generally because of a T-shape angulation between the two branches. However, the realisation that the jailed wire technique could favourably modify the angle between the two branches progressively led the operator to adopt type B treatment which obviates the need for systematic stenting of the two branches. Type C treatment, also known as Culotte stenting, was rapidly discarded and type D treatment (kissing or touching stent deployment) was only used on rare occasions. Predilatation of one or both branches of the bifurcation was almost systematically performed between 1996 and 1998. It has become decreasingly used especially in patients with acute coronary syndromes in order to reduce the risk of distal embolisation. Over the years, predilatation of the side branch has ceased to be performed because it may further complicate the access to the side branch through the struts of the main branch stent in the case of side branch dissection when Type B treatment is used.
All patients were treated with Ticlopidine or Clopidogrel in association with aspirin 75 mg daily for at least one month and they had a prospective 7 month clinical follow-up with 6 month stress test and coronary angiogram in case of angina or ischemia.
Definitions and endpoints
Patients were defined as post MI when the bifurcation lesion (culprit lesion or not) was treated within one month after the onset of MI. Lesion type were defined by QCA according to our previous definition18, including lesions with a significant side branch > 2 mm in diameter. Lesion angulation was measured at baseline in the working view which was the view providing the best side branch ostium visualisation, by measuring the distal angle between the side branch and the main branch vessel distal to the bifurcation. When angulation was < 70°, bifurcation lesion was defined as Y shape. Angiographic success in the treatment of bifurcation lesions was defined as a < 30% residual stenosis (stenting era and 5 mm edges) in the main branch and < 50 % in the side branch by QCA. Acute thrombosis was defined as the occurrence of acute closure of the target vessel less than 24 hours after the index procedure; subacute thrombosis was defined as the occurrence of acute closure of the target vessel after 24 hours but less than one month and late thrombosis as the occurrence of acute closure at least one month after the index procedure. MACE were defined in a hierarchical order as the occurrence of death, Q- or non-Q-wave MI, or target vessel revascularization (TVR). CPK were measured in all cases 24 hours after the index procedure or more in cases of chest pain. Non Q-wave-MI was defined as a CPK level > 3 times the normal value without occurrence of a Q wave. Q-wave MI was defined as a CPK level > 3 times the normal value and/or occurrence of a new Q wave on EKG at follow-up. TVR was defined as the need for re-intervention in the treated vessel using either PCI or CABG. These data were analyzed at hospital discharge and at seven month follow-up (cumulative).
Statistical analysis
Data are expressed as mean and standard deviation or median and quartiles when appropriate. The association between MACE or TVR and qualitative variables was analyzed using chi square or Fischer’s exact test as appropriate. Odds ratios (OR) and 95% confidence methods were calculated to assess predictive value. The association between quantitative variables and MACE or TVR was analysed using Mann-Whitney tests. A P value <0.05 was considered significant. All parameters significantly associated with MACE or TVR at seven months were included in a multivariate logistic regression analysis for the determination of independent parameters associated with Death or MI, TVR and MACE.
RESULTS
Demographics
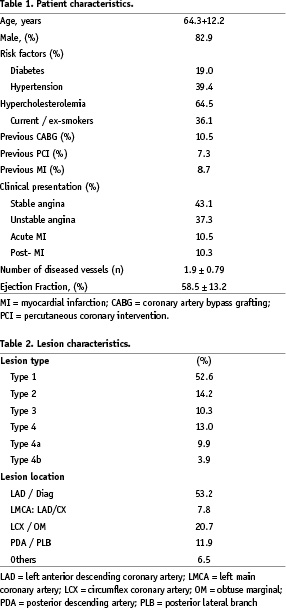
The main characteristics of the patients are summarised in Table 1. The median age was 65 (55 - 73) and 19.0% had diabetes mellitus; 37.3% had unstable angina and 10.5% acute MI.
Vessel and lesion characteristics. The left anterior descending /diagonal bifurcation was the target in the majority of cases (53.2 %) and the lesion was type 1 or 4 ICPS classification in 65.6% of cases (Table 2). The baseline reference vessel diameters of the main branch proximally and distally were 3.1 [2.8 - 3.5] mm and 2.8 [2.4 - 3.1] mm and side branch 2.3 [2.0 - 2.6] mm. The majority of lesions (79.9%) had a Y shape angulation.
Procedural characteristics
This is summarised in Table 3. The main branch was stented in 98.6% of cases and the side branch in 37.2%. Tubular stents were used in 87.4% of cases and final Kissing was performed in 84.5% of cases. Type B treatment was the most widely implemented strategy (73.7%) with the side branch being stented in 25.6% of the cases. Type A treatment was used in 18.3%, Type C in 1.9% and Type D treatment in 6% of cases. Angiographic success of the main branch was obtained in 96.3% of cases and both branches in 92.9%.
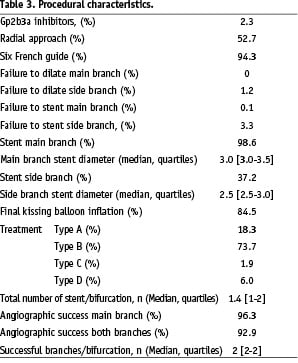
In hospital outcome
Acute occlusion occurred in 0.5% and sub-acute thrombosis in 1.2% of cases. Urgent revascularisation was performed by PCI in 1.4% and emergency CABG in 0.4%. Access site complications were observed in 0.3% of patients, requiring transfusion in 0.3% and vascular surgery in 0.2%. Mean hospital stay was 2.9+3.0 days. Q-wave MI occurred in 0.6%, non-Q wave MI in 2.8%, and death in 0.4%. The total in-hospital MACE rate was 4.6%. These data are summarised in a hierarchical order in Table 4.
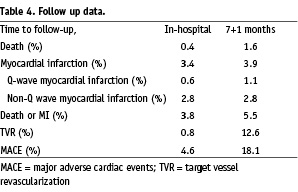
Seven month follow-up
Clinical follow-up was obtained in 96.7% of patients at 7+1 months. A cumulative death rate of 1.6% was observed and the combined endpoint of death and MI (Q wave and non-Q-wave) was 5.5%. The need for TVR was 13.2% (including CABG in 2.7%) with a total MACE rate of 18.1%. Follow-up events are summarised in a hierarchical order in Table 4.
Univariate predictors of adverse events
By univariate analysis, predictors of death at follow-up were left main bifurcation (4.3 %, P = 0.02), diabetes mellitus (3 %, P = 0.007) and non use of Type B treatment (4%, P = 0.01). There was only one predictor of irreversible events (death, MI or CABG) at 7 month follow-up: non use of type B treatment compared to other treatment types: OR 0.53, CI 0.31-0.90 (p=0.018). The relationship between irreversible events and the type of treatment used was as follows: type B, 4.5 %; type A, 5.9%; type D, 10.6% and type C treatment, 28.6%.
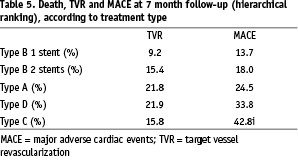
A relation between TVR and lesion type was also observed. The lowest rate of TVR was found in type 3 lesions (8.3%), P = 0.008 compared to the highest in type 4 lesions (22.1%) and a relation was also evidenced between treatment type and TVR (Table 5). The lowest rate of TVR was reported in patients treated with the provisional T stenting strategy. When type B treatment (provisional T stenting) was applied without stent placement in the side branch, TVR was 9.2%; it increased to 15.4% when the side branch was stented. (p=0.009). Type A treatment (systematic T stenting) was associated with a TVR rate of 21.8%.
Univariate predictors of MACE were unstable angina (18.9 vs 16.4%), period 1996-98 compared to period 1999-2002 (22.1 vs 14.8%), proximal main branch reference diameter < 2.7 mm (21.1 vs 17.0% ), type D treatment compared to type B treatment (35.3 vs 14.0%) and use of 2 stents (24.1 vs 13.6%) as shown in Figure 3. MACE rate was also influenced by lesion type. The lowest rate of MACE was observed in type 3 lesions and the highest in type 4 lesions (28.3 vs 8.8%).
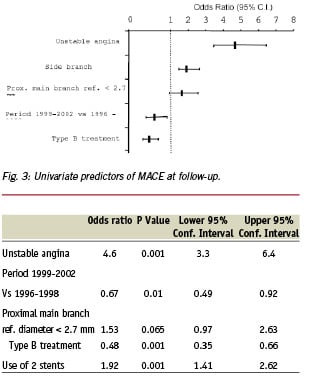
Multivariate analysis
By multivariate analysis only unstable angina (OR 1.77, CI 1.04-2.99; p=0.034) and non use of type B treatment (OR 0.55, CI 0.32-0.95, p=0.03) were found as independent predictors of death or MI. Independent predictors of TVR were unstable angina (OR 6.74, CI 4.66-9.88; p<0.001), proximal main branch reference diameter < 2.7 mm (OR 2.03, CI 1.22-2.28; p=0.006) and non use of Type B treatment (OR 0.46, CI 0.31-0.67; p<0.001). Predictors of MACE at follow-up are shown in Figure 4.
Discussion
The rare published studies reporting the results of PCI with stenting in bifurcation lesions16,19-25 were conducted with inhomogeneous techniques and were characterized by relatively high restenosis and event rates. In a study of 54 bifurcation lesions with angiographic follow-up, Sheiban et al.26 reported a 42% restenosis rate in the main branch and 47% in the side branch leading to a 61% target site restenosis rate. In their retrospective analysis of a series of 131 bifurcation lesions treated by PCI and stent Al suwaidi et al.20 showed a one year event free survival rate of 69.6% in patients treated by T stenting and 13.7% in patients treated with the “culotte” technique (type C treatment).
Over a period of seven years, we have had the opportunity to evaluate the predictors of outcome in a large single center registry of 1,149 bifurcation lesions. Not surprisingly, the presence of acute coronary syndromes was predictive of higher MACE rates as was a proximal main branch reference diameter < 2.7mm. Findings from this registry also confirmed that the technique and strategy of stent implantation play a definite role in the outcome. Al Suwaidi et al.20 have shown that the strategy of provisional T stenting was associated with a 26.8% event rate at one year in patients treated with only one stent in the main branch and balloon angioplasty in the side branch vs. 47.7%, when T stenting was used with 2 stents (p<0.05). Similarly, data analysis of our registry showed that stent implantation in both branches of the bifurcation whether systematic (type A treatment) or provisional (type B treatment) was associated with a higher need for TVR at 7 months compared to implantation of a single stent. Though the less favourable outcome observed in the double stenting group may be explained by the presence of more complex lesions, this tends to show that the provisional T stenting strategy should be encouraged. In a previous report18, we demonstrated that the strategy of final kissing balloon inflation and the placement of a tubular stent in the main branch were predictive of favourable long-term outcome. In the series reported here, another technical predictor of improved outcome was evidenced, namely, the use of provisional T stenting (Treatment B) which resulted in a significant reduction in MACE and TVR rates at 7 months. This strategy of provisional T stenting using the Bestent was previously shown in a prospective dual center study (27) to be associated with a low rate of MACE (14.6%) including a TVR of 9.4% at 6 month follow-up. In view of the above, the type of treatment chosen would appear to be a powerful predictor of outcome.
The question has been raised as to whether the use of sirolimus eluting stents will solve all technical issues. In the sirolimus bifurcation study recently published by Colombo et al.28 in which 85 patients were randomised for a strategy of systematic T stenting or provisional T stenting, there were 4 (6.1%) cases of restenosis in the main branch and 14 (21.2%) cases of restenosis in the side branch. Side branch restenosis was more frequent in the double stenting group (11 cases) than in the single stenting group (3 cases). These results clearly show that drug-eluting stents are not the ultimate solution to the problem of bifurcation lesion treatment and that technical issues remain to be appropriately addressed.
Study limitations
There are several limitations to our study. This single center non randomised registry may induce a bias by favouring a strategy considered as preferable by the operators. Indeed, two specific techniques (Culotte and Crush) were seldom or never used. On the other hand, it reflects an historical evolution of strategies influenced by bench testing as well as interactions and discussion between all members of our team. No systematic follow-up angiography was performed, which results in an underestimation of the true restenosis rate. However, the clinical follow-up data collection was very carefully performed and is representative of patient management in real life, and the strength of this registry lies is in the large sample size.
Conclusions
This study shows that bare metal stents can be deployed in bifurcation lesions with high procedural success and acceptable MACE rates at 7 months. In this respect, we have shown that stenting of the main branch followed by kissing balloon inflation and provisional T stenting of the side branch when necessary is the strategy associated with the most acceptable acute and mid-term results when using workhorse stents. This optimal strategy could be applied in the current era of drug-eluting stents and preliminary data are very promising. The high incidence of bifurcation lesions in a daily practice calls for the development of user-friendly dedicated stents.
Acknowledgments
The authors would like to thank Mrs. Corine Henot for collection and data entry and Mrs Catherine Dupic for her assistance in the preparation of the manuscript.